The Electrocardiogram in Infants and Children
Srikant B. Iyer
Introduction
The surface electrocardiogram (ECG) remains an efficient and inexpensive aid in the initial and emergent evaluation of dysrhythmias, conduction disturbances, myocardial damage and chamber hypertrophy and dilatation. Important differences exist between children of various ages and adults in ECG procedure and interpretation. This chapter provides an overview of the indications for obtaining a pediatric ECG, details of the ECG procedure and a suggested stepwise approach for the interpretation of pediatric ECGs.
Anatomy and Physiology
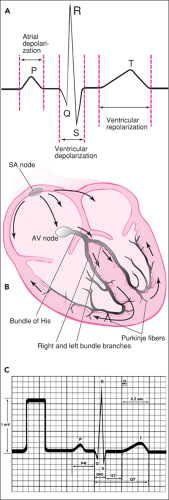
Figure 69.1A shows a diagrammatic representation and ECG tracing of a cardiac cycle (see also Chapters 22 and 70). The heart beats in response to an electrical signal that is generated by the heart’s “pacemaker,” normally the sinoatrial (SA) node located in the right atrium. This electrical signal is conducted through the atria and ventricles, creating an electrical impulse that may be recorded from electrodes applied to the skin. The recording of this impulse comprises the ECG. The appearance of an impulse will vary depending on which electrodes are used to make the recording.
The SA node impulse depolarizes the right and left atria, producing a P wave on the ECG. The impulse then arrives at the atrioventricular (AV) node, which conducts at a much slower to velocity than other parts of the heart. This “delay” in the AV node is represented by the PR interval. The impulse then travels rapidly through the bundle of His, the left and right bundle branches, the Purkinje fibers, and finally the ventricular muscle. This rapid conduction is represented by the QRS complex. If the QRS complex begins with a negative deflection, this negative deflection is called the Q wave. If the complex begins with a positive deflection, this positive deflection is called the R wave. The first negative deflection after the R wave is called the S wave. A second positive or negative deflection is called R′ or S′, respectively. Finally, repolarization of the ventricles produces the T wave.
The anatomy of the chest wall and the heart of the pediatric patient differs from that of an adult in a number of ways that directly affect the recording of the ECG. The heart of an infant or child is larger relative to the size of the thoracic cavity. The normal adult heart occupies about half the transverse diameter of the thorax, whereas the normal pediatric heart occupies up to two thirds of this space, depending on the age of the child. In general, the younger the patient, the larger the area that the heart occupies. As described below, this proportionately wider anterior chest surface area in infants and younger children is addressed when recording an electrocardiogram by adding one or two extra right-sided chest leads and, if necessary, an extra left-sided lead. Many of the other age-related differences in pediatric ECGs are related to changes in ventricular dominance. The normal right ventricular (RV) dominance of the newborn period is gradually replaced by left ventricular (LV)
dominance in adulthood. Because the ECG reflects these changes in heart size and ventricular dominance, there is great variation in the normal values for various ECG measurements. The following changes occur with increasing age:
dominance in adulthood. Because the ECG reflects these changes in heart size and ventricular dominance, there is great variation in the normal values for various ECG measurements. The following changes occur with increasing age:
The PR interval, QRS duration, and QT interval increase.
The QRS axis changes from a right anterior direction in infants to a left posterior direction in adults.
The R/S ratio in the right precordial leads decreases.
The R/S ratio in the left precordial leads increases.
The T vector also changes significantly depending on patient age. During the first 3 days of life (and up to 8 to 10 days of age), the T vector is directed anteriorly, resulting in upright T waves in the anterior precordial leads. Immediately after this period and throughout early adolescence, the T vector is directed posteriorly, resulting in inverted T waves in the anterior precordial leads. During adolescence, the T vector gradually shifts to an anterior direction again, resulting in upright T waves in the anterior precordial leads. Therefore, correct interpretation of the T vector requires knowing these expected age-based normal conduction patterns.
An exhaustive explanation of the physiologic and electromechanical principles of electrocardiography and vectorcardiography is beyond the scope of this chapter. The references listed at the end of this chapter provide more detailed explanations of these principles.
Indications
The most common indications for obtaining an ECG in the pediatric patient are listed in Table 69.1. History of palpitations, heart racing, and fluttering of the heart should lead the clinician to consider an underlying electrocardiac abnormality or a structural lesion. Tachycardias, bradycardias, or irregular rates and/or rhythms should be detectable on examination of the patient, and the ECG can be used as a confirmatory and diagnostic tool.
Signs of cardiac failure may be subtle in infants and young children (e.g., poor feeding, sweating during feeds), and the differentiation from primary pulmonary disease can be difficult. Pediatric patients with heart failure may manifest nonspecific electrocardiographic changes or changes associated with
a specific underlying cardiac lesion. An electrocardiogram can be helpful in determining previously undiagnosed congenital heart disease or onset of acquired heart disease such as pericarditis or myocarditis.
a specific underlying cardiac lesion. An electrocardiogram can be helpful in determining previously undiagnosed congenital heart disease or onset of acquired heart disease such as pericarditis or myocarditis.
TABLE 69.1 Indications for ECG Tracing in Pediatric Acute Care | |
|---|---|
|
The presence of a heart murmur sometimes constitutes an indication for performing an ECG with a pediatric patient. The significance of the murmur—that is, whether it may represent underlying cardiac disease—is determined by the intensity, radiation, and point of maximum loudness. Children in a high output state, such as hyperpyrexia, may present with a loud murmur that is not significant. However, if the patient has no known prior history of murmur and the clinical picture cannot be defined, an ECG may be helpful.
Cyanosis related to pulmonary disease usually improves significantly with oxygen. Cyanosis not ameliorated by oxygen may be related to a hemoglobinopathy but may also be related to previously undiagnosed cyanotic congenital heart disease. An electrocardiogram can be useful in screening for the cardiac causes of cyanosis.
While the differential diagnosis of chest pain in children is extensive, this complaint does not often relate to cardiac disease. The most common causes are respiratory and musculoskeletal etiologies as well as gastroesophageal reflux, costochondritis, and functional problems. However, the occasional pediatric patient with chest pain will show ECG findings consistent with cardiac strain, pericarditis, or myocarditis. In rare instances, there may be signs of ischemia. Additionally, chest pain without overt palpitations will sometimes be found in children with an aberrant atrial pathway such as Wolff-Parkinson-White syndrome.
TABLE 69.2 Equipment for Recording an Electrocardiogram | |
|---|---|
|
Syncope in children is usually related to noncardiac causes, such as vasovagal episodes, orthostatic syncope, and breath-holding spells. However, an electrocardiogram should be considered for all pediatric patients presenting with syncope to screen for arrhythmia as the cause. Syncope may be the only manifestation of prolonged QT syndrome, a condition that puts the patient at risk for subsequent sudden death.
Equipment
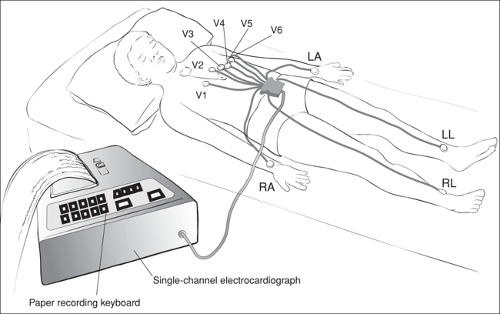
An electrocardiograph and its associated equipment are used to obtain an ECG (Table 69.2). These machines have evolved dramatically over the years from Einthoven’s galvanometer to today’s electronically sophisticated computerized devices. The keyboard, monitor, and simultaneous three-channel paper recording of an automated modern electrocardiograph are shown in Figure 69.2. These machines must be preprogrammed but after preprogramming are relatively simple to operate.
Electrodes are usually conveniently prepackaged. They are coated on one side with an adherent conducting material that holds the electrode in place on the patient’s skin. On the other side, they have a conducting button or clip holder that attaches to the electrode wires. The appropriate electrode wires, recording paper, and plugs are supplied with the machine.
Procedure
The patient should be lying supine on an examining table or crib that is free of vibration, electrical interference, and human contact. The usual array of distractors and tricks may calm the crying infant or frightened child. If these are not successful, sedation may be required, depending on the urgency with which the tracing is required and the general clinical status of the patient.
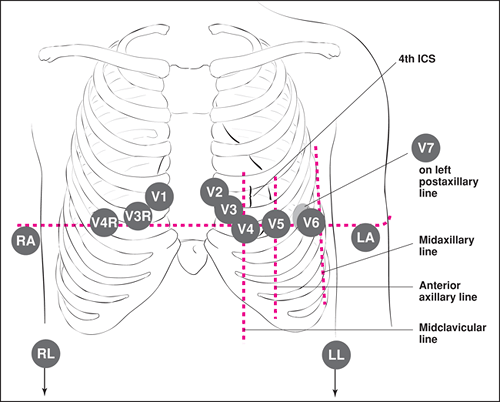
The proper sites for placement of the electrodes are listed in Table 69.3 and are shown in Figure 69.3. Proper placement is essential, particularly when sequential ECG tracings will be required over time for a given patient. For effective
lead attachment, it may be necessary to clean the skin with isopropyl alcohol to remove oils before placement of the electrodes. Some adolescents will have enough body hair that the electrode sites may need to be abraded slightly by rubbing with dry gauze or, rarely, to be shaved.
lead attachment, it may be necessary to clean the skin with isopropyl alcohol to remove oils before placement of the electrodes. Some adolescents will have enough body hair that the electrode sites may need to be abraded slightly by rubbing with dry gauze or, rarely, to be shaved.
TABLE 69.3 Electrode Location | ||
|---|---|---|
|
The number and sites of electrode placement for the chest leads depend on the age of the patient. For infants and children up to approximately 1 year of age, the electrodes shown in Figure 69.3 will normally be required. Children between 1 and 12 years of age should have leads V4R through V6 recorded. For patients older than 12 years of age, only leads V1 through V6 are necessary.
Depending on the design of the machine, the electrode lead wires must be attached to the electrode by the appropriate clip, button, or probe. The wires are marked near their distal ends with symbols corresponding to those in Figure 69.3 and Table 69.3. Modern machines that are designed primarily for adult use have chest lead wires that are only dedicated for leads V1 through V6, and an additional “nondedicated” wire is available for V4R, V3R, and V7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree