Contraindications include active knee infection, no functional instability with activity, lack of acceptable knee range of motion, or an inability to comply with the postoperative protocol for rehabilitation.
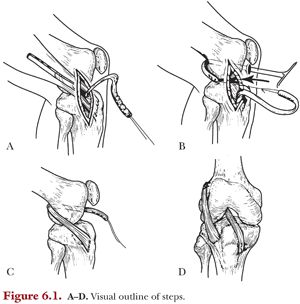
Our approach to ACL reconstruction in the skeletally immature patient is based on physiologic and skeletal age using the Tanner staging system and the Greulich and Pyle wrist atlas for each respective age. In prepubescent patients (Tanner 1 or 2), the author of this chapter prefer the combined intra-articular/extra-articular reconstruction with autogenous iliotibial band graft due to personal experience, technical ease, and recent biomechanical evidence exhibiting more closely restored anterior posterior and rotatory stability using this technique compared with other physeal-respecting reconstruction options (Fig. 6.1 A–D). Kocher et al.37 reported on 44 prepubescent patients (mean age, 10.3 years; range, 3.6 to 14.0 years) who underwent a combined extra-articular/intra-articular reconstruction using autogenous iliotibial band. The mean skeletal age was 10.1 years (range, 3.5 to 14.0 years). Of the 44 patients, 31 were Tanner stage 1 and 13 were Tanner stage 2. There were two traumatic reruptures (4.5%): one at 4.7 years and one at 8.3 years postoperatively, no growth disturbances, and mean (± SD) International Knee Documentation Committee (IKDC)65 score of 96.7 ± 6 and mean (± SD) Lysholm66 score of 95.7 ± 6.7 in the remaining patients. The mean follow-up was 5.3 years (range, 2.0 to 15.1 years), and the mean total height gained after surgery was 21.5 cm (range, 9.5 to 118.5 cm).
Although it is true that this reconstruction is not anatomic, a recent study by Kennedy et al.67 examined the kinematics of the combined intra-articular/extra-articular reconstruction with autogenous iliotibial band versus an all-epiphyseal reconstruction and a transtibial over-the-top reconstruction in a cadaver model. Their findings concluded that the iliotibial band reconstruction technique most closely restore native ACL kinematics. There was, however, a tendency for the technique to overconstrain the knee to varus rotational forces at certain angles of knee flexion. As is noted in the following texts, we have modified a portion of the technique from the original publication to prevent this occurrence. There is no explanation offered by the authors as to why this reconstruction technique was better able to restore native ACL kinematics. Anecdotally, we believe that the extra-articular tenodesis eliminates the rotatory instability, whereas the intra-articular reconstruction from other techniques principally eliminates only the anterior to posterior translational instability.
Surgical Technique Step by Step
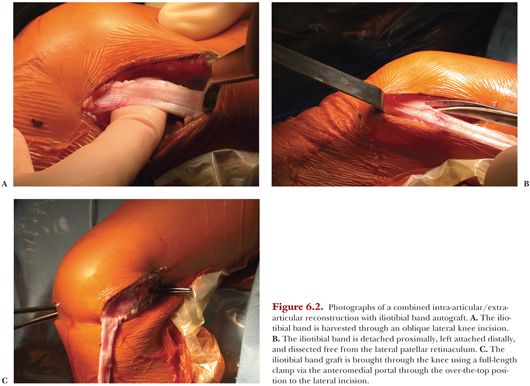
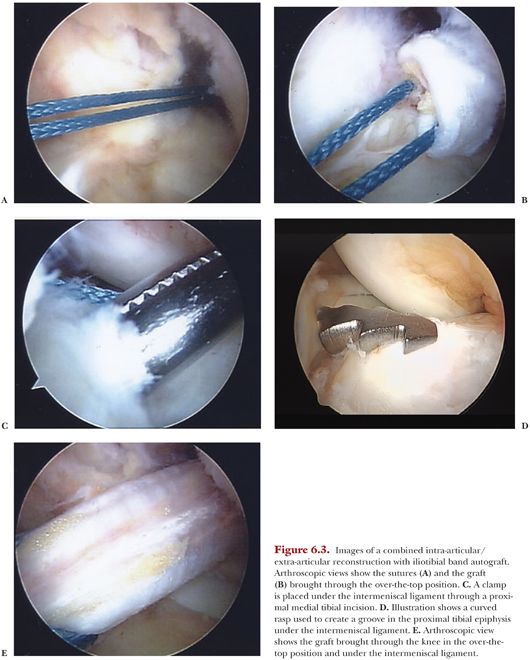
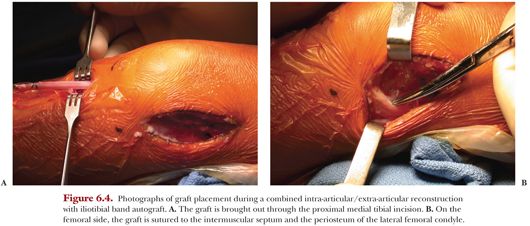
For this procedure, the child is placed in the supine position on a standard flat-top operating room (OR) table. A pneumatic tourniquet is placed as far proximally as possible on the thigh but is not routinely inflated during harvest to prevent iliotibial band tethering. The tourniquet is routinely inflated after harvest at the commencement of arthroscopy. Alternatively, a sterile tourniquet can be applied after harvest. An oblique 6-cm incision is made from the midlateral joint line to the anterior border of the iliotibial band (Fig. 6.2A). Subcutaneous fat should be dissected off the iliotibial band with a Cobb elevator. The anterior and posterior borders of the iliotibial band should be identified and incised; the incisions are carried proximally under the skin with a curved meniscotome. The iliotibial band is detached proximally with a curved meniscotome or an open tendon stripper. Alternatively, an additional proximal incision can be made to detach the tendon. Distal dissection of the tendon off the joint capsule and lateral patellar retinaculum is performed, but the tendon is left attached to the Gerdy tubercle (Fig. 6.2B). The free end is tubularized with a no. 5 nonabsorbable braided suture using a whipstitch technique. The graft is typically 10 cm relative to the lateral incision at this point. The graft is placed back in the wound, the tourniquet is inflated, and diagnostic arthroscopy is performed via standard anterolateral and anteromedial portals. The ACL remnant is excised and any intra-articular pathology can be treated at this point. The over-the-top position on the femur and the over-the-front position under the intermeniscal ligament on the tibia are identified. At most, a minimal notchplasty should be performed to avoid injury to the perichondral ring of the distal femoral physis.68 A curved clamp is passed through the anteromedial portal and bluntly through the capsule, out through the posterolateral compartment of the knee, and into the lateral incision (Fig. 6.2C). It is important to maintain the clamp on the posterolateral femur during dissection to avoid neurovascular injury. The free end of the graft is passed through the knee in the over-the-top position and the sutures are passed out via the anteromedial portal (Fig. 6.3 A,B). A two-incision rear-entry guide can also be used. A second incision is made on the anterior tibia near the pes anserinus, and the dissection is carried down 4.5 cm to the periosteum to ensure that the proximal tibial physis and tibial tubercle apophysis are not in the area of dissection. A curved clamp is used to tunnel up to and through the joint capsule under the intermeniscal ligament (Fig. 6.3C). The clamp is replaced with a rasp, which is used to create a groove for passage of the graft (Fig. 6.3D). The clamp is reintroduced via the tibial incision to grasp the sutures attached to the graft, and the graft is passed under the intermeniscal ligament (Fig. 6.3E), out of the knee joint, and into the tibial incision (Fig. 6.4A). The extra-articular portion of the reconstruction procedure is performed by securing the graft to the lateral femoral condyle at the insertion of the intermuscular septum with mattress sutures with the knee placed in 90 degrees of flexion (Fig. 6.4B). The author of this chapter have modified this portion of the procedure and no longer externally rotate the knee 15 degrees at this point to prevent overconstraint.67 Tibial fixation is subsequently accomplished by elevating two small flaps of periosteum in the anterior tibial incision and creating a shallow bony trough in the tibia with a motorized burr. Fluoroscopy can be used to confirm that the physis has not been violated. With the knee in 20 degrees of flexion and appropriate tension on the graft, the graft is secured to the periosteum in the bony trough with mattress sutures. With the knee in 20 to 30 degrees of flexion, distal tension is applied to the graft. No. 2 FiberWire sutures are thrown from proximal to distal then tied after all are placed. We use mattress sutures from superficial to deep through the medial periosteum, medial to lateral through graft, then deep to superficial through lateral periosteum, angling the stitches proximally to increase graft tension when tied. At least three sutures should be placed proximally in the femur and distally in the tibia. Tibial fixation may be supplemented with a post if necessary.

Patients are typically admitted overnight for pain control and therapy on postoperative day 1 to ensure safety with crutches or a walker if the child is very young.
List of Equipment
• Standard arthroscopy equipment (30-degree scope, shaver, etc.)
• Long right-angle retractor (Fig. 5)
• Rat-tail rasp (Fig. 5)
• Full-length clamp (Fig. 5)
• Curved and straight meniscotomes (Fig. 5)
• No. 2 FiberWire or similar suture
Rehabilitation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


