The Febrile Child
M. Douglas Baker and Jeffrey R. Avner
Although fever is almost always a sign of an underlying illness, many parents and patients consider it to be a serious disorder that requires immediate relief. Accordingly, fever is often a cause of great consternation for parents and is one of the most common reasons for children to visit a physician. Fever is a primitive, almost universal component of the acute phase response to illness. As such, it may result from virtually any process associated with inflammation or, more specifically, with cytokine release, including malignancies, immunologic reactions, and trauma (see Chapters 121 and 227 for a detailed discussion on thermoregulation and the genesis of the febrile response). In children, fever is most frequently a manifestation of an infectious illness (see Chapter 227), usually of benign prognosis, such as a limited viral illness or a localized bacterial infection. On occasion, however, fever may be the only clinically detectable sign of serious infection, a concern that is particularly relevant in patients whose immunologic defenses are reduced. Therefore, the appearance of fever as a lone manifestation of illness always demands a logical and careful approach to evaluating the underlying cause.
DEFINITION OF FEVER
Body temperature, even during the febrile response, follows a diurnal variation, with a nadir in the early morning and a peak in the early evening, and is influenced both by environmental circumstances and by the place where it is measured in the body. Core body temperature, the operating temperature of the tissues in vital organs (often estimated from temperature probes in the great vessels or the thoracic esophagus), is not practically accessible under most clinical conditions. Thus, families and clinicians usually rely upon measurements taken from the body surface (skin of the axilla or the forehead) or from accessible body cavities such as the mouth, the ear canal, or the rectum. In interpreting the results, it is important to remember that these measurements only reflect core temperature to the extent that the tissues from which they are obtained maintain a rich blood flow. Any decrease in perfusion of the skin or the mucous membranes lining the cavities where the measurement is obtained will result in an underestimation of core temperature. Many pediatricians define fever as a rectal temperature measurement of 38°C or greater, obtained with a reliable measurement tool, such as an electronic or glass and mercury thermometer.1
Illnesses associated with fever are particularly common in the first few years of life. Children younger than 3 years of age and especially young infants are at greater risk of suffering from a serious infection because of their limited immunologic repertoire and the frequent lack of localizing signs (see Chapter 227 for a discussion on common pathogens).
CLINICAL ASSESSMENT OF ACUTE FEVER
The management of the child with acute fever is discussed in Chapter 227. Management of the child with chronic fever of unknown origin is discussed in Chapter 228, and of fever in the immunocompromised child in Chapter 229. An algorithm for the management of infants and children with acute fever is shown in Figure 227-1.
 INFANT LESS THAN 3 MONTHS OF AGE
INFANT LESS THAN 3 MONTHS OF AGE
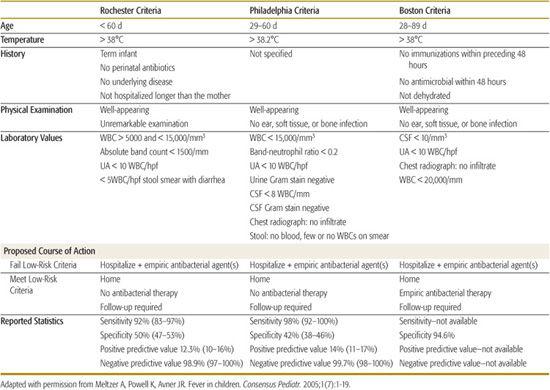
Traditionally, the majority of clinicians in the United States investigated aggressively any infant who presented with fever before 2 to 3 months of age,2 including a broad laboratory investigation for bacterial disease, hospitalization, and empirical parenteral administration of antibiotics. In the 1990s, this approach became tempered by a series of large clinical studies3,4 that established new screening tools to identify febrile infants at low risk of having a serious bacterial infection (Table 105-1). Of the three screening tools developed,3,5,6 the model created at the Children’s Hospital of Philadelphia5 was the most conservative and had the highest negative predictive value.
The application of screening tools has diminished the number of febrile infants who are admitted to the hospital or who leave the emergency room with antibiotics. However, the approach to managing fever in the young infant is far from uniform, and many pediatric practitioners continue to rely on long-established personal practices.7
A few principles are well accepted. In the presence of fever, the clinician should conduct a thorough history and physical examination, including an assessment of well or ill appearance. The latter must prompt aggressive investigation for possible bacterial infection and empirical administration of antibiotics as an inpatient regardless of initial results of diagnostic tests.
Well appearance, while reassuring, does not necessarily indicate absence of bacterial disease. Even when validated objective criteria for clinical appearance are applied,8 many senior, experienced clinicians will describe infants who have culture-proven serious bacterial infections as appearing well.
Diagnostic Testing
The minimum diagnostic testing for evaluating fever in young infants consists of a complete blood count with differential, blood culture, urinalysis with microscopy, urine culture, and usually spinal fluid analysis and culture. To minimize contamination, the urine sample should be obtained via urine catheterization or bladder puncture, and not by bag collection.9
A lumbar puncture is indicated in febrile infants less than 1 month of age and in any ill-appearing older infants. Performing a lumbar puncture in well-appearing febrile infants who are 1 to 2 months of age has become a source of debate over the past few years. Some studies suggest that lumbar puncture can be delayed or omitted provided that the infant meets all low-risk clinical and laboratory criteria and that the parents are reliable observers and have appropriate follow-up skills.7 However, recent data has shown that 40% of infants with bacterial meningitis had total white blood cell counts in the usually acceptable range (5000–15,000), so this was not a reliable predictor of absence of bacterial meningitis.1 In another study of the performance of clinical criteria for infants at very low risk of bacterial meningitis, all failures of the tool to predict absence of bacterial meningitis involved infants younger than 2 months of age.10
Table 105-1. Defining Low-Risk Criteria for the Management of Febrile Infants
The necessity of obtaining a chest radiograph in every infant with fever is also a debatable issue. Several clinical studies have shown that the chest film has a low yield in those infants who do not have specific signs of respiratory disease.11
The use of acute phase reactants such as C-reactive protein (CRP) and procalcitonin (PCT) as predictors of bacterial infection has come into vogue in recent years.4,12 Both CRP and PCT are produced by the liver in response to cytokines like tumor necrosis factor alpha and interleukin-6. Their values increase 3 to 4 and 4 to 6 hours, respectively and peak within hours after the onset of fever. While valuable as a screening tool, none of these acute phase reactants is reliable as a sole predictor of bacterial infection.
It is a widely held concept that children develop acute illnesses as single and distinct events, one at a time. Reports of some groups of infants, such as those with clinical bronchiolitis (defined as presence of fever and wheezing), cite very low rates of concurrent bacterial infection.13 However, rapid testing and identification of viral agents is not useful to rule out the possibility of bacterial infection since evidence suggests that young infants can test positive for two infecting agents at the same time. During the past two decades, studies of large cohorts of febrile infants and preschool-age children have consistently demonstrated that 6% to 7% will test positive for the simultaneous presence of viral and bacterial pathogens.14,15 This is true of infants with documented respiratory syncytial virus infections16 and with other common viral infections.17 In infants who have documented viral disease, the most common location for simultaneous bacterial infection is the urinary tract. However, bacteremia occurs in approximately 1% of infants who test positive for the presence of common viruses.
 INFANTS AND YOUNG CHILDREN (3 TO 36 MONTHS OF AGE)
INFANTS AND YOUNG CHILDREN (3 TO 36 MONTHS OF AGE)
The rates of bacterial infection in older infants and toddlers lie in between the higher rates for newborns and the lower rates for school-age children. As is the case for those younger and older, the urinary tract is the most common site of bacterial infection associated with fever in this age group, with a reported incidence of approximately 5%. Responsiveness of fever to antipyretics does not correlate with likelihood of presence of bacterial disease. While several prospective design studies have disproved any such correlation, many parents continue to value this myth.
Occult bacteremia, which is defined as a positive blood culture in a well-appearing febrile child who has no discernable focus of infection on clinical evaluation, has become less of a concern for children younger than 36 months. This is in great part attributable to the introduction of modern vaccination practices for strains of Haemophilus influenza type b (in 1986) and Streptococcus pneumococcus (in 2000).
Clinical examination alone will also fail to identify all instances of bacterial disease in older infants. McCarthy and colleagues at Yale University have developed a workable objective clinical tool to help identify the likelihood of serious bacterial disease in the face of fever.11 Sensitivity (74%) and specificity (75%) of the tool are very good but are not perfect. Many children with potentially serious illnesses can appear well on clinical examination and vice versa. For the toxic-appearing older infant or toddler, there is uniformity of opinion and approach: All should have thorough investigation for possible bacterial sources of infection and should receive parenteral antimicrobial therapy (ie, a third-generation cephalosporin and possibly vancomycin) as inpatients. The choice of antibiotic(s) should be tailored to combat the pathogens most commonly identified through institutional and community surveillance. It is the well-appearing child with insidious infection who benefits most from additional laboratory testing.
Diagnostic Testing
Numerous investigators have studied the utility of commonly available laboratory tests in identifying children at increased risk for occult bacteremia. One study of febrile children between 3 and 36 months of age demonstrated that increased risk of occult bacteremia correlated with total white blood cell counts above 15,000 per microliter.18
In this study, the risk of occult bacteremia was 10.8% for those children who had two peripheral blood white blood cell counts of 25,000 per microliter or higher. However, the sensitivity of that single parameter was only 21%.
Urinary tract infections (UTIs) occur in up to 7% of boys younger than 6 months and in up to 8% of girls younger than 1 year of age.19 Overall, girls are about twice as likely to have UTIs as boys, and white children are almost 10 times more likely to have UTIs than nonwhites. Unfortunately, dipstick urinalysis is not a reliable means of detecting presence of bacteriuria; sensitivities approximate 80% in large cohorts of young children. In infants younger than 6 months of age, there is evidence to suggest that Gram stain has excellent (> 90%) correlation with presence of bacteriuria. Thus, many experts recommend that a specimen of urine for culture be obtained in otherwise asymptomatic febrile boys younger than 6 months of age and in otherwise asymptomatic girls younger than 1 year of age. The means of obtaining the urine sample is important, as bag technique in younger children is much more prone to contamination than clean catch, catheterization, or needle aspiration of the bladder.
The value of spinal fluid analysis and culture in children has decreased as the occurrence rates of different types of meningitis have decreased with the advent of new vaccinations. However, while the overall rates of occurrence of different types of bacterial meningitis have been substantially reduced, the incidence remains highest in children younger than 2 years and in adults older than 60 years of age. Clinical appearances can at times be misleading. Whenever meningitis is suspected, a sample of cerebrospinal fluid should be obtained for analysis and culture, and a prudent decision should be made about early administration of antibiotics.
The majority of older infants and toddlers who acquire bacterial meningitis will have either suggestive historical or physical findings (ie, ill-appearance, seizure activity) or abnormal laboratory test results (ie, positive CSF Gram stain, elevated CSF protein, elevated peripheral blood, or CSF ANC).
A recent multicenter retrospective review of data from febrile children younger than 20 years of age identified a five-component clinical tool that assigns very low risk of bacterial meningitis to children who meet all five very-low-risk criteria (negative CSF Gram stain, CSF ANC < 1000, CSF protein < 80, peripheral CBC ANC < 10,000, no evidence of acute associated seizure activity). This clinical tool has not yet been prospectively tested for reliability.
Management Approach
Published fever-management protocols have called for empirical administration of antibiotics to certain cohorts of infants and children who have higher temperatures (ie, 39°C or higher) or to those in the higher temperature range who also have an elevated peripheral white blood cell count (ie, 15,000 or higher).20-22 However, the relatively low prevalence of occult bacteremia and the even lower prevalence of serious sequelae, such as bacterial meningitis, has led to a physician practices trend toward less diagnostic and therapeutic intervention and closer outpatient observation. Thus, a thorough history, physical examination, and assessment of general appearance along with parental observation and reliable follow-up remain the mainstay of management for well-appearing febrile children without an identifiable source of infection. The management of occult bacteremia (positive blood culture without an obvious source of infection) is discussed in Chapter 227. 
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


