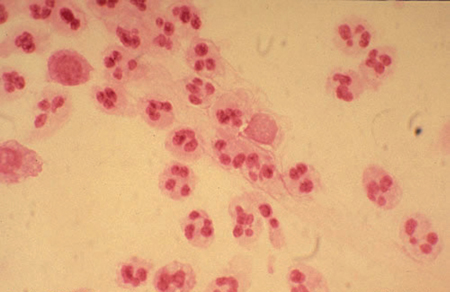
31 Sexually Transmitted Diseases Tanya S. Ghatan Sexually transmitted diseases (STDs) represent a major public health problem, and complications from untreated disease can have serious medical consequences. A thorough sexual history is important for effective screening. The Centers for Disease Control and Prevention (CDC) recommends the five “P’s”: Partners, Prevention of pregnancy, Protection from STDs, Practices, and Past history of STDs. It is also important to elicit information about any new sexual partners, history of multiple partners, types of sexual exposure, and condom use. STD screening must be done in a nonjudgmental manner. Common risk factors for all STDs include young age, African-American race, a new sexual partner, multiple partners, history of prior STD, and illicit substance abuse. The causative agent is Neisseria gonorrhoeae. Gonococcal infections represent one of the most common sexually transmitted diseases worldwide with approximately 700 000 infections in the United States annually. Risk factors for acquisition include, but are not limited to, low socioeconomic status, early onset of sexual activity, and substance abuse. There is an unequal transmission rate between sexes, with the male-to-female transmission rate as high as 80–90% compared with 20–25% for female to male. Infection occurs primarily at the columnar epithelium of the genital tract. The transitional epithelium of the urinary tract is a second location of infection. Symptoms may include cervical purulent discharge, urinary frequency, dysuria, and occasionally rectal discomfort. Many women may have mild to no symptoms. Complications from Gonorrhea may develop regardless of the severity of symptoms. Gonorrhea is a common cause of pelvic inflammatory disease, which in turn can lead to long-lasting pain and infertility. Currently, DNA probes from either cervical swabs or urine are used to diagnose the infection. Other, less common methods of diagnosis are culture or Gram stain. Neisseria gonorrhoeae is a Gram-negative diplococcus described as “paired kidney beans” (Fig. 31.1). Standard treatment is a single dose of ceftriaxone 250 mg intramuscularly. Additionally patients should be treated for Chlamydia if it has not been ruled out secondary to a high incidence of concurrent infection. Fig. 31.1 Gonoccocus “Gram-negative diplococcus.” Source: University of Washington (Seattle STD/HIV Prevention Training Center). The causative agent is Chlamydia trachomatis. Chlamydia is the most frequently reported STD in the United States. There is an approximately 2.2% prevalence rate of chlamydial infections with 1 030 911 infections reported to the CDC in 2006. Many women are asymptomatic and therefore do not seek testing or treatment. Risks factors for acquisition are the same as for Gonorrhea and include early onset of sexual activity, multiple sexual partners, a new sexual partner within the previous three months, low socioeconomic status, and a history of a prior STD. Chlamydia may present as an ocular, respiratory or genital tract infection (Fig. 31.2). Chlamydia is primarily acquired through sexual contact although, rarely, vertical transmission may be seen. The organism attaches to columnar epithelial cells in the genital tract. Symptoms usually appear within 1–3 weeks of exposure. Symptoms include mucopurulent cervical discharge, hypertrophic friable cervix, and acute urethral syndrome. Genetic probes are utilized for diagnosis. Cell culture is the “gold standard” but is difficult and requires at least seven days. Standard treatment is either a single oral dose of azithromycin 1 g or doxycycline 100 mg twice daily for 1 week. Complications can involve salpingitis leading to infertility, pelvic pain, and ectopic pregnancy. In neonatal infections conjunctivitis and otitis media are common complications. Fig. 31.2 Chlamydial Cervicitis Source: Conni Cellum and Walter Stamm (Seattle STD/HIV Prevention Training Center). Annual screening for Chlamydia is recommended for all sexually active women under the age of 25 years. In addition, older women with risk factors and pregnant women should be screened. The spirochete Treponema pallidum is the causative agent. Infections are primarily sexually transmitted. The spiro-chetes enter through abrasions on the skin and mucosal surfaces, where they then replicate (Fig. 31.3). Syphilis may be divided into initial, secondary, and tertiary stages with different symptoms, complications, and treatment for each stage. Syphilis lesions may resolve spontaneously and the patient may remain asymptomatic during any stage of the disease. The initial lesion or “chancre” is approximately 1 cm in size. It is painless, red and round with raised edges. The chancre appears 3 weeks after exposure, although it may have a 10–60-day incubation period. The chancre will heal without treatment, but the disease will still progress to the secondary stage. The secondary stage may appear 1–3 months after the primary lesion has resolved. It represents a disseminated infection. The typical maculopapular rash occurs on the palms and soles of the feet. The dermatologic lesions may be diverse resulting in syphilis being known as the “great imitator.” Malaise, headache and anorexia are also often present. Syphilis passes into a latent phase upon completion of the secondary stage. This may last for years before tertiary syphilis develops. This allows transmission of syphilis from those who are unaware that they are themselves infected. Tertiary syphilis is rare in the United States. The pathognomic lesions are granulomas or gummas of the bone and skin representing lesions of necrotic, ulcerative nodules. Other complications of syphilis include neurosyphilis with tabes dorsalis and aortitis. Fig. 31.3 Primary Syphilis lesion The spirochetes can be identified utilizing dark-feld microscopy, although this is now rarely used for diagnosis. Screening occurs with a nonspecific antibody test. Examples of these are the RPR (rapid plasmin regain) and the VDRL (venereal disease research laboratory) tests. Following a positive screening test infection is confirmed with a specific treponemal test, such as the microhemagglutination assay for Treponema pallidum
Screening and Risk Factors
Non-Ulcerative Lesions
Gonorrhea
Chlamydia

Ulcerative Lesions
Syphilis

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


