Chapter 12
Spinal, Epidural, and Caudal Anesthesia
ANATOMY, PHYSIOLOGY, AND TECHNIQUE
Naveen Nathan MD, Cynthia A. Wong MD
Chapter Outline
The art and science of neuraxial anesthesia requires a thorough appreciation of neuroanatomy and the physiologic effects imposed by medications commonly administered via the spinal and/or epidural route. The focus of this chapter is to characterize the anatomic and technical considerations for neuraxial anesthesia. The reader is referred to Chapter 23 for a corresponding discussion of the physiologic and untoward effects of neuraxial analgesia in laboring women and to Chapter 26 for a discussion of neuraxial anesthesia for cesarean delivery. Successful administration and management of neuraxial anesthesia requires well-developed technique moderated by sound clinical judgment.
Anatomy
Neuraxial Anatomy
The Spinal Cord, Spinal Canal, and Meninges
The cephalad aspect of the spinal cord is continuous with the brainstem through the foramen magnum. The spinal cord most often terminates as the conus medullaris at the level of the lower border of the first lumbar vertebral body. The conus medullaris is attached to the coccyx by means of a neural-fibrous band called the filum terminale, which is surrounded by the nerves of the lower lumbar and sacral roots, known as the cauda equina. Within the bony vertebral column are three membranes: the pia mater, the arachnoid mater, and the dura mater. The pia mater is a highly vascular membrane that closely invests the spinal cord. The arachnoid mater is a delicate, nonvascular membrane closely adherent to the third and outermost layer, the dura. The subarachnoid space, located between the pia mater and arachnoid mater, contains (1) cerebrospinal fluid (CSF), (2) spinal nerves, (3) a trabecular network between the two membranes, (4) blood vessels that supply the spinal cord, and (5) lateral extensions of the pia mater—the dentate ligaments. The dura mater is a membrane composed of collagen that encapsulates the spinal cord, the deeper meningeal layers, and the subarachnoid space. This layer forms a connective tissue sheath along the vertical axis of the central nervous system (CNS) that is contiguous with connective tissue covering the lateral extension of spinal nerve roots as they exit the intervertebral foramina. The interface between the dural and arachnoid layers has been described as a potential space capable of expansion subsequent to mechanical trauma. Unintentional injection of local anesthetic into this subdural space may explain some cases of failed spinal anesthesia. It may also explain the rare, slow-to-develop cases of high spinal anesthesia after the inadvertent subdural injection of larger volumes of local anesthetic intended for epidural administration.1 Although the spinal cord ends at the level of the bodies of L1 and L2 in most patients, the subarachnoid space and cauda equina continue to the S2 level (Figure 12-1).
The Epidural Space
The epidural space is located external to the sac of the dura mater and contains loose connective tissue, adipose tissue, lymphatics, spinal nerve roots, and the internal vertebral venous plexus (Batson’s plexus) (Figure 12-2). This space is bound by the posterior longitudinal ligament anteriorly, the ligamentum flavum and the periosteum of the lamina posteriorly, the pedicles of the vertebrae, and the intervertebral foramina with their contents laterally. The epidural space is closed at the foramen magnum where the spinal dura attaches to the dura of the cranium and at the sacral hiatus by the sacrococcygeal ligament. Frequently, anatomic references will illustrate neuraxial anatomy by way of sagittal and/or transverse cross section. This may result in the erroneous impression that the epidural space is a continuous columnar entity that envelops the dural sac at all points about its perimeter. Investigations using cryomicrotome sections and three-dimensional reconstruction of radiologic data verify that the epidural space is in fact discontinuous along the vertical and lateral axes of the spinal canal. It varies in anteroposterior thickness according to dermatomal distribution, being widest at the level of lumbar vertebrae and thinnest in the cervical region.2,3 Epiduroscopy and epidurography suggest the presence of a dorsal median connective tissue band in some individuals.4 Anatomic dissection and computed tomographic epidurography have also suggested the presence of epidural space septa. This band (or these septa) may provide an explanation for unilateral or incomplete epidural anesthesia.5 However, some investigators have suggested that the dorsal median band is an artifact of epidural space distention or an anatomic manifestation of the previously unappreciated epidural space segmentation.3
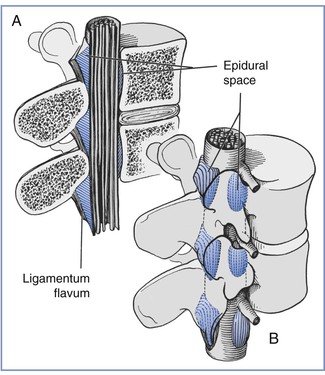
FIGURE 12-2 A, Sagittal section of the epidural space demonstrates that the contents of the epidural space depend on the level of the section. B, Three-dimensional drawing of the epidural space shows the discontinuity of the epidural contents. However, this potential space can be dilated by the injection of fluid into the epidural space. (Redrawn from Stevens RA. Neuraxial blocks. In Brown DL, editor. Regional Anesthesia and Analgesia. Philadelphia, WB Saunders, 1976:323).
The Vertebral Column and Ligaments
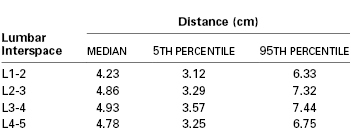
The ligamentum flavum lies posterior to the epidural space (Figure 12-3). The lamina, the spinous processes of the vertebral bodies, and the interspinous ligaments lie posterior to the ligamentum flavum. Posterior to these structures are the supraspinous ligament (which extends from the external occipital protuberance to the coccyx), subcutaneous tissue, and skin. Historically, some have described the ligamentum flavum as a single ligament. In actuality, however, it is composed of two curvilinear ligaments that join in the middle and form an acute angle with a ventral opening.3,6 Much like the epidural space, the ligamentum flavum is not uniform from skull to sacrum; indeed, it is not uniform even within a single intervertebral space. The thickness of the ligamentum flavum varies with vertebral level, body mass index, and age, as does the distance between the skin and the epidural space (Table 12-1).7,8
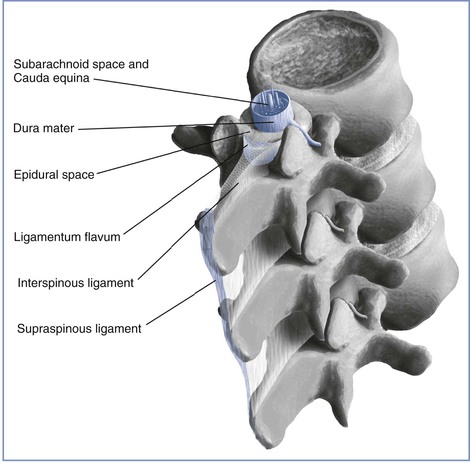
FIGURE 12-3 Central neuraxial anatomy. Note the variable thickness of the ligamentum flavum, which is greatest in the midline and decreases as it fans out laterally. (Drawing by Naveen Nathan, MD, Northwestern University Feinberg School of Medicine, Chicago, IL.)
Anatomic Changes of Pregnancy
The normal anatomic changes of pregnancy affect the use of neuraxial anesthesia techniques. Uterine enlargement and vena caval compression result in engorgement of the epidural veins. Unintentional intravascular epidural catheter cannulation and injection of local anesthetic are more common in pregnant patients than in nonpregnant patients. In addition, the vertebral foraminal veins, which are contiguous with the epidural veins, are enlarged and obstruct one of the pathways for anesthetic egress from the epidural space during administration of epidural anesthesia. The enlarged epidural veins also may displace CSF from the thoracolumbar region of the subarachnoid space, as does the greater intra-abdominal pressure of pregnancy; this displacement partly explains the lowered dose requirement for spinal anesthesia in pregnant women.9 Subarachnoid dose requirements are also affected by the lower specific gravity of CSF in pregnant patients than in nonpregnant patients.10
The hormonal changes of pregnancy affect the perivertebral ligamentous structures, including the ligamentum flavum. The ligamentum flavum may feel less dense and “softer” in pregnant women than in nonpregnant patients; thus, sensing the passage of the epidural needle through the ligamentum flavum may be more difficult. It may also be more difficult for a pregnant woman to achieve flexion of the lumbar spine. Progressive accentuation of lumbar lordosis alters the relationship of surface anatomy to the vertebral column. At least three changes may occur. First, a pregnant woman’s pelvis rotates on the long axis of the spinal column; thus, the line joining the iliac crests (Tuffier’s line) assumes a more cephalad relationship to the vertebral column (e.g., this imaginary line might cross the vertebral column at the L3 to L4 interspace rather than the L4 to L5 interspace). Second, there is less space between adjacent lumbar spinous processes during pregnancy. It may be more difficult to use the midline approach to identify the epidural or subarachnoid space in pregnant women. (Thus the often-heard comment, “She has a narrow interspace.”) Third, magnetic resonance imaging has shown that the apex of the lumbar lordosis is shifted caudad during pregnancy, and the typical thoracic kyphosis in women is reduced during pregnancy.11 These changes may influence the spread of subarachnoid anesthetic solutions in supine patients, leading to a higher sensory level in the pregnant patient (Figure 12-4).12 Finally, labor pain makes it more difficult for some women to assume and maintain an ideal position while the anesthesia provider performs neuraxial anesthesia.
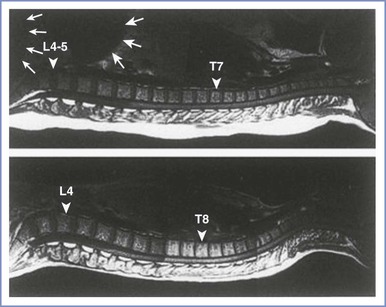
FIGURE 12-4 The curvature of the spinal column in the pregnant female (top) and nonpregnant female (bottom). The large and small white arrows indicate the uterus and fetal head, respectively. The apex of the lumbar lordosis moves caudad (triangular arrow), and the thoracic kyphosis is reduced and moves cephalad (triangular arrow) in the pregnant woman. (Reprinted with permission from Hirabayashi Y, Shimizu R, Fukuha H. Anatomical configuration of the spinal column in the supine position. II. Comparison of pregnant and non-pregnant women. Br J Anaesth 1995; 75:6-8.)
Physiology
Obstetric Pain Pathways
Pain during the first stage of labor results primarily from changes in the lower uterine segment and cervix. Pain is transmitted by visceral afferent nerve fibers that accompany the sympathetic nerves and enter the spinal cord at the T10 to L1 segments. During the late first stage and second stage of labor, pain results from distention of the pelvic floor, vagina, and perineum. Pelvic pain is transmitted by somatic nerve fibers, which enter the spinal cord at the S2 to S4 segments (Figure 12-5).
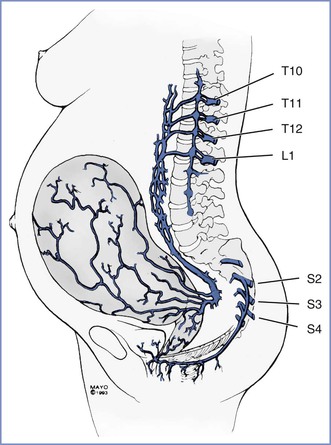
FIGURE 12-5 Pain pathways during labor and delivery. The afferent pain pathways from the cervix and uterus involve nerves that accompany sympathetic fibers and enter the neuraxis at T10 to L1. The pain pathways for the pelvic floor and perineum include the pudendal nerve fibers, which enter the neuraxis at S2 to S4.
During cesarean delivery, additional nociceptive pathways are involved in the transmission of pain, and a T4 level of anesthesia is required to provide adequate anesthesia. Most cesarean deliveries are performed with a horizontal (e.g., Pfannenstiel) skin incision, which involves the infraumbilical T11 to T12 dermatomes. During surgery, stretching of the skin may involve dermatomes two to four levels higher. Intraperitoneal manipulation and dissection involve poorly localized visceral pain pathways. Visceral pain may be transmitted by pathways as high as the celiac plexus. Additional somatic pain impulses may occur as a result of diaphragmatic stimulation because the intercostal nerves innervate a portion of the peripheral diaphragm.
Physiology of Neural Blockade
Hormonal changes, anatomic changes, and decreases in CSF specific gravity likely are responsible for the lower local anesthetic dose requirements for spinal anesthesia in pregnant women.10,13 Local anesthetics produce conduction blockade primarily by blocking sodium channels in nerve membranes, thereby preventing the propagation of neural impulses. Differential blockade is manifested as differences in the extent of cephalad blockade of temperature discrimination and vasomotor tone, sensory loss to pinprick, sensory loss to touch, and motor function. Temperature discrimination and vasomotor tone are blocked to the greatest extent (i.e., most cephalad level) and motor function to the least extent. During spinal anesthesia, local anesthetics act directly on neural tissue in the subarachnoid space. Regression of anesthesia can be explained by the simple vascular uptake of local anesthetic from the subarachnoid space and spinal cord.14 Epidural anesthesia has a much smaller zone of differential motor–sensory–sympathetic blockade; this difference suggests that the mechanism of epidural anesthesia must involve more than simple diffusion across the dura. For many years, nerve fiber size was presumed to be the primary determinant of susceptibility to local anesthetic blockade (i.e., smaller fibers are blocked more readily than larger fibers). However, later studies have shown that the length of nerve fiber exposed to local anesthetic is as important as the size of the nerve fiber. Fink15 hypothesized that the length of nerve fiber exposed to local anesthetic affects the extent of the differential zone of motor and sensory blockade. With spinal anesthesia, the local anesthetic concentration required to block sufficient sodium channels to affect motor, sensory, and sympathetic function is less than that needed for the better-protected nerves found in the epidural space; thus, a wider band of differential blockade occurs during spinal anesthesia than during epidural anesthesia.
The understanding of the mechanisms of spinal and epidural anesthesia likely remains oversimplified. Nonetheless, it seems clear that spinal anesthesia results primarily from the effects of local anesthetic on the spinal cord, whereas epidural anesthesia results from the effects of local anesthetic on nerve tissue within both the epidural and subarachnoid spaces.
Technique
Pre-procedural Considerations
Monitoring
The American Society of Anesthesiologists (ASA) has published guidelines for administration of neuraxial anesthesia in obstetric patients (see Appendix A). Among other things these recommendations address (1) the required presence of qualified anesthesia and obstetric care providers, (2) immediate availability of resuscitation medication and equipment (Box 12-1), (3) mandatory pre-procedural intravenous access, and (4) employment and documentation of maternal vital signs and fetal heart rate (FHR) monitoring.
During the initiation of neuraxial analgesia for labor, all patients are monitored with an automatic blood pressure cuff and a pulse oximeter to facilitate continuous assessment of the maternal heart rate and oxygenation. Maternal blood pressure is measured every 1 to 2 minutes after the administration of the test and therapeutic doses of local anesthetic for approximately 15 to 20 minutes, or until the mother is hemodynamically stable. Subsequently (during maintenance of neuraxial analgesia), maternal blood pressure is measured every 15 to 30 minutes or more frequently if hypotension ensues. Continuous pulse oximetry during maintenance analgesia is used in selected patients (e.g., patients with obstructive sleep apnea or cardiovascular disease). Rarely, invasive hemodynamic monitoring is necessary. The sensory level of analgesia and the intensity of motor block are assessed after the administration of the test and therapeutic doses of local anesthetic. Subsequently, sensory level and motor block are assessed at regular intervals.
Neither the ASA nor the American College of Obstetricians and Gynecologists (ACOG) provides a specific recommendation as to whether continuous FHR monitoring is necessary during performance of neuraxial anesthesia procedures. The ASA Task Force on Obstetric Anesthesia16 has stated:
The fetal heart rate should be monitored by a qualified individual before and after administration of neuraxial analgesia for labor. The Task Force recognizes that continuous electronic recording of the fetal heart rate may not be necessary in every clinical setting and may not be possible during initiation of neuraxial anesthesia.
The anesthesia provider cannot predict when hypotension will occur during the administration of neuraxial anesthesia. In addition, there is concern that intrathecal administration of an opioid is associated with a higher incidence of nonreassuring FHR patterns than other neuraxial techniques (see Chapter 23).17 Thus, we believe that continuous electronic FHR monitoring should be performed both during (if possible) and after the administration of neuraxial analgesia in all laboring women. In some cases, the mother’s position or maternal obesity precludes the use of an external Doppler device to monitor the FHR. In such cases (especially when there is concern regarding fetal well-being), it is helpful for the obstetric provider to place a fetal scalp electrode to monitor the FHR.
Informed Consent, Patient-Procedure Verification, and Partner’s Presence
Prior to initiation of neuraxial anesthesia, a pre-procedural verification process (i.e., “time-out”) is instituted as part of compliance with national patient safety recommendations from hospital accreditation organizations.18 The participation of the patient, the anesthesia care provider, and a third party such as a member of the nursing staff may lead to the discovery of concerns that should be addressed before the initiation of neuraxial anesthesia. The risk of neuraxial procedures relates to (1) the physical instrumentation of the spinal axis and (2) physiologic changes associated with medication administration via this anatomic route. Contraindications to needle or catheter placement include patient refusal or inability to cooperate, ongoing bleeding diathesis, infection either at the site of intended intervention or untreated systemic blood-borne illness, and increased intracranial pressure predisposing to cerebral herniation. Contraindications to injecting local anesthetics via the epidural or spinal route include severe hypovolemia and allergy to local anesthetics. It would be axiomatic that patient refusal presents an absolute contraindication to an elective procedure. A thorough preoperative assessment of current fetal well-being, maternal volume status, intrapartum systemic opioid use, antibiotic administration for ongoing chorioamnionitis or other infectious process, and a brief reiteration of known maternal disease states, including allergies, will readily identify most of the major concerns that would render neuraxial anesthesia potentially hazardous. The anesthesia provider should weigh the risks and benefits of neuraxial anesthesia for each patient.
Informed consent should include a frank discussion about anesthetic procedures and risks. Surveys of postpartum women have demonstrated that most parturients want to know the possible complications of epidural analgesia, even those that are rare.19,20 It is best to relay this information before the onset of labor (e.g., during antenatal classes),21 or early in the intrapartum period, although doing so is not always feasible. Some anesthesia providers fear that distressed, desperate, or sedated parturients may not understand the discussion of anesthetic procedures. However, adequacy of consent can be demonstrated not only by documentation of information provided to the patient but also by the lack of patient objection to a procedure and the cooperation provided by the patient during the procedure.22 In a survey of North American anesthesiologists, Brull et al.23 found that a majority of clinicians did not disclose the most severe risks of central neuraxial anesthesia to their patients. Additionally, most anesthesiologists cited inaccurate incidences of these complications. We do not find it difficult to explain the procedure and the risks of neuraxial analgesia to a laboring woman. The preanesthetic evaluation allows the physician to communicate a sense of concern and to demonstrate a commitment to the patient’s care. Most laboring women understand the need for informed consent, and they appreciate the opportunity to participate in decisions about their care.
Management of the pregnant patient occurs in a unique clinical care environment in which the presence of the patient’s spouse or family member must be addressed. Most often, the dictates of local institutions will establish whether a partner’s presence during neuraxial labor analgesia is acceptable. However, hospital policy may be vague enough that the discretion lies in the hands of the anesthesia provider. Intuition may suggest that a partner who remains present during the conduct of neuraxial analgesia may help alleviate the patient’s ongoing anxiety regarding the procedure. Conversely, the partner may be so apprehensive or disruptive that the partner’s presence becomes counterproductive to the care of the patient. Orbach-Zinger et al.24 randomized 84 nulliparous women to either presence or absence of their partner during labor epidural catheter placement. Interestingly, patient and partner anxiety, as measured by a validated anxiety questionnaire, were reduced when partners were absent during the procedure.
Patient Positioning
Pregnant women have an exaggerated lumbar lordosis, and it is more difficult for them to flex the lumbar spine. However, most pregnant women are young, and youth usually allows sufficient flexibility to facilitate the insertion of a needle into the epidural or subarachnoid space. Whether the block is initiated in the lateral or sitting position is a matter of provider and patient preference. Notable advantages of the lateral position include (1) orthostatic hypotension is less likely and (2) the position often facilitates continuous FHR monitoring during placement of the epidural catheter. Vincent and Chestnut25 performed a study in which they observed that neither the sitting nor the lateral position was consistently superior with regard to patient comfort. However, pregnant women who preferred the left lateral decubitus position weighed less and had lower body mass indices than women who preferred the sitting position. The sitting position is likely associated with a higher incidence of orthostatic hypotension and syncope. However, the sitting position is preferred—and may be required—in obese parturients, in whom identification of the midline is usually significantly easier in the sitting position. Further, morbidly obese women may experience hypoxemia when placed in the lateral decubitus position.
One study demonstrated a greater reduction in maternal cardiac output with maximal lumbar flexion in the lateral decubitus position than in the sitting position during identification of the epidural space in laboring women.26 The researchers speculated that maximal lumbar flexion in the lateral decubitus position results in concealed aortocaval compression. In contrast, they suggested that the uterus falls forward (and thus does not cause aortocaval compression) when the patient assumes the sitting flexed position. They recommended that “the tight fetal curl position be avoided,” especially when the patient assumes the lateral decubitus position for identification of the epidural or intrathecal space.
Aortocaval compression must be avoided at all times. The gravid uterus can occlude the inferior vena cava and aorta when the parturient assumes the supine position.27–29 This position may cause maternal hypotension30,31 and reduce uteroplacental perfusion,32 even in the absence of anesthesia. Increased venous tone in the lower extremities helps overcome partial occlusion of the inferior vena cava in unanesthetized pregnant women. If maternal hydration is inadequate and if aortocaval compression is not avoided, the onset of anesthesia-induced sympathetic blockade may result in decreased venous return, cardiac output, and uteroplacental perfusion.29
Maternal position during placement of the epidural catheter does not seem to affect the incidence of unintentional dural puncture. However, adoption of the lateral recumbent head-down position for epidural catheter placement may reduce the incidence of epidural venous puncture.33
When spinal or epidural anesthesia is performed with the patient in a lateral position, the patient’s back should lie at, and parallel to, the edge of the bed, for at least two reasons. First, the edge is the most firm section of the mattress. If the patient lies away from the edge of the bed, the patient’s weight will depress the mattress, and the anesthesia provider must work in a “downhill” direction. Second, this position allows anesthesia providers to keep their elbows flexed, facilitating control of fine hand and wrist muscle movements. The plane of the entire back should be perpendicular to the mattress. When asked to flex the lower back, patients typically roll the top shoulder forward, an action that rotates the spine (which is undesirable) but does not flex the lower back.
Similarly, patients positioned sitting should have their feet supported by a stool with the backs of their knees against the edge of the bed, a maneuver that helps position the patient’s back closer to the anesthesia provider. The shoulders should be relaxed symmetrically over the hips and buttocks. Beds in obstetric units often break at the foot, and the split in the mattress encourages the patient’s seat to slope downhill if she is straddling the mattress split; this position will cause spine rotation and may make the procedure more difficult.
When spinal anesthesia is performed, the patient’s posture relative to the baricity of the anesthetic solution should be considered, because it influences the extent of blockade, the latency of blockade, and the incidence of hypotension. The incidence, timing, and extent of hypotension in the period immediately after initiation of the block depend on the type of block (e.g., spinal, epidural, or combined spinal-epidural [CSE]), drug characteristics (e.g., baricity, concentration), patient position during the procedure, and patient position in the period following the procedure. For example, when spinal anesthesia is initiated with a hyperbaric solution for instrumental vaginal delivery, it often makes sense for the patient to be sitting to ensure the rapid onset of sacral anesthesia. Conversely, spinal anesthesia for cervical cerclage can be initiated with the patient in the steep lateral Trendelenburg position with a hypobaric anesthetic solution.
Posture has less influence on the spread of epidural anesthesia.34–36 During epidural anesthesia, a unilateral block more likely results from the malposition of the catheter (or perhaps an anatomic barrier within the epidural space) than from patient position, particularly after a bolus injection. Norris and Dewan34 observed that gravity did not augment the spread of anesthesia in patients receiving epidural anesthesia for cesarean delivery, and they concluded that posture does not need to be manipulated to ensure adequate bilateral epidural anesthesia. In at least two studies it was noted that the use of the sitting position is not necessary for the development of good sacral anesthesia when large volumes of epidural local anesthetic are given for cesarean delivery.34,36 However, Reid and Thorburn36 observed that use of the sitting position appeared to delay the spread of anesthesia to the midthoracic dermatomes. In comparison with the bolus administration of epidural local anesthetic, the extent of blockade may be more gravity dependent when the anesthetic is administered as a continuous infusion over a prolonged period.
Some anesthesiologists contend that maternal position after epidural catheter placement affects the efficacy of epidural analgesia, although this is a matter of some dispute. Beilin et al.37 observed that the placement of the laboring woman in the supine position with a 30-degree leftward tilt was associated with better epidural analgesia than maintenance of the left lateral decubitus position. In contrast, Preston et al.38 observed no difference in analgesia and a significantly higher incidence of fetal bradycardia with the supine wedged position than with the full lateral position.
Caudal anesthesia is used infrequently in modern obstetric anesthesia practice. However, there remain some circumstances in which a caudal technique is useful and/or advantageous. It is a good choice for the second stage of labor in selected patients in whom the lumbar epidural approach is hazardous or contraindicated (e.g., fusion or instrumentation of the lumbar spine). In most cases, caudal anesthesia can be successfully performed with the patient in a lateral decubitus position.
Aseptic Technique
There appears to be a great degree of practice variation among anesthesia providers with respect to aseptic technique during administration of neuraxial anesthesia.39–41 This lack of consensus may result from an underappreciation of the gravity of infectious complications related to neuraxial anesthesia.42–44 Indeed the incidence of epidural abscess and spinal meningitis is generally so low that many of the available recommendations are based on evidence from other domains of infection control (e.g., surgical wound site and central venous catheter–related infection).45–47 Nonetheless, neurologic compromise resulting from neuraxial infection can be a devastating complication.
Infection of the epidural space tends to result in the formation of an abscess, most commonly formed by Staphylococcus aureus found in the epidermis of either the patient or the anesthesia provider. In contrast, meningitis associated with neuraxial procedures is most commonly caused by Streptococcus viridans. Viridans species of streptococcus may reside in the oronasopharyngeal tract of providers or patients or in the vagina. Potential routes of infection include the (1) epidural catheter track, (2) bloodstream, (3) equipment, and (4) injectate. A more in-depth discussion of neuraxial infection is found in Chapter 32.
Guidelines describing aseptic technique for regional and neuraxial anesthetic procedures have been published by professional anesthesiology organizations, including the ASA, the Association of Anaesthetists of Great Britain and Ireland, and the American Society of Regional Anesthesia and Pain Medicine.47–49 The following recommendations deserve emphasis:
1. Given that the oropharyngeal and skin flora of the anesthesia provider are implicated in many cases of neuraxial infection, the provider should don a surgical facemask and hat before initiation of spinal/epidural anesthesia. Microbial sampling in laminar-flow operating theaters has shown a 22-fold increase in bacterial counts when a facemask and hat are not worn.50
2. Washing hands with an alcohol-based antiseptic solution is recommended because this has been shown to be superior to antimicrobial soap.51 Jewelry (e.g., rings, watches) should be removed before and sterile gloves worn after hand cleansing.
3. The patient’s skin should be decontaminated, preferably with a chlorhexidine-in-alcohol solution.47 An abundance of evidence affirms the superior bacteriocidal and bacteriostatic efficacy of chlorhexidine compared with povidone-iodine.46,52 If chlorhexidine is not available, then povidone-iodine with alcohol, rather than povidone-iodine alone, is preferred.47,53 Of importance, the anesthesia provider is encouraged to exercise patience in allowing the antiseptic to dry, because a major mechanism of antisepsis is the desiccating action of alcohol.
Equipment and Placement of Needle/Catheter
Spinal Anesthesia
The first equipment decision involves determining whether to perform a single-shot or continuous technique. Continuous spinal anesthesia is not a new technique; indeed, some physicians performed continuous spinal anesthesia more than 50 years ago. Currently, a large-bore epidural needle and catheter must be used for continuous spinal anesthesia, because the U.S. Food and Drug Administration rescinded approval for the use of small-bore microcatheters in 1992.54 Therefore, the risk for post–dural puncture headache is significant. This technique is useful after unintentional dural puncture with an epidural needle. In the morbidly obese patient, it may be easier to manipulate and advance a rigid epidural needle than a more flexible spinal needle; thus the technique is useful for establishing continuous analgesia or anesthesia in this patient population, particularly when the need for anesthesia is urgent. However, for most obstetric patients, a single-shot technique is preferred for spinal anesthesia.
The primary equipment choice for spinal anesthesia concerns the type and size of the spinal needle. Cutting-bevel needles (e.g., Quincke) are rarely used in contemporary obstetric anesthesia practice because of the unacceptably high incidence of post–dural puncture headache associated with their use.55 Instead, non-cutting needles (e.g., Whitacre, Sprotte, Gertie Marx) are used almost exclusively (Figure 12-6). Some anesthesia providers refer to the non-cutting needles as “pencil-point needles.” It is now believed that the pencil-point needles cause more trauma to the dura, which then results in a more intense inflammatory response than occurs with cutting-bevel needles. Presumably, the inflammation results in more rapid closure of the dural defect.56
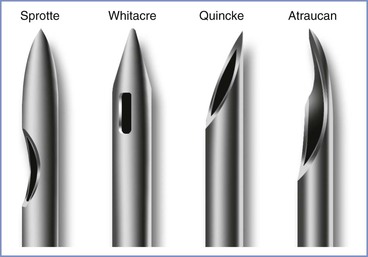
FIGURE 12-6 Spinal needle assortment often used in parturients. Each needle is shown in an open-bevel view and an oblique orientation. The Whitacre and Sprotte needles have cone-shaped bevels, whereas the Quincke has a cutting bevel. (Other sizes are available in some of these needle designs.)
Needle size must also be determined. Larger needles offer a greater fidelity of tactile feedback as the anesthesia provider traverses tissue planes of variable impedance when performing spinal anesthesia. Furthermore, larger needles are more likely to withstand the high resistance encountered when contacting bone without bending or shearing. In general, the “ease-of-use” advantages associated with larger needles must be balanced against a lower incidence of post–dural puncture headache with smaller needles. Most anesthesia providers use 25- or 27-gauge non-cutting needles for routine spinal anesthesia in obstetric patients. However, anesthesia providers should make individual decisions based on their own skills, practice setting, and the patient. The urgency of the procedure may also influence the choice of needle size. For example, a 27-gauge needle might be chosen for spinal anesthesia for an elective procedure, and a larger (e.g., 22-gauge) needle might be chosen when the subarachnoid space must be entered quickly because of severe fetal compromise.
With a small-gauge needle (i.e., 24-gauge or smaller), use of an introducer needle is preferable. The introducer needle engages the interspinous ligament and more accurately guides the trajectory of the smaller spinal needle than is possible with use of a small-gauge spinal needle alone. The introducer needle also aids with skin puncture; it is often difficult to puncture the skin with non-cutting needles.
Either the midline or the paramedian approach can be used to enter the subarachnoid space. The midline approach requires the patient to reduce her lumbar lordosis to allow access to the subarachnoid space between adjacent spinous processes (usually L3 to L4, sometimes L4 to L5 or L2 to L3). The interspinous space may be identified with one (usually the thumb or index finger) or two fingers (usually the index and middle fingers) of the anesthesia provider’s nondominant hand. The single finger “slides” along the skin in the midline from cephalad to caudad until it “settles” into an interspinous space. The two fingers identify the interspinous space by palpating the caudad border of the more cephalad spine. The fingers identify the midline by rolling in a medial-to-lateral direction (Figure 12-7).
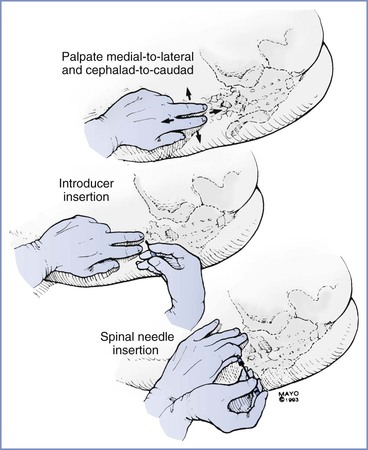
FIGURE 12-7 The midline approach for spinal needle insertion requires accurate identification of a lumbar interspinous space. The palpating fingers are rolled in a medial-to-lateral and cephalad-to-caudad direction; an introducer is then inserted through the interspinous space almost perpendicular to the lumbar spinous process. Once the introducer is seated in the interspinous ligament, the spinal needle is inserted; the needle is stabilized in a tripod fashion during insertion (much like a dart being thrown).
Next, the anesthesia provider injects local anesthetic intradermally and subcutaneously. The introducer needle is inserted into the substance of the interspinous ligament. It is helpful if the introducer needle is embedded in the interspinous ligament; therefore, obese patients may require a longer introducer needle. The introducer needle should lie in the sagittal midline plane. It is then grasped and steadied with the fingers of the nondominant hand while the dominant hand holds the spinal needle like a dart. The fifth finger may be used as a tripod against the patient’s back to prevent patient movement from causing unintentional needle insertion to a level deeper than intended, and to “brake” the needle. As the needle passes through the ligamentum flavum and the dura, characteristic changes in resistance are noted. A “pop” is often perceived as the needle tip traverses the ligamentum flavum. A subsequent and more pronounced pop is perceived as the needle tip exits the dura-arachnoid. The stylet is removed, and CSF should appear in the needle hub. If CSF does not appear, the stylet is replaced, and the needle is advanced a few millimeters and again checked for CSF flow. This process continues until either bone is encountered or CSF returns through the needle. If neither occurs, the needle and introducer are withdrawn and the process is repeated.
Although with time and practice the tactile feedback produced by advancing a needle through tissues of variable resistance will become utterly familiar to the anesthesia provider, the novice may be unsure of the anatomic position of the needle tip, especially if unexpected resistance (i.e., contact with bone) or an unexpected and premature “pop sensation” is encountered during needle advancement. A stepwise problem-solving approach is reasonable. First, the anesthesia provider should reconfirm that (1) the patient has normal anatomy (i.e., not scoliotic), (2) she is acceptably positioned at an appropriate height for the anesthesia provider, and (3) the chosen point of needle insertion is the true midline plane. If these assertions are true, and the needle tip encounters bone, it is highly likely that the osseous structure is either the inferior or superior spinous process. One of two maneuvers may overcome this barrier. After slight withdrawal of the needle, simple angulation in a cephalad or caudad direction may redirect the needle trajectory sufficiently to achieve access to the central neuraxial canal. One must appreciate the “toughness” of the interspinous ligament. Even a 17-gauge epidural needle can be bent if the angle is changed without some prior retraction of the needle. Furthermore, if a spinal needle/introducer complex is used, care must be exercised that angulation of the spinal needle does not occur without first withdrawing it into the lumen of the introducer. Thereafter, the entire spinal needle/introducer complex is angulated before the spinal needle is re-advanced. Angulation of the spinal needle without first withdrawing it into the introducer creates a fulcrum at the junction of the introducer tip where the spinal needle emerges and can potentially damage or even shear the delicate spinal needle (Figure 12-8).57
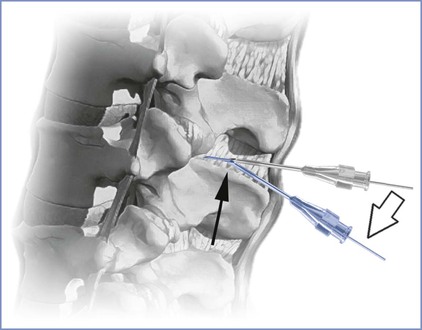
FIGURE 12-8 Change of needle trajectory during spinal anesthesia. Note that if both the spinal needle and its introducer needle are manipulated without prior retraction of the spinal needle into the lumen of the introducer (open arrow), a fulcrum is created (dark arrow) where the risk for bending or shearing the delicate spinal needle may occur. (Drawing by Naveen Nathan, MD, Northwestern University Feinberg School of Medicine, Chicago, IL.)
Alternatively, the needle may be withdrawn fully into subcutaneous tissue and either raised or lowered (cephalad or caudad) while still maintaining an angulation that is parallel to the original trajectory. Which approach is more effective may depend on the reason for the initial bone contact. If the patient has very narrow interspaces, then careful raising or lowering of the needle while maintaining a trajectory parallel to the floor may be appropriate. However, if the patient is overly flexed forward, it is possible that her lumbar spinous processes are projecting in a slightly upward angulation (relative to the perpendicular transverse plane). This may require that the needle be re-angulated accordingly. If bone is still encountered despite all these considerations, it is likely that the needle tip is in fact not in the midline plane and is contacting the vertebral lamina. This may occur if the initial skin puncture is not in the midline, the needle tip deviates from the midline as it is advanced, or the patient’s spine is rotated (either from poor positioning or scoliosis). Clues that the needle tip is not midline include (1) the patient complaining of lateralizing pain, (2) lack of CSF flow despite appropriate needle depth, and (3) the perception of “soft” or “mushy” tissue during needle advancement (paraspinous tissue) rather than the more “rigid” ligamentous tissue, or even a false “pop” as the needle tip exits the interspinous ligament laterally into paraspinous tissue. Much like the progressive modifications described earlier for correct alignment in the superoinferior plane, so too can these approaches be employed for redirecting in the lateral plane (Figure 12-9). The novice is advised to make systematic changes in a stepwise fashion, rather than indiscriminately changing needle direction without first considering the anatomic problem.
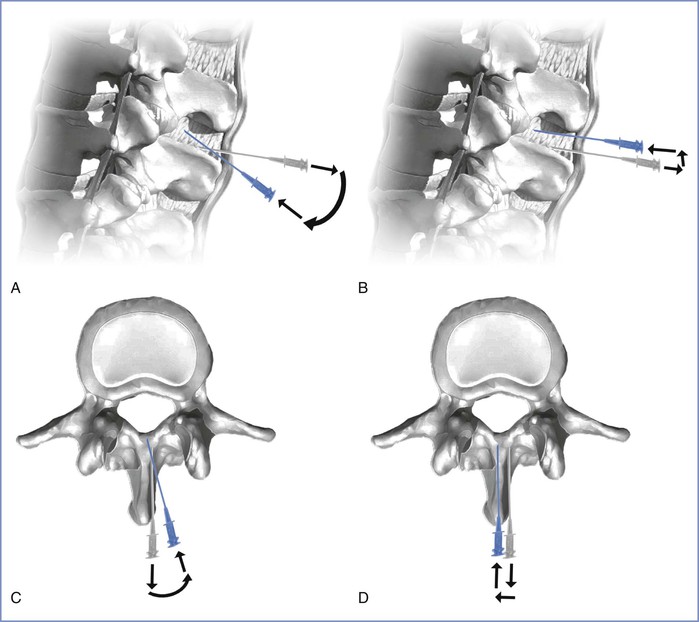
FIGURE 12-9 Troubleshooting contact with bony structures during needle placement. The gray needle represents the initial needle trajectory; the blue needle represents the adjusted needle trajectory. A, Assuming correct midline needle placement, the needle can be retracted slightly and angulated to overcome a spinous process. B, Alternatively, the needle may be “lifted” after slight retraction while keeping the original trajectory constant. C, Assuming the needle is deviating from the midline plane and contacting lamina, an action similar to that in A may be executed. D, Alternatively a stepwise lateral shift similar in concept to that shown in B may correctly achieve midline alignment. (Drawing by Naveen Nathan, MD, Northwestern University Feinberg School of Medicine, Chicago, IL.)
Once CSF is freely dripping from the needle hub, the dorsum of the provider’s nondominant hand steadies the spinal needle against the patient’s back while the syringe with local anesthetic is attached to the needle. After aspirating to ensure the free flow of CSF, the anesthesia provider injects the local anesthetic at a rate of approximately 0.2 mL per second. After completion of the injection, some anesthesia providers again aspirate approximately 0.2 mL of CSF and reinject it into the subarachnoid space. This last step reconfirms the needle location and clears the needle of the remaining local anesthetic. The patient is then repositioned as appropriate.
For most patients, the midline approach is faster and less painful than the paramedian approach. The midline approach is also easier to teach than the paramedian approach, because it requires mental projection of the anatomy in only two planes, whereas the paramedian approach requires appreciation of a third plane and estimation of the depth of the subarachnoid space from the skin (Figure 12-10).
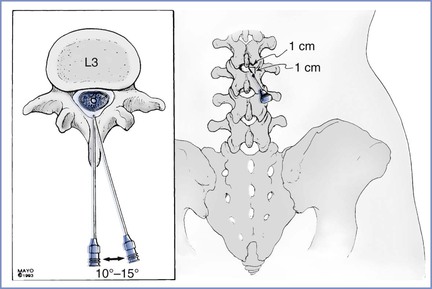
FIGURE 12-10 Vertebral anatomy of midline and paramedian approaches for spinal and epidural anesthesia. The midline approach requires anatomic projection in only two planes: sagittal and horizontal. The paramedian approach also requires consideration of the oblique plane. However, the paramedian approach requires less patient cooperation in reducing lumbar lordosis to allow for successful needle insertion. The paramedian needle insertion site is made 1 cm lateral and 1 cm caudad to the caudad edge of the more cephalad spinous process. The paramedian needle is inserted 10 to 15 degrees off the sagittal plane (inset).
Nevertheless, the paramedian approach is a useful technique that allows for the successful identification of the subarachnoid or epidural space in difficult cases. The paramedian approach does not require that the patient fully reduce her lumbar lordosis. This approach exploits the larger target that is available when the needle is inserted slightly off the midline.
A common error that is made with the paramedian approach is the insertion of the needle too far off the midline; the vertebral lamina then becomes a barrier to needle insertion. With the paramedian approach, the palpating fingers should again identify the caudad edge of the more cephalad spinous process. A skin wheal is raised 1 cm lateral and 1 cm caudad to this point; a longer needle is then used to infiltrate the deeper tissues in a cephalomedial plane. This step contrasts to the midline approach, in which the local anesthetic is not injected beyond the subcutaneous tissue. The spinal introducer is then inserted 10 to 15 degrees off the sagittal plane in a cephalomedial direction, and the spinal needle is advanced through the introducer needle toward the subarachnoid space. Another common error is to use an excessive cephalad angle with initial needle insertion. When the needle is inserted correctly and contacts bone, it is redirected slightly cephalad. If bone is again encountered, but at a deeper level, the slight stepwise increase in cephalad angulation is continued, and the needle is “walked” up and off the lamina. As with the midline approach, the characteristic feel of the ligamentum flavum and dura can be appreciated. The aim of the paramedian approach is to puncture the dura in the midline, even though the needle is inserted off the midline. Use of the paramedian approach requires insertion of a greater length of needle. Once CSF is obtained, the block is performed as it is with the midline approach.
During the performance of any nerve block technique, needle advancement should stop if the patient complains of pain. If pain is the result of inadequate soft tissue anesthesia, additional local anesthetic should be injected. Pain or paresthesias may also result from needle contact with central nerves or the spinal cord. Patient perception of paresthesias during the initiation of spinal anesthesia may indicate that the needle tip is in the subarachnoid space. The anesthesia provider should remove the stylet and check for CSF. If the paresthesia has resolved, the local anesthetic may be injected. If the paresthesia persists, however, the needle should be withdrawn and repositioned. In any case, the anesthesia provider should never inject the local anesthetic if the patient is complaining of paresthesias or lancinating pain, either of which may signal injection into a nerve or the spinal cord.
Epidural Anesthesia
Special equipment for epidural analgesia or anesthesia includes an epidural needle, an epidural catheter (for a continuous technique), and a loss-of-resistance syringe (for the loss-of-resistance technique to identify the epidural space). Single-shot epidural anesthesia is rarely used in obstetric practice, because the major advantage of epidural over spinal anesthesia is the ability to provide continuous anesthesia or analgesia without puncturing the dura with a large needle. An epidural needle with a lateral opening (e.g., Hustead, Tuohy) is most commonly used because it allows a catheter to be threaded through its orifice (Figure 12-11).
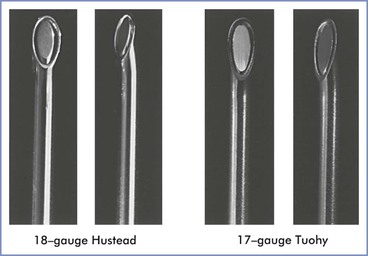
FIGURE 12-11 Epidural needles often used in parturients. Each needle is shown in an open-bevel view and an oblique orientation. The 18-gauge Hustead and 17-gauge Tuohy needles have lateral-facing openings, which direct epidural catheters to enter the epidural space more easily than if a single-shot Crawford needle design is used. (Other sizes and needle designs are available for obstetric epidural anesthesia.)
Two methods are used to identify the epidural space during needle advancement: (1) hanging drop method and (2) loss-of-resistance method. The majority of anesthesia providers use the loss-of-resistance method (Figure 12-12).
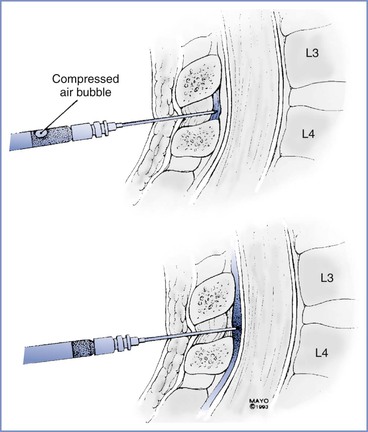
FIGURE 12-12 Loss-of-resistance technique for identifying the epidural space. The needle is first inserted into the interspinous ligament or ligamentum flavum, and a syringe containing an air bubble in saline is attached to the hub. After compression of the air bubble by pressure on the syringe-plunger, the needle is carefully advanced until a loss of resistance to syringe-plunger pressure is noted as the needle enters the epidural space.
The traditional loss-of-resistance syringe is a finely ground glass syringe with a Luer-Lok connector. Plastic syringes are now available, and the choice is generally a matter of the anesthesia provider’s preference. The syringe is filled with 2 to 4 mL of saline, air, or saline with a small (0.25 to 0.5 mL) air bubble. There is some controversy regarding the use of air versus saline for detecting the point of loss of resistance.58 Saline causes some syringe plungers to stick and may be confused with CSF during initiation of CSE anesthesia. Conversely, injection of air into the epidural space may contribute to patchy anesthesia,59 and unintentional pneumocephalus may increase the risk for post–dural puncture headache.60
Prior investigations have suggested superiority of loss-of-resistance with saline over air with respect to block success. This conclusion is further supported by the results of a meta-analysis that pooled six controlled trials (n = 1037) in which laboring women were randomized to receive loss-of-resistance to air versus liquid (saline or local anesthetic solution).61 This analysis suggested an increased risk for unblocked segments when loss-of-resistance to air was used, presumably owing to air bubbles leaking through the intervertebral foramina and residing adjacent to nerve roots.62
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree