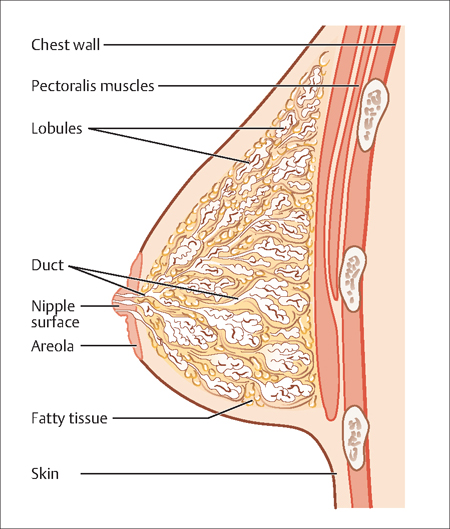
36 The Breast and Benign Breast Disease Robert L. Barbieri The breast overlies the chest wall from the second to the sixth rib. The medial border is the sternum, the lateral border is the latissimus dorsi, the superior border the clavicle, and the inferior border is the costal margin and the upper rectus sheath. The breast contains glandular adipose and connective tissues. The glandular tissues of the breast are arranged in 15 to 20 lobes (Fig. 36.1). Each lobe consists of a branching arrangement of lobules and acini. The acini are lined by a layer of milk-secreting epithelial cells. Each acinus is surrounded by a criss-crossing array of contractile myoepithelial cells. The lumens of the acini connect to collecting intralobular ducts which empty into the main collecting system of the lobe. Each lobe drains into the nipple. The nipple consists of a pigmented areola. The sebaceous glands that are located on the perimeter of the areola are the glands of Montgomery. The glandular tissue of the lobules and acini are embedded in adipose tissue which accounts for most of the breast volume. The lobules are separated by Cooper ligaments, which are connective tissue sheets that run from the subcutaneous tissue to the chest wall. Fig. 36.1 Anatomy of the breast The main function of the breast is secretion of milk. Breast milk contains the milk proteins casein and lactal-bumin, free fatty acids, and the milk sugar lactose. Lactose is a disaccharide of glucose and galactose. The breast is sensitive to the sex steroids, estradiol, progesterone, and testosterone, and to reproductive protein hormones including prolactin and oxytocin. During puberty and pregnancy these hormones stimulate the breast to grow. Estradiol stimulates the ductal system and progesterone stimulates the growth of the acini and the stromal tissues. In eu-estrogenic environments, androgens inhibit breast growth. In premenopausal women, the breast examination is best timed after menses but before ovulation. For postmeno-pausal women, the breast examination can be performed at any time. The examination begins with inspection of the breast with the patient in both upright and supine positions to look for asymmetry, skin changes such as erythema or dimpling, and nipple inversion, retraction, or discharge. The regional lymph nodes, especially those in the axilla, clavicular area and neck should be palpated for enlargement. A bimanual examination of the breast should be performed with the patient in the sitting and supine positions with the arm extended above the head. In the sitting position the breast can be supported by one hand while palpating it with the finger pads, not the finger tips, of the other hand. Palpation of the breast usually is performed in concentric circles starting from the nipple and moving outward, or in vertical strips starting laterally and moving toward the sternum. Using light pressure, the finger pads can be used to exam the breast tissue immediately under the skin. Using firmer pressure the finger pads can be used to exam the breast tissue deep to the skin. Gentle, but firm, pressure around the areolar area can be performed to check for breast secretion. Breast self-examination can be reviewed at the completion of the examination. During pregnancy the breast is exposed to high levels of lactogenic hormones, including prolactin, human placental lactogen and placental growth hormone, a variant of pituitary growth hormone. In the nonpregnant woman, prolactin concentration is about 15 ng/mL. During the third trimester of pregnancy, prolactin concentration is about 300 pg/mL. Serum human placental lactogen concentration is 6 000 000 pg/mL during the third trimester. These lactogenic and growth factors stimulate the alveoli to grow and prepare for lactation. During pregnancy, the very high serum concentrations of progesterone block lactogenesis. After delivery of the placenta, the rapid decrease in estradiol and progesterone releases the block to lactogenesis and results in an increase in the production of the milk proteins, fatty acids, and sugar that occurs over 3–5 days. During suckling, neural signals from the nipple travel through thoracic nerves 4, 5 and 6 to the paraventricular and supraoptic nuclei and stimulate the release of oxytocin from the hypothalamus—posterior pituitary. Oxytocin causes contraction of the myoepithelial cells causing the flow of milk through the ducts to the nipple. Visual and auditory stimuli can also cause the release of oxytocin. Suckling stimulates the pituitary to release prolactin, which maintains lactogenesis by stimulating gene transcription in the alveolar epithelial cells, increasing the production of the milk proteins, fatty acids, and sugar. The best food for a newborn and infant is breast milk. Breast milk is recommended as the exclusive or main nutrient source of food during the first 6 months of life. From 6 months to 1 year of age, breast milk should be combined with solid food. Human breast milk has immediate and long-term health benefits for the newborn and infant. Breast milk provides benefits to gastrointestinal action, defense against infections, and possibly a reduced risk of developing obesity as an adult. Hormones in breast milk, including epidermal growth factor and nerve growth factor, help the immature gastrointestinal