Background
Cervical cancer is the third most common gynecologic malignancy in the United States. Approximately 1-3% of cervical cancers will be diagnosed in pregnant and peripartum women; optimal management in the setting of pregnancy is not always clear.
Objective
We sought to describe the management of patients with cervical cancer diagnosed in pregnancy and compare their outcomes to nonpregnant women with similar baseline characteristics.
Study Design
We conducted a retrospective chart review of all patients diagnosed with cervical cancer in pregnancy and matched them 1:2 with contemporaneous nonpregnant women of the same age diagnosed with cervical cancer of the same stage. Patients were identified using International Classification of Diseases, Ninth Revision codes and the Dana-Farber/Massachusetts General Hospital Cancer Registry. Data were analyzed using Stata, Version 10.1 (College Station, TX).
Results
In all, 28 women diagnosed with cervical cancer during pregnancy were identified from 1997 through 2013. The majority were Stage IB1. In all, 25% (7/28) of women terminated the pregnancy; these women were more likely to be diagnosed earlier in pregnancy (10.9 vs 19.7 weeks, P = .006). For those who did not terminate, mean gestational age at delivery was 36.1 weeks. Pregnancy complications were uncommon. Complication rates in pregnant women undergoing radical hysterectomy were similar to those outside of pregnancy. Time to treatment was significantly longer for pregnant women compared to nonpregnant patients (20.8 vs 7.9 weeks, P = .0014) but there was no survival difference between groups (89.3% vs 95.2%, P = .08). Women who underwent gravid radical hysterectomy had significantly higher estimated blood loss than those who had a radical hysterectomy in the postpartum period (2033 vs 425 mL, P = .0064), but operative characteristics were otherwise similar. None of the pregnant women who died delayed treatment due to pregnancy.
Conclusion
Gestational age at diagnosis is an important determinant of management of cervical cancer in pregnancy, underscoring the need for expeditious workup of abnormal cervical cytology. Of women who choose to continue the pregnancy, most delivered in the late preterm period without significant obstetric complications. For women undergoing radical hysterectomy in the peripartum period, complication rates are similar to nonpregnant women undergoing this procedure. Women who died were more likely to have advanced stage disease at the time of diagnosis. This information may be useful in counseling women facing the diagnosis of cervical cancer in pregnancy.
Introduction
Cancer diagnosis during pregnancy has risen over the last 50 years, now complicating up to 1 in 1000 pregnancies. Some authors suggest that this may be attributable to delay in childbearing to third or fourth decade of life. Cervical cancer is the third most common gynecologic cancer in the United States, with >12,000 new cases of invasive cervical cancer diagnosed annually and approximately 4000 cervical cancer–related deaths every year.
Cervical cancer is most frequently diagnosed at an early stage in both pregnant and nonpregnant populations, and typically treated surgically with radical hysterectomy plus bilateral pelvic lymphadenectomy. Approximately 1-3% of cases of cervical cancer will be diagnosed in pregnant or peripartum women. However, the optimal treatment for cervical cancer diagnosed in pregnancy is not always clear. Providers must consider stage at the time of diagnosis, trimester of pregnancy, and patient preferences regarding pregnancy outcome. We sought to describe the management and subsequent outcomes of patients with cervical cancer diagnosed in pregnancy compared to nonpregnant women with similar baseline characteristics.
Materials and Methods
This was a retrospective study of all patients diagnosed with cervical cancer in pregnancy at Brigham and Women’s Hospital and Massachusetts General Hospital. Patients were identified using International Classification of Diseases, Ninth Revision codes and the Dana Farber and Massachusetts General Hospital Cancer Registry. These women were then matched 1:2 with contemporaneous nonpregnant patients diagnosed within the same 5-year period. Patients were stage- and age-matched for comparison.
Information was collected regarding sociodemographic characteristics as well as medical and pregnancy history. Pregnancy outcomes included termination of pregnancy, mode of delivery for women who did not undergo termination, gestational age (GA) at delivery, birthweight, and 5-minute Apgar scores. Oncologic outcomes of interest included time from diagnosis to treatment, method of treatment (surgical vs medical), operative time, estimated blood loss (EBL), surgical complications, and 5-year survival. Surgical complications were defined as intensive care unit admission, unexpected injury to adjacent organs, or reoperation. In a planned subgroup analysis among women diagnosed with cervical cancer in pregnancy, we compared outcomes of women who elected termination of pregnancy with those who continued their pregnancy. Finally, we evaluated surgical outcomes for women who underwent gravid radical hysterectomy and compared them to women who had surgical management in the postpartum period. Study data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at Partners Health System. REDCap is a secure, World Wide Web–based application designed to support data capture for research studies.
Data were analyzed using software (Stata, Version 10.1; StataCorp LP, College Station, TX). The χ 2 test was used for categorical data, while a 2-sided t -test was used for continuous variables. A P value of <.05 was considered significant. This study was approved by the Partners Health System Institutional Review Board.
Materials and Methods
This was a retrospective study of all patients diagnosed with cervical cancer in pregnancy at Brigham and Women’s Hospital and Massachusetts General Hospital. Patients were identified using International Classification of Diseases, Ninth Revision codes and the Dana Farber and Massachusetts General Hospital Cancer Registry. These women were then matched 1:2 with contemporaneous nonpregnant patients diagnosed within the same 5-year period. Patients were stage- and age-matched for comparison.
Information was collected regarding sociodemographic characteristics as well as medical and pregnancy history. Pregnancy outcomes included termination of pregnancy, mode of delivery for women who did not undergo termination, gestational age (GA) at delivery, birthweight, and 5-minute Apgar scores. Oncologic outcomes of interest included time from diagnosis to treatment, method of treatment (surgical vs medical), operative time, estimated blood loss (EBL), surgical complications, and 5-year survival. Surgical complications were defined as intensive care unit admission, unexpected injury to adjacent organs, or reoperation. In a planned subgroup analysis among women diagnosed with cervical cancer in pregnancy, we compared outcomes of women who elected termination of pregnancy with those who continued their pregnancy. Finally, we evaluated surgical outcomes for women who underwent gravid radical hysterectomy and compared them to women who had surgical management in the postpartum period. Study data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at Partners Health System. REDCap is a secure, World Wide Web–based application designed to support data capture for research studies.
Data were analyzed using software (Stata, Version 10.1; StataCorp LP, College Station, TX). The χ 2 test was used for categorical data, while a 2-sided t -test was used for continuous variables. A P value of <.05 was considered significant. This study was approved by the Partners Health System Institutional Review Board.
Results
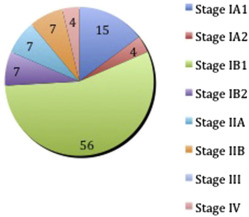
A total of 28 women diagnosed with cervical cancer during pregnancy were identified from 1997 through 2013. These patients were matched with 52 nonpregnant control patients. The majority of patients diagnosed with cancer in pregnancy were stage IB1 at the time of diagnosis ( Figure ). Demographic characteristics were similar between the pregnant and nonpregnant groups, as were medical comorbidities ( Table 1 ).
| Pregnant n = 28 | Nonpregnant n = 52 | P value | |
|---|---|---|---|
| Demographics | |||
| Age, y Mean (SD) | 33.2 (5.0) | 34.4 (5.6) | |
| Public insurance N (%) | 6 (22.2) | 10 (20) | .82 |
| White N (%) | 20 (71.4) | 43 (82.7) | .24 |
| Nulliparous N (%) | 11 (39.3) | 20 (41.7) | .84 |
| English-speaking N (%) | 25 (89.3) | 46 (88.5) | .91 |
| Smoker N (%) | 13 (46.4) | 16 (32) | .21 |
| HIV positive N (%) | 1 (3.6) | 1 (2) | .67 |
On average, patients were diagnosed in the 17th week of gestation (mean GA at diagnosis 17.4 weeks). Of the pregnant patients, 25% (7/28) terminated their pregnancy after learning of their diagnosis. These women were significantly more likely to be diagnosed in the first trimester (mean GA at diagnosis 10.9 vs 19.7 weeks, P < .005) ( Table 2 ). While most pregnant women were early stage (79% of women who continued, 63% of women who terminated), all those who terminated were stage IB1 or greater at the time of the diagnosis (5/7 women stage IB1, 2/7 stage IIB). There were no differences in demographics, medical comorbidities, parity, or treating hospital between the 2 groups. Their oncologic outcomes were also similar ( Table 2 ).
| Termination n = 7 | No termination n = 21 | P value | |
|---|---|---|---|
| GA at diagnosis, wk Mean (SD) | 10.9 (4.1) | 19.7 (6.6) | .006 a |
| Oncologic outcomes | |||
| Surgical management N (%) | 6 (85.7) | 17 (81.0) | .78 |
| Operative time, min Mean (SD) | 294 (47.5) | 245 (21.2) | .30 |
| EBL, mL Mean (SD) | 1162 (787.8) | 1095 (352.9) | .93 |
| Transfusion N (%) | 1/5 (20) | 5/19 (26.3) | .77 |
| Still living N (%) | 5 (89.3) | 20 (95.2) | .08 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


