Splinting Teeth
Maria Carmen G. Diaz
Introduction
Children often present to the emergency department with traumatic dental injuries. Most of these injuries affect the maxillary central incisors. In primary dentition, these injuries are most frequently caused by falls, whereas in permanent dentition, these injuries often occur in motor vehicle accidents or during sporting events. Emergency physicians should be aware of the management of these common injuries.
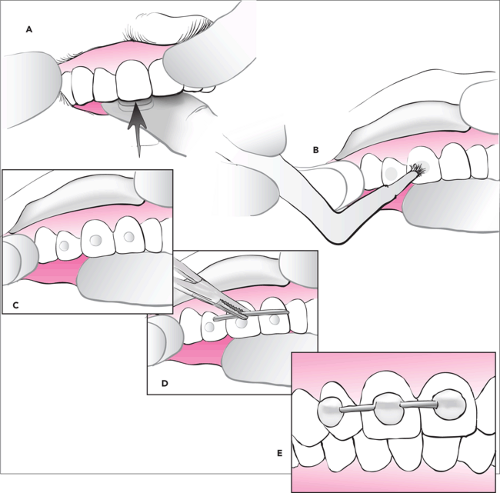
The emergent care of traumatized teeth should first and foremost optimize healing of the injured area and the supporting structures. Splinting teeth is an easy technique that allows the traumatized region to gain stability and support from neighboring unaffected teeth while the injured area is undergoing the healing process. It is vital that physicians be aware of proper splinting methods in order to enhance and ensure proper healing. Splinting is best done in the emergency department so that the regeneration process is initiated in a timely manner.
Anatomy and Physiology
Teeth are composed of enamel, dentin, and cementum. They contain a neurovascular supply within the root canal and pulp chamber and are suspended in the supporting alveolar bone by fibrous periodontal ligaments. By providing stability and preventing further damage, splints permit and promote the regeneration of the periodontal ligaments (1). It is these ligaments that maintain the integrity of the root and form the attachment between the root and the bone. Absence of these periodontal ligaments results in ankylosis, a bony union between the tooth and the alveolar bone. Persistence of this bony union may eventually result in facial deformities. Splints also enhance the regeneration of cementum, which is most critical for the development of root resorption and ultimately tooth vascularity and viability.
Clinical healing of the periodontium takes place within the first 7 days after a traumatic injury. It is crucial that the recovery period enhance the regeneration of these junctional fibers. The alveolar socket is continuously remodeling in response to functional stimuli. The splint applied should not impair but rather augment this remodeling process (2).
Indications
Types of injuries that require dental splints include reimplanted avulsed permanent teeth, luxated or extruded permanent teeth that have been repositioned, crown-root fractures in permanent dentition, and alveolar fractures (3,4,5,6). It is best not to splint injured teeth that have minimal mobility. Also, care should be taken in attempting to splint teeth when there are surrounding artificial crowns or large fillings, as these synthetic structures do not provide adequate support for the splint. Injured primary teeth should not be splinted, as immobilization in these types of teeth increases the risk for ankylosis. Attempting to apply a splint in a very uncooperative patient may be difficult and may require the assistance and expertise of a dental consultant. The duration of the splint varies depending on the type of injury but ranges between 1 and 3 weeks (7).
Principles of Splinting Teeth
The ideal splint should create an environment in which tooth movement can be contained within physiologic limits while restoring function and patient comfort. An acceptable splint should be simple to apply directly on the teeth and not cause
any trauma during its application. It should immobilize the injured tooth in a normal position while allowing physiologic mobility in order to promote regeneration of periodontal fibers but discourage ankylosis and external root resorption. The fixation provided by the splint should last during the entire period of immobilization and not permanently alter the tooth structure. Additionally, the patient needs to feel comfortable while wearing the splint. The splint should therefore not interfere with occlusion or articulation and should not impinge on the gingiva. Any damage to the surrounding soft tissues may disrupt the healing process and may lead to bacterial infection. It is imperative that the patient be able to maintain good oral hygiene while the splint is in place. The splint should not predispose the teeth to caries and should
not interfere with potential endodontic therapy. Finally, the splint should be easy to remove once therapy is completed (8,9).
any trauma during its application. It should immobilize the injured tooth in a normal position while allowing physiologic mobility in order to promote regeneration of periodontal fibers but discourage ankylosis and external root resorption. The fixation provided by the splint should last during the entire period of immobilization and not permanently alter the tooth structure. Additionally, the patient needs to feel comfortable while wearing the splint. The splint should therefore not interfere with occlusion or articulation and should not impinge on the gingiva. Any damage to the surrounding soft tissues may disrupt the healing process and may lead to bacterial infection. It is imperative that the patient be able to maintain good oral hygiene while the splint is in place. The splint should not predispose the teeth to caries and should
not interfere with potential endodontic therapy. Finally, the splint should be easy to remove once therapy is completed (8,9).
Equipment
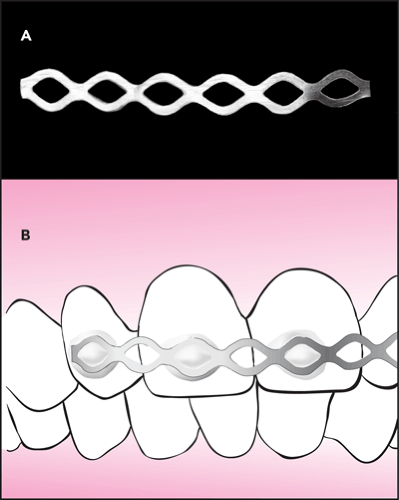
Many different types of splints have been studied throughout the years. One type of splint that meets nearly all of the above criteria is the acid-etch wire composite splint (9,10). Materials needed to apply this type of splint include the following:
Light-cured composite material
Etchant
Bonding material
Flat plastic applicator
0.6- to 0.7-mm stainless steel orthodontic wire
Wire cutters and pliers
Cotton wool rolls
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree