Slit Lamp Examination
Alex V. Levin
Introduction
Slit lamp biomicroscopy is a diagnostic procedure that requires experience and specific skills. It is unlikely that the majority of pediatricians and emergency physicians will have the opportunity to repetitively use the slit lamp enough to acquire and refine the skills needed to use it well in many situations. Therefore, this chapter will address the basic theory and practice of slit lamp illumination, along with a few common applications that may fall into the scope of practice of nonophthalmologists treating children in the emergency setting. It would of course be appropriate to seek ophthalmology consultation whenever the physician does not feel comfortable using the slit lamp, the diagnosis remains in question, or the evaluation and treatment of the patient requires slit lamp techniques beyond the basics discussed herein.
Purchasing a slit lamp is an individual decision that should take into account cost, need, and frequency of use. If it is unlikely to be used often, then it is unlikely that the physicians will have the opportunity to acquire the skills necessary for proper use. In this setting, it may be more harmful than beneficial. The slit lamp is best placed in a dedicated area, with an adjustable patient chair and with ocular medications, forceps, and cotton swabs readily available. Purchasing a slit lamp on wheels is an alternative. Another consideration is the utility of having the slit lamp available on-site for the consulting ophthalmologist. In some situations, this may obviate the need for the patient to make a trip to the ophthalmologist’s office and may allow the ophthalmologist to optimize the examination on-site.
Anatomy and Physiology
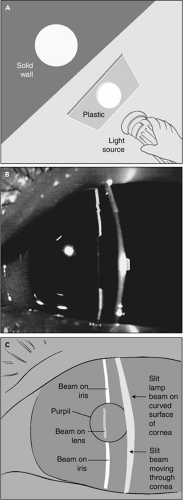
Light can only be seen when it is reflected off an object. If a person were to hold a flashlight and shine it into an endless vacuum, the beam of light emanating from the bulb would be invisible. Only if a person were to place a substance or object within the path of the light would the light become visible. For example, if smoke or dust were allowed to enter our theoretical vacuum, the beam of light would readily become apparent, as it would be reflected by the particles. This is called the Tyndall phenomenon. Likewise, if a person were to erect a piece of semitransparent plastic several centimeters thick in the vacuum and then several meters thereafter erect a cement slab, the beam of light would become visible as it strikes the plastic, as it moves through the plastic (being reflected by the continuous substance of the plastic), and again as it hits the opaque cement slab (Fig. 46.1A). Because the vacuum itself contains no reflective materials, the beam would remain invisible at all other places.
These principles are directly applicable to the eyeball. If a person shines a beam of light (in this case, the slit lamp beam) into the eyeball, it will only be visible where it is reflected. Between the bulb and the eyeball it is invisible, as, for the most part, air is relatively nonreflective from an optical standpoint. However, as the beam hits the surface of the cornea, it can be seen (Fig. 46.1B,C). As it passes through the corneal substance, it is continuously visible, just as the light passing through the plastic in the previous example would be continuously visible. The beam then becomes invisible as it leaves the back of the cornea and travels to the surface of the iris, where it is once again reflected and therefore becomes visible to the observer. The space between the back of the cornea and the iris (anterior chamber) is filled with optically clear fluid (aqueous humor), which prevents the beam from being visualized. The pupil is simply a hole in the iris through which the beam continues to pass, invisible to the observer until it strikes the front surface of the lens, which is just beyond the pupil. Again, the beam becomes visible as it hits the surface of the lens and passes through the substance of
the lens. Visualization of the interior of the lens is difficult without pharmacologic dilation of the pupil, but the anterior surface is easily seen with the pupil in its usual state. After pupillary dilation, the skilled observer can also visualize strands of vitreous behind the lens. Using special lenses, the ophthalmologist also can direct the slit lamp beam to allow visualization of the posterior vitreous, optic nerve, and retina.
the lens. Visualization of the interior of the lens is difficult without pharmacologic dilation of the pupil, but the anterior surface is easily seen with the pupil in its usual state. After pupillary dilation, the skilled observer can also visualize strands of vitreous behind the lens. Using special lenses, the ophthalmologist also can direct the slit lamp beam to allow visualization of the posterior vitreous, optic nerve, and retina.
The slit lamp is given its name because of its ability to create a slit beam of light. Using a slit allows for a topographic appreciation of each surface because the light appears to bend along the curvature of that surface. The observer can appreciate the corneal curvature, the iris architecture, and the curved surface of the lens (Fig. 46.1). In disease states, the observer can assess the elevation and contour of ocular structures. For example, a foreign body on the cornea would cause an elevation of the beam as it bends to go over the material. The slit beam also allows for the delineation of the internal anatomy of translucent structures such as the cornea and lens. The skilled observer can visually distinguish the corneal layers and therefore recognize the depth of a lesion, such as foreign body or corneal laceration.
When the aqueous humor loses its optical clarity, the beam of light becomes visible as it passes from the cornea to the iris and lens. This occurs with iritis and hyphema. The white blood cells and protein that leak out of inflamed iris vessels in iritis and the red blood cells of a hyphema reflect the beam to the observer so that the particles can actually be seen floating in the aqueous, similar to the beam of an automobile headlight in the fog. The visualization of red or white blood cells is called “cells” and graded on a scale of 1+ to 4+ by an experienced examiner. The presence of protein is referred to as “flare” and graded on a similar scale.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree