Suctioning the Trachea
Mary E. Lacher
Introduction
Suctioning is a technique used to maintain airway patency by removing pulmonary secretions, blood, vomitus, saliva, or other foreign material. Removal of these materials allows for the maintenance of gas exchange to provide adequate oxygenation and ventilation. In addition, suctioning removes potentially infective material from the upper airway and trachea. Suctioning may be nasal, oral, nasopharyngeal, or tracheal, depending on the patient’s particular problem. Tracheal suctioning began to be performed in the 1950s, concurrent with the development of positive pressure ventilation (1,2,3,4,5).
Even though suctioning is a common, basic procedure, it may be associated with complications and risks if not done properly. It is frequently performed in pediatric patients of all age groups and may be performed by health care providers with different training backgrounds (emergency medical technicians, nurses, physicians, respiratory therapists, etc.). Suctioning the upper airway is detailed in Chapter 13.
Anatomy and Physiology
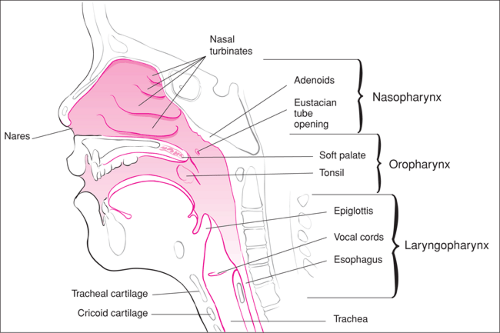
The upper airway includes the nose, mouth, and pharynx (Fig. 79.1). The upper airway has several functions, including (a) conducting inspired gases to the lungs, (b) acting as a filter to prevent foreign material from entering the lower airway, and (c) humidifying and heating inspired gases.
The nose is lined with ciliated and nonciliated mucous cells. These cells help humidify inspired gases and filter foreign material. The filtering of foreign material is aided by the hair follicles and the thick, sticky mucous secretions of the nose. When an artificial airway (i.e., endotracheal tube or tracheotomy) is in place, the protective mucociliary clearance system is bypassed, leading to a reduction in airway humidity and thus drying and thickening of the secretions. The generous blood supply to the nares helps to warm and humidify inspired gases. As much as 1,000 mL of water per day humidifies the inspired air by mucous and serous secretions (1). These glands also are stimulated to produce more secretions from inflammatory processes such as respiratory infections, allergies, and inhalation of toxic substances (e.g., smoke, chemicals).
From the base of the tongue, the laryngopharynx extends to the esophagus, which lies posterior to the trachea (Fig. 79.1). The proximity and function of these structures around the larynx serve to protect the airway from microbial organisms. Closure of the glottis during swallowing prevents food or other substances from contaminating the tracheobronchial tree. Patients with neuromuscular illness, anatomically abnormal airways, or poorly protected airways are at the greatest risk for aspiration of gastrointestinal contents.
Within the neck, the trachea begins at the level of the cricoid cartilage. The trachea descends in the middle of the neck to the vertebral level of T5-6 and bifurcates into the right and left bronchi. This bifurcation is positioned slightly angled to the right, making the opening to the right bronchi a less acute angle. This allows an endotracheal tube or suction catheter to enter the right mainstem bronchus if passed beyond the carina.
Gas flow during respiration in normal healthy airways occurs by laminar flow, with the molecules traveling parallel to the walls of the airway. Laminar flow is governed by the law of Poiseuille, which states that at a constant driving pressure, the resistance to flow of a gas will vary with the fourth power of the radius of the tube it transverses. For example, if the internal diameter of the tube is halved, resistance to flow will be increased 16-fold. Therefore, small changes in airway caliber, even in local parts of the tracheobronchial tree (e.g., secretions or debris causing obstruction, insertion of a suction catheter), can greatly increase resistance to gas exchange.
Airway secretions can affect respiratory function in several ways (Fig. 79.2). Initially, these secretions may provoke a local inflammatory response that leads to increased resistance to airflow by the narrowing secondary to hyperemia and edema. This increases the work of breathing necessary to move gases past the secretions and inflamed airways. Ventilation-perfusion mismatch occurs because plugging, inflammation, and retained secretions lead to uneven distribution of oxygen reaching the distal pulmonary bed. Perfused lung segments may not receive fresh air, which leads to hypoxemia and triggers increased ventilatory effort in an attempt to compensate. If retained secretions cause total plugging of the bronchioles, atelectasis will develop, leading to a reduction in lung compliance, thereby worsening the ventilation-perfusion mismatch. Atelectatic or inflamed lung segments also continue to produce secretions that further act as a culture media for bacteria.
Defense mechanisms exist to remove foreign debris and excess secretions from the airway that are caused by artificial airways or primary disease. Small amounts of foreign material are continually swept up by cilia and mucus to the supraglottic region, where they can be swallowed down the esophagus. Coughing also is a means by which the secretions and foreign material can be expelled from the airway. Receptors in the mucosa of the large respiratory passages are stimulated by irritation from secretions or foreign material, producing cough. Coughing begins with a deep inspiration, followed by a forced expiration against a closed glottis. The glottis is then suddenly opened, producing a forceful outflow of air.
Endotracheal or tracheotomy tubes tend to reduce effective cough and ciliary clearance, potentially leading to further inspissation of secretions. This is in part due to the need for a closed glottis for truly effective cough to be maintained. This is not possible with an endotracheal tube in place. Because the normal upper airway humidification systems are bypassed, secretions may be drier and thicker with artificial airways. The endotracheal tube impedes ciliary function. A foreign body can stimulate increased secretions.
Indications
Tracheal suctioning may be necessary any time foreign material is interfering with adequate ventilation or oxygenation of a patient with natural or artificial airways. A number of medical
conditions affect the production and clearance of secretions to the degree that tracheal suctioning is indicated. Children with pneumonia or cystic fibrosis often have increased thick secretions that are difficult to clear. Victims of smoke inhalation or other inhalation injury may have edema and increased secretion production. Head injury or intoxicated patients may have reduced or absent protective reflex mechanisms that assist in the maintenance of clear airway. Patients with poor pulmonary mechanics (due to thoracic-abdominal surgery, rib fracture or chest trauma, or neuromuscular disorders such as muscular dystrophy) may not be able to clear their secretions. In addition to suctioning to clear the airway, suctioning may be used to obtain sputum for a culture to aid diagnosis.
conditions affect the production and clearance of secretions to the degree that tracheal suctioning is indicated. Children with pneumonia or cystic fibrosis often have increased thick secretions that are difficult to clear. Victims of smoke inhalation or other inhalation injury may have edema and increased secretion production. Head injury or intoxicated patients may have reduced or absent protective reflex mechanisms that assist in the maintenance of clear airway. Patients with poor pulmonary mechanics (due to thoracic-abdominal surgery, rib fracture or chest trauma, or neuromuscular disorders such as muscular dystrophy) may not be able to clear their secretions. In addition to suctioning to clear the airway, suctioning may be used to obtain sputum for a culture to aid diagnosis.
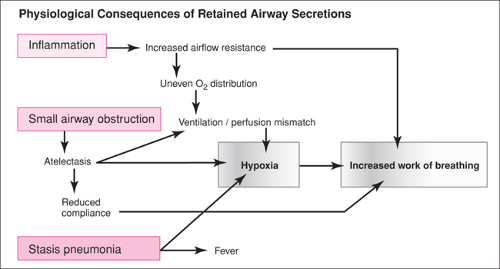 Figure 79.2 Physiologic consequences of retained secretions. (Adapted from Shapiro BA, Kacmarek RM, Cane RD, et al. Clinical Applications of Respiratory Care. St. Louis: Mosby; 1991.) |
Patients with artificial airways (tracheotomy cannula or endotracheal tube) have a routine need for suctioning. It is common for children with small artificial airways (endotracheal tube size 2.5 to 4.0) to require more frequent suctioning than older children or adults with larger airways just to ensure continued patency of the smaller tube.
Suctioning is performed frequently in the emergency department in patients with increased secretions or foreign material in the airway. The most common form is oral and nasopharyngeal suctioning (Chapter 13). Suctioning is routinely performed when a patient is being intubated to improve the visualization of landmarks and after the artificial airway is in place to maintain its patency and provide adequate oxygenation and ventilation.
Equipment
The necessary equipment for suctioning is listed in Table 79.1. Various types of catheters are available, depending on the type of suctioning to be performed (Fig. 79.3). One major type is a disposable, vented polyvinyl chloride plastic catheter (Fig. 79.3A); another is a Yankauer-type tube (Fig. 79.3B). When suctioning the upper airway, the catheter should be soft and pliable but not collapsible when suction is applied. The distal end should be open and have at least two holes and smooth edges. The catheter should allow for intermittent suction with a thumb control valve (Fig. 79.3C). With this valve, no suction occurs when the valve port is open. To create suction, the clinician places a thumb over the valve opening. The Yankauer catheter is frequently used to suction the pharynx before endotracheal intubation or when initially
clearing the oropharynx in children who are at risk for aspiration. In these instances, after intubation of the airway, the soft, vented polyvinyl catheter is used.
clearing the oropharynx in children who are at risk for aspiration. In these instances, after intubation of the airway, the soft, vented polyvinyl catheter is used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree