Background
Intrauterine balloon tamponade is an effective treatment for postpartum hemorrhage when first-line treatments fail. The optimal duration of intrauterine balloon tamponade for management of postpartum hemorrhage is unclear.
Objective
The objective of the study was to determine whether intrauterine balloon tamponade removal >12 hours of duration is associated with postpartum hemorrhage–related clinical outcomes.
Study Design
This was a retrospective cohort study of women with postpartum hemorrhage from 2007 through 2014 who underwent intrauterine balloon tamponade. We excluded failures of intrauterine balloon tamponade (intrauterine balloon expulsion with duration <2 hours or if hysterectomy was required prior to planned intrauterine balloon removal). Patients who underwent intrauterine balloon tamponade for 2–12 hours were compared with those who underwent intrauterine balloon tamponade for >12 hours. Examined postpartum hemorrhage–related clinical outcomes included estimated blood loss after intrauterine balloon tamponade placement, blood product transfusion, use of adjuvant measures to control postpartum hemorrhage after intrauterine balloon tamponade (either uterine artery embolization or hysterectomy), and maternal intensive care unit admission. Secondary outcomes examined included postpartum fever and hospital length of stay. Multivariable logistic regression models were used to control for confounding variables.
Results
Of 274 eligible women, 206 (75%) underwent intrauterine balloon tamponade for >12 hours and 68 (25%) underwent intrauterine balloon tamponade for 2–12 hours. The median estimated blood loss after intrauterine balloon tamponade placement (190 vs 143 mL, P = .116) as well as the frequencies of blood product transfusion (62.1% vs 51.5%, P = .120), transfusion of ≥4 U of packed red blood cells (17.0% vs 14.7%, P = .659), uterine artery embolization (15.1% vs 16.2%, P = .823), hysterectomy (0.0% vs 1.5%, P = .248), and intensive care unit admission (8.7% vs 7.4%, P = .721), was not statistically different between the groups, and this lack of association persisted in multivariable regressions. Intrauterine balloon tamponade duration >12 hours was associated with a higher frequency of postpartum fever (27% vs 15%, P = .047) and a longer mean hospital length of stay (3.7 vs 3.1 days, P = .002). After adjusting for variables that differed statistically between groups, the difference in length of stay associated with intrauterine balloon tamponade duration was no longer present, but the association between intrauterine balloon tamponade duration >12 hours and postpartum fever persisted (odds ratio, 2.33, 95% confidence interval, 1.07–5.11). Including chorioamnionitis as an independent variable in a post hoc multivariable analysis diminished the association between intrauterine balloon tamponade >12 hours and postpartum fever (adjusted odds ratio, 2.04, 95% confidence interval, 0.92–4.53).
Conclusion
There are no significant differences in postpartum hemorrhage–related outcomes associated with intrauterine balloon tamponade duration >12 hours compared with removal 2–12 hours. If ongoing hemorrhage has abated, it is reasonable to consider the removal of an intrauterine balloon by 12 hours after its initial placement.
Aggressive treatment is essential in the management of postpartum hemorrhage (PPH), the world’s leading cause of maternal mortality. When first-line treatments such as uterotonic agents and bimanual uterine massage fail, intrauterine balloon tamponade (IUBT) has been shown to be effective, with reported bleeding cessation rates of 55–94%. However, previous studies have been limited to case series and small observational studies, and thus, many questions remain about the appropriate management of the intrauterine balloon devices once they have been successfully placed and hemorrhage has abated. Specifically, it remains unknown what the optimal duration of IUBT is with regard to PPH-related outcomes.
IUBT is proposed to stop obstetric hemorrhage by direct tamponade of the vascular placental bed, encouragement of uterine contractility, and/or direct hydrostatic pressure on the uterine arteries. Whether these actions are successful and sustained after a set duration of IUBT has not been previously studied.
We sought to determine whether IUBT duration is associated with PPH-related outcomes. We hypothesized that a longer duration of IUBT would be associated with increased effectiveness in the management of PPH.
Materials and Methods
This is a retrospective cohort study of all women who underwent IUBT at Northwestern Memorial Hospital (Chicago, IL) from January 2007 to October 2014. The estimated blood loss (EBL) is routinely recorded in the delivery form of our electronic medical record. A query of cases with an EBL of ≥500 mL after a vaginal delivery or ≥1000 mL after a cesarean delivery yielded all cases of PPH. Medical records for each case of PPH were then reviewed to identify women undergoing IUBT.
At the study institution, IUBT was recommended by protocol as a second-line option for the management of PPH refractory to uterotonic agents and bimanual uterine massage. The protocol indications for use of IUBT included placental site bleeding and uterine atony. The IUBT device used was the Bakri postpartum balloon (Cook Medical Inc, Bloomington, IN).
We excluded women whose balloon was removed within the first 2 hours of placement because of expulsion (n = 33) as well as women who underwent hysterectomy prior to planned IUBT removal for refractory hemorrhage (n = 7) because these circumstances indicated a failure of IUBT rather than an outcome related to the duration of IUBT placement. We identified no cases in which IUBT was discontinued intentionally before 2 hours because of perceived success in controlling PPH.
After placement of IUBT, patients underwent a period of observation on the labor and delivery unit, with close monitoring of vital signs and ongoing estimation of blood loss. The duration of IUBT was at the discretion of the clinical provider and was not dictated by protocol; thus, this practice pattern varied at the study institution. A designated nurse was tasked with recording the events of the PPH episode, including ongoing estimation of blood loss as well as timing and type of intervention. When the decision was made for removal, the intrauterine balloon was deflated over the course of 5–10 minutes and the patient monitored on the labor and delivery unit for the subsequent 2–3 hours to ensure clinical stability of the PPH.
Demographic data, labor and delivery data, and postpartum data were gathered from the electronic medical record. Demographic and baseline clinical data collected included maternal age, self-reported race and ethnicity, and delivery admission body mass index. Obstetric data abstraction included gestational age at delivery, gravidity and parity, multiple gestation, the presence of placenta previa, polyhydramnios, preeclampsia requiring the use of magnesium sulfate infusion, chorioamnionitis, mode of delivery, EBL before balloon placement, the use of uterotonic agents, and antibiotic use.
Chorioamnionitis was defined as a minimum temperature of 100.4°F, with clinical signs of intrauterine infection (fetal or maternal tachycardia, purulent discharge, uterine tenderness, or leukocytosis). All cases of chorioamnionitis received broad-spectrum antibiotics with initiation during the intrapartum period.
Patients undergoing cesarean delivery also received preoperative antibiotics for surgical prophylaxis, and in those who had chorioamnionitis and underwent cesarean delivery, broad-spectrum antibiotics were continued for 24 hours postpartum. Additionally, nighttime placement (between 6:00 pm and 7:00 am ) and daytime removal of IUBT were included to measure the influence of provider preference for removal of IUBT during the day.
The PPH outcomes evaluated included nadir hemoglobin ≤6 mg/dL, transfusion of any blood products, transfusion of ≥4 U of packed red blood cells (PRBCs), EBL after balloon placement, uterine artery embolization, hysterectomy performed after IUBT removal, and maternal intensive care unit (ICU) admission.
Transfusion was defined as transfusion of any blood product, including red blood cells, platelets, fresh frozen plasma, or cryoprecipitate. EBL after IUBT placement was estimated clinically by a combination of blood-soaked sponge count, weighed disposable pads and drapes, and output from the IUBT device itself. Clinical staff members who participate in the care of patients with PPH are trained in the estimation of obstetric blood loss through mandatory ongoing EBL training at the study institution.
Secondary outcomes included postpartum fever (defined as a temperature of ≥100.4°F) and postpartum length of stay. Postpartum length of stay was calculated forward from the time of delivery until discharge.
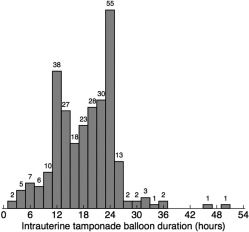
National guidelines for IUBT duration are lacking, so based on an observed bimodal distribution of timing of IUBT duration in our institution (one peak leading up to 12 hours, the other peak leading up to 24 hours), we compared women who had IUBT duration of 2–12 hours with those who had an IUBT duration >12 hours (see Figure ).
The groups were compared using the Wilcoxon rank-sum test, χ 2 test, and Fisher exact test, as appropriate. Tests of hypothesis were 2 tailed with a predefined alpha of 0.05. Logistic regression models that included statistically significant differences ( P < .05) in bivariable analyses were performed to determine the effect of confounding on the results.
We used Stata Statistical Software, release 14 (2015; StataCorp, College Station, TX). The Northwestern University Research Institutional Review Board approved the study.
Results
During the study period, 93,825 deliveries occurred, of which 5731 (6.1%) resulted in PPH. An intrauterine balloon was placed in 314 women with PPH (5.5%). Of these, 40 (13%) were excluded because of expulsion in the first 2 hours or excessive ongoing hemorrhage requiring immediate alternative interventions prior to planned balloon removal, leaving 274 patients for analysis. There were 206 women who had an IUBT duration of >12 hours (75.2%) and 68 women with an IUBT duration of 2–12 hours (24.8%). The IUBT duration range was 2–51 hours, with most durations between 10 and 24 hours, as seen in the histogram ( Figure ).
Women with IUBT duration >12 hours were more likely to have undergone cesarean delivery (56.3% vs 35.3%, P = .003) and less likely to have had the intrauterine balloon placed during the nighttime (between 6:00 pm and 7:00 am ) (36.9% vs 75.0%, P < .001). Other baseline characteristics and markers of management leading up to the hemorrhage were similar between the groups ( Table 1 ).
| Characteristic | IUBT 2–12 hours (n = 68) | IUBT >12 hours (n = 206) | P value |
|---|---|---|---|
| Total IUBT duration, median hours | 11 (8–12) | 21 (17–24) | < .001 |
| Age, y | 33 (29–36) | 33 (29–37) | .720 |
| Race/ethnicity | .711 | ||
| Non-Hispanic white | 40 (58.8) | 101 (49.0) | |
| Non-Hispanic black | 7 (10.3) | 25 (12.1) | |
| Asian | 5 (7.4) | 17 (8.3) | |
| Hispanic | 2 (2.9) | 10 (4.8) | |
| Other | 14 (20.6) | 53 (25.7) | |
| Body mass index, kg/m 2 | 30.1 (26.8–35.8) | 30.3 (27.6–35.2) | .440 |
| Gestational age, wks | 39.1 (37.3–40.1) | 38.8 (37.0–39.6) | .374 |
| Nulliparous | 30 (44.1) | 110 (53.4) | .184 |
| Multiple gestation | 13 (19.1) | 46 (22.3) | .576 |
| Placenta previa | 2 (2.9) | 10 (4.9) | .504 |
| Polyhydramnios | 1 (1.5) | 1 (0.5) | .408 |
| Preeclampsia | 12 (17.7) | 24 (11.7) | .204 |
| Magnesium sulfate infusion a | 13 (19.2) | 30 (14.6) | .371 |
| Chorioamnionitis | 3 (4.4) | 21 (10.2) | .144 |
| Cesarean delivery | 24 (35.3) | 116 (56.3) | .003 |
| Uterotonic agents used, total number | .494 | ||
| Zero | 0 (0) | 6 (2.9) | |
| One | 3 (3.4) | 8 (3.9) | |
| Two | 4 (5.9) | 17 (8.3) | |
| Three | 20 (29.4) | 69 (33.5) | |
| Four | 41 (60.3) | 106 (51.5) | |
| EBL before IUBT placement, mL | 2000 (1317–2373) | 2000 (1555–2520) | .173 |
| Nigh time placement (6:00 pm to 7:00 am ) | 51 (75.0) | 76 (36.9) | < .001 |
| Prophylactic antibiotic use | 61 (89.7) | 196 (95.2) | .107 |
| Daytime removal (7: 00 am to 6: 00 pm ) | 50 (73.5) | 165 (80.1) | .253 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