mucosa of the newborn to grow and mature an epithelial barrier that helps protect against infections acquired through the gastrointestinal tract. In addition milk contains the secretory immunoglobulin IgA and IgG, interleukins, lysozyme, and immune cells that likely reduce the risk of infection. In developing countries, neonatal morbidity and mortality are reduced by breast-feeding compared with bottle feeding. In developed countries, the rate of neonatal hospitalization is less among breastfed infants. In one population-based survey among approximately 16 000 infants living in the United Kingdom, exclusive breast-feeding reduced the risk of hospitalization for diarrhea by 60% compared with never-breast-fed infants. Similarly the risk of hospitalization for respiratory infection was reduced by about 50% by breast-feeding. Breast-feeding may also reduce the risk of otitis media by about 50%. Breast-feeding during infancy may also reduce the risk of obesity, diabetes, and myocardial infarction in later life. In developed countries there are no major contraindications to breast-feeding except for active maternal infection with HIV, because of the risk of maternal-to-infant infection; and maternal consumption of certain drugs, such as cyclophosphamide and amiodarone, which may affect the newborn and infant. If the newborn is affected by galactosemia—an inherited inborn error metabolism that prevents the proper metabolism of galactose—no exposure to lactose should occur. In developing countries, women infected with HIV may need to breast-feed because of lack of formula supplements. For these women, treatment with an antiretroviral agent such as nevirapine, or the combination of nevirapine plus zidovudine, reduces the risk of transmission of HIV to the infant by about 50%. Mastitis is a common infection of the breast, typically with Staphylococcus aureus or Streptococcus, which presents as a firm, erythematosus, swollen and tender quadrant or localized area of the breast. Most women with mastitis present with a high temperature, greater than 38.3 °C. Treatment of mastitis includes continued breastfeeding, to move milk through the ducts, an antipyretic agent such as ibuprofen, and an antibiotic such as diclox-acillin 500 mg taken orally, four times daily for 10–14 days. A breast abscess is an uncommon problem in breastfeeding women, which may be preceded by untreated or incompletely treated mastitis. As with most abscesses, treatment involves drainage of the abscess by needle aspiration or incision-drainage, and antibiotic treatment. About 1% of healthy women are carriers of methicillin-resistant Staphylococcus aureus (MRSA). There is a developing trend that up to 50% of cases of breast abscess are caused by MRSA, necessitating the use of active surveillance and broad-spectrum antibiotics such as vancomycin. Theoretically, maternal treatment with vancomycin could cause diarrhea in newborns. A galactocele is a cystic collection of milk caused by an obstructed duct. Needle aspiration reveals milk as demonstrated by the presence of milk fats. Suckling activates multiple neuroendocrine systems that inhibit gonadotropin-releasing hormone (GnRH) secretion and the pituitary secretion of luteinizing hormone and follicular stimulating hormone, which inhibits ovulation. The degree to which breast-feeding suppresses GnRH secretion and inhibits ovulation is influenced by the intensity of the breast-feeding, the nutritional status of the mother and the body mass and body composition of the mother. Lactation is a major metabolic challenge for the mother, especially if she is undernourished. When nutrition is adequate and the body mass and composition are normal, breast-feeding is less likely to cause prolonged anovulation. During exclusive breast-feeding about 40% of women will remain anovulatory at 6 months post-partum. Lactating women who remain anovulatory may have higher serum prolactin levels than those who become ovulatory during lactation. High doses of estrogen, progestin, and androgens suppress lactation. Steroid contraceptive hormones, especially those that contain both estrogen and progestin, significantly alter the volume of breast milk and its composition. Standard estrogen—progestin oral contraceptives reduce breast milk volume by about 40%. In contrast, a progestin-only contraceptive reduces daily breast milk volume by about 10%. Standard estrogen—progestin oral contraceptives also reduce the breast milk concentration of lactalbumin, lactoferrin, and lactose, but these reductions are very modest and within the lower part of the normal range. The neurocognitive development and weight gain of exclusively breast-fed infants whose mothers took steroid contraceptives appear to be normal. However, if exclusive breast-feeding is planned, it is probably best to use a progestin-only contraceptive or an intrauterine device. Fig. 36.2 Algorithm for the evaluation of nipple discharge Nipple discharge is common among women. An simplified algorithm for the evaluation of nipple discharge is presented in Fig. 36.2
Breast Structure and function
Breast Examination
Lactation
Breast-Feeding
Mastitis, Breast Abscess, and Galactocele
Breast-Feeding and Amenorrhea
Breast-Feeding and Contraception
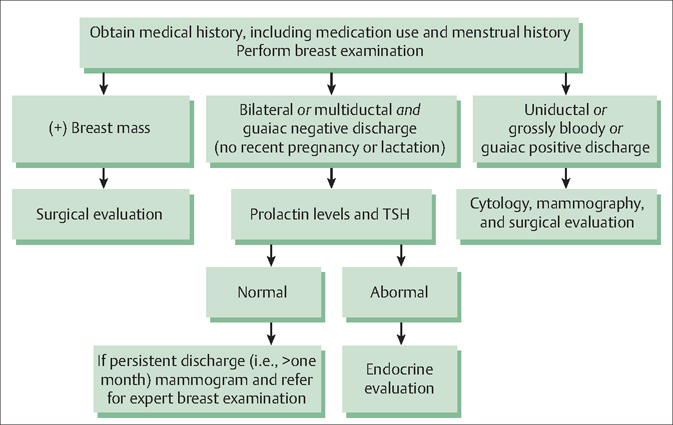
Nipple Discharge
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


