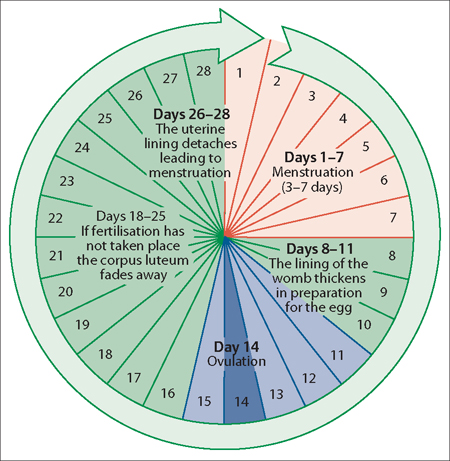
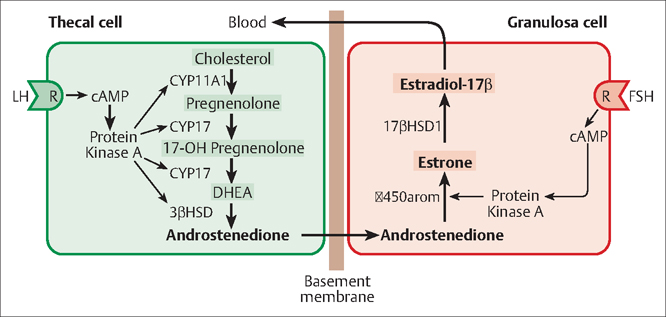
4 The Menstrual Cycle and Fertilization Arnon Wiznitzer Menarche is often considered to be the central event of female puberty. The age of onset of menarche is variable, and ranges between 9.1 and 17.7 years with a mean of almost 13 years. The events that initiate puberty are still unknown. However, adrenal steroids and melatonin are probable initiators of these events. Maturation at puberty probably involves changes in the hypothalamus that are independent of ovarian steroids. An orderly sequence of events follows the maturational changes in the hypothalamus, which includes an increased secretion and response to gonadotropin-releasing hormone (GnRH). This, in turn, leads to an increased production and secretion of gonadotropins, which are responsible for follicular growth and development in the ovary and increased sex steroid levels. This series of events leads finally to the monthly cycle of hormone production and simultaneous proliferation of the uterine lining to prepare for possible fertilization of the ovum and implantation of the embryoa process known as the “menstrual cycle.” To facilitate understanding in this chapter, discussion of the menstrual cycle is divided between cyclic changes that occur in ovary and the uterus. There is also a brief discussion of the process of fertilization. Amenorrhea: The absence of menstrual bleeding is known as amenorrhea. Follicular atresia: This is the process by which a primary follicle or a tertiary follicle stops growing, leading to disappearance (apoptosis) of its follicle cells and the oocyte, or egg, they contain. Such a follicle is called an atretic follicle. Gamete: This term refers to a mature sexual reproductive cell having a single set of unpaired chromosomes. Gametocyte: This describes an immature animal or plant cell that develops into a gamete by meiosis. Hypophysis: This is a term for the pituitary gland. The anterior lobe is sometimes identified as the adenohypophysis and the posterior lobe as the neurohypophysis. Menarche: The time in a girl’s life when menstruation first begins is known as menarche. During the menarche period, menstruation may be irregular and unpredictable. Mood, weight, activity level, and growth rate may fluctuate with the hormone levels. This term is often used synonymously with female puberty. Menses: This refers to the monthly flow of blood from the genital tract of a woman. Menorrhea: This term describes the normal discharge of the menses. Oocyte: A female gametocyte that develops into an ovum after two meiotic divisions is known as an oocyte. Oogonia: This term describes a descendant of a primordial germ cell that gives rise to oocytes. Pubarche: This is a term for the beginning of puberty marked by the first appearance of pubic hair in the genital region. Puberty: This is the process of physical changes by which a child’s body becomes capable of reproduction. Puberty is initiated by hormone signals from the brain to the gonads (the ovaries and testes). In response, the gonads produce a variety of hormones that stimulate the growth, function, or transformation of brain, bones, muscle, skin, breasts, and reproductive organs. Thelarche: The start of breast development in a woman at the beginning of puberty is known as thelarche. The menstrual cycle can be divided into three phases: Follicular development is a dynamic process designed to allow the monthly recruitment of a cohort of follicles, and the selection of one dominant follicle that will release a single mature oocyte each month. In humans, the average length of the follicular phase ranges from 10 to 14 days (Fig. 4.1), and variability in this length is responsible for most of the variation in total cycle length. The follicular phase initiates at the first day of the menses. At this time the levels of gonadal steroids are low, and with the demise of the corpus luteum follicle-stimulating hormone (FSH) levels begin to rise recruiting a cohort of follicles. In response to FSH, the follicles initiate the secretion of estrogen, which increases through the follicular phase and is responsible for endometrial growth. The rise in estrogen exerts a negative feedback on FSH at the hypophysis (pituitary gland) level. In addition, the growing follicles produce inhibin B, which also suppresses FSH secretion by the pituitary. Conversely, the rise in estrogen levels at the beginning of the cycle produces a negative effect on the secretion of luteinizing hormone (LH), but late in the follicular phase LH levels increase dramatically. Fig. 4.1 A diagram of the menstrual cycle The follicular phase constitutes the period beginning with menstruation and ending at ovulation, which is approximately 14 days in most women. During the follicular phase, hormonal feedback promotes the orderly development of a single dominant follicle, which is destined to ovulate from a period of initial growth of a primordial follicle through the stages of the preantral, antral, and preovulatory follicular growth (Fig. 4.2). This phase corresponds to the proliferative phase in the uterus, in which there is building of the endometrial lining. In the middle of the follicular phase of menstrual cycle, after growth of a follicle has been achieved, local concentrations of prostaglandins and proteolytic enzymes induce the extrusion of the oocyte through the follicular wall, and ovulation occurs. After ovulation, the menstrual cycle enters the luteal phase, the ruptured follicle becomes the corpus luteum and secretion of both progesterone and estrogen provide the adequate environment for the fertilized oocyte to implant in the endometrium. This phase corresponds to the secretory phase in the uterus. If fertilization occurs, the secretion of human chorionic gonadotropin (HCG) by the embryo rescues the corpus luteum, allowing the continued secretion of progesterone and estrogen to sustain the pregnancy. If fertilization does not occur, the corpus luteum dies, which causes a drop in progesterone and estrogen levels and eventual shedding of the endometrium (menses). Most oogonia are lost during fetal development, and the remaining follicles are recruited during the reproductive years until menopause occurs, in which the oocyte reserve is depleted. During fetal development, the oogonia are arrested at the diplotene stage of the prophase in the first meiosis, the germ-cell process of reduction division. At this stage, a single layer of 8 to 10 granulosa cells surrounds the oogonia to form the primordial follicle. Those oogonia that fail to be properly surrounded by granulosa cells undergo atresia. When the developing oogonia begin to enter the meiotic prophase I, they are known as primary follicles (Fig. 4.3), or oocytes, and remain arrested in this phase, until the time of ovulation, by a probable stasis mechanism involving an oocyte maturation inhibitor (OMI) produced by granulosa cells. It is believed that the inhibitory action of this substance is achieved via gap junctions connecting the oocyte to its surrounding granulosa cells. When the LH surge at midcycle occurs, the gap junctions are disrupted, and the connection between the oocyte and granulosa cells is interrupted, allowing meiosis I to resume. Fig. 4.2 Folliculogenesis and the classes of growing follicles in the human ovary The early stages of folliculogenesis proceed very slowly, and it has been estimated that in humans the process can take more than 300 days Even in the preantral stage (class 1), many growing follicles fail to survive, and degenerate through a process termed follicular atresia Growing follicles enter class 2 usually in the late luteal phase, class 3 between late luteal and early follicular phases, class 4 during late follicular phase, and become recruitable class 5 follicles during late luteal phase. Fig. 4.3 The life cycle of a follicle In each cycle there is growth of a cohort of oocytes. The initial recruitment and growth of the primordial follicles is independent of gonadotropin and affects a cohort over several months. The factor(s) responsible for the recruitment in each cycle is unknown. After initial recruitment, control of follicular growth and differentiation shifts from gonad-otropin-independent to gonadotropin-dependent growth, presumably by FSH. The action of FSH promotes growth of the oocyte and expansion of the granulosa cells (Fig. 4.4) from a single layer to a multilayer of cuboidal cells. Fig. 4.4 A human oocyte with surrounding granulosa cells, after aspiration. Driven by the stimulus of FSH, the zona pellucid, a glycoprotein-rich substance, is formed, which separates the oocyte from the surrounding granulosa cells. Simultaneously with the proliferation of granulosa cells, there is proliferation of theca cells in the stroma bordering the granulosa. Both granulosa and theca cells function synergistically to produce estrogen, which is then secreted into the circulation. One of the follicles attains dominance over the rest of the cohort, which undergo atresia. The mechanism for selection of the dominant follicle is still not clear, but follicular development can be explained by the “two-cell, two-gonadotropin theory,” which states that during follicle development, steroid hormone synthesis takes place in a compartmentalized manner (Fig. 4.5). According to the two-cell theory, estrogen is produced in the granulosa cell by aromatization of androgens; the activity of the enzyme (aromatase) that catalyzes this reaction is enhanced by FSH stimulation of specific receptors on these cells. Fig. 4.5
Definitions
The Menstrual Cycle
Follicular Phase
Ovarian Follicular Development
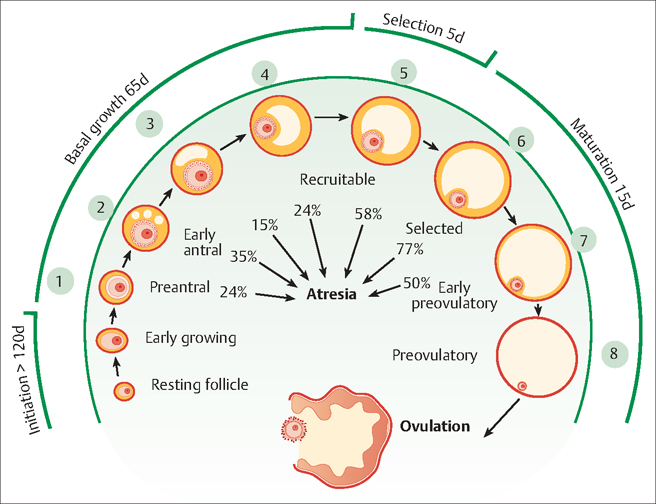
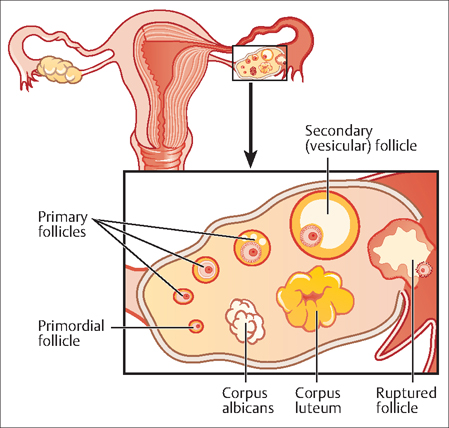
Primordial Follicles
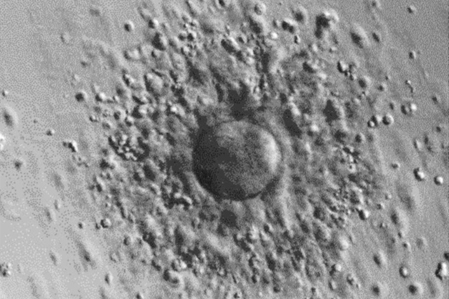
Preantral Follicle
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


