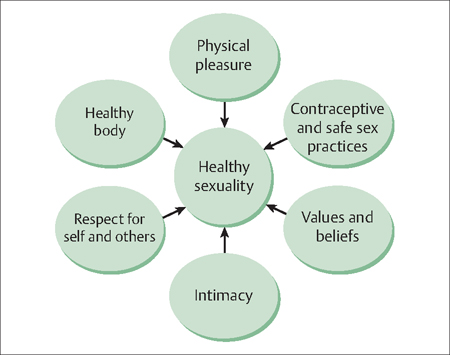
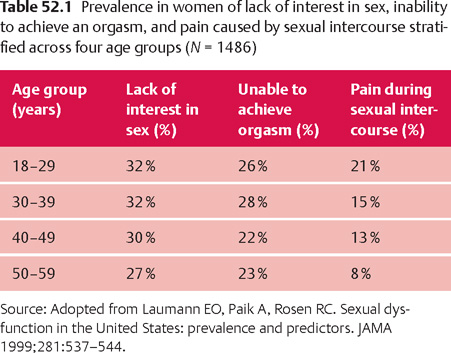
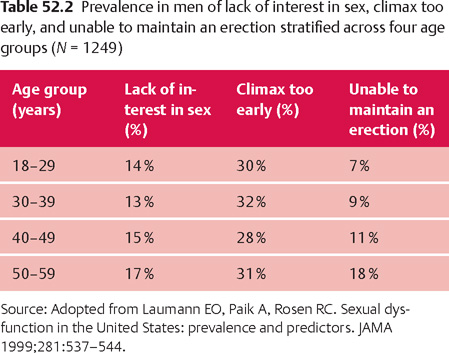
52 Sexuality Robert L. Barbieri Sexuality is a central part of human experience (Fig. 52.1). Sexual dysfunction is the inability to participate as desired in a sexual relationship. The causes of sexual dysfunction are complex. Problems of sexual function are best approached with a biopsychosocial model that recognizes the important contribution of biological, psychological, and social-cultural factors in sexual health. Across mammalian species, haploid gametes can be reliably assigned to two categories: sperm (male), and oocytes (female). In contrast, it is not possible to assign all people to parallel, rigid, sexual identities such as male and female. Sexual identity is more plastic than biological or anatomical sex. Many people have blended sexual identities that combine features of male and female sexuality. In addition, about 1 in 10 000 people who are genetically and anatomically male, strongly prefer a female sexual identity, and vice versa. Trans-sexuals are estranged from their own sex organs and seek a gender identity of the opposite sex. Transgendered individuals are estranged from their own sex organs but do not desire to seek full reassignment to the opposite sex, and seek an in-between sexual status. Among many mammalian species, during embryonic development and fetal life, the brain is programmed toward a male or female pattern of sexuality. The programming is manifested in morphologic diferences in brain nuclei and is associated with sex-specific behaviors such as copulatory positions. The programming occurs in fetal life and the dimorphic patterns of behavior become observable after being activated by the hormones of puberty. Fetal androgens appear to play a major role in causing differentiation of the brain nuclei to a male pattern. In humans, fetal programming is influenced by events in childhood and adolescence. Fig. 52.1 Health sexuality is the product of multiple dimensions. Masters and Johnson posited that in men and women there are four stages of sexual response: excitement, plateau, orgasm, and resolution. Building on this linear model of sexual response, later investigators replaced excitement with two phases: desire, and arousal. This culminated in a five-stage linear model of sexual response: Recent models of sexual response have emphasized that a circular model, where sequential responses overlap and build on previous stimuli, may be more accurate. Recent models also emphasize the importance of emotional intimacy and the quality of the relationship between the two partners in the achievement of sexual health. Sensory input and psychological fantasy stimulate the arousal response. In men, sexual arousal is anatomically evident by the development of penile tumescence or erection. In women arousal may result in vasocongestion of the clitoris, vagina, vulva, breasts and areola, transudation of vaginal fluid, and nipple erection. In men orgasm is manifested by contractions of the vas deferens, seminal vesicles, and prostate followed by contractions of the urethra and penile base muscles, which accompanies ejaculation. In women orgasm most often occurs separately from sexual intercourse, with manual or oral stimulation of the clitoris. In women, during orgasm the upper one-third of the vagina tents and becomes enlarged, while the lower one-third of the vagina narrows from muscular contractions involving the perineal, bulbocavernosus, and pubococcygeal muscles. Sexual dysfunction is the presence of disturbances in sexual desire and/or in the psychophysiological changes associated with the sexual response cycle. Approximately 40% of women and 30% of men report sexual dysfunction. Common problems reported by heterosexual women are: 1) a lack of interest in sex; 2) an inability to achieve orgasm; 3) pain caused by sexual intercourse; 4) lack of pleasure with sex; and 5) trouble lubricating (Table 52.1). Common problems reported by heterosexual men are: 1) lack of interest in sex; 2) orgasm occurs too early; 3) trouble maintaining an erection; 4) inability to achieve orgasm; and 5) anxiety about sexual performance (Table 52.2). In both men and women, poor overall health, mental health problems, poverty, and a history of sexual abuse increase the risk of sexual dysfunction. The majority of women and men will not volunteer to their clinician that they are having sexual problems. In one study only 3% of patients volunteered that they had a sexual problem, but when the same group of patients was directly asked by their clinician about sexual issues, 20% reported a sexual problem. It is important for clinicians to provide a supportive environment to discuss sexual problems, and to actively inquire about their presence. If a sexual disorder is identified, it may be helpful for the clinician to explicitly comment that these disorders are common in their practice and that it can be difficult for patients to openly discuss intimate sexual issues, but that by discussing these issues improvement will likely occur. The sexual history may be initiated by asking, “Do you have any concerns about your sex life?” Additional open-ended questions that may be helpful include: Are you having sexual relations currently? With men or women or both? If you are not having sex, when did you last have intercourse? Are you satisfied with the frequency and quality of your sexual experiences? How many sexual partners do you have? What is the emotional quality and intimacy of your relationship with your sex partner(s)? A more thorough approach to the sexual history is presented in Table 52.3. If a sexual concern is identified, the patient should describe her problem in detail, in her own words. Many women will report that they have decreased “libido,” but on further questioning an orgasm or pain disorder is identified. Asking the patient to describe in detail a typical sexual interaction with her partner can be helpful too: Who initiates sexual play? What is the frequency of sexual relations? Are you feeling receptive when your partner initiates sexual play?
Sexual Identity
Sexual Response in Men and Women
Sexual Dysfunction in the General Population
The Sexual History
| Approach to the patient |
| Sexual function is influenced by many factors including biological, psychological, and social factors Most sexual problems are best approached using a biopsychosocial model |
| Chief Complaint and creation of a supportive environment |
| Elicit, in her own words, the concern the patient has with sex and sexual function What problems are present in most situations? Have you had a change in your interest in sex? Do you have trouble becoming aroused or sufficiently lubricated? Are you able to have an orgasm by self-stimulation or with your partner? Do you have pain with sex? |
| Use open-ended questions Explicitly acknowledge the potential embarrassment of the topic Reassure the patient that sex problems are common Counsel the patient that it is good to address these issues |
| Biological factors |
|
| Psychological factors |
|
| Social factors |
|
The patient’s medical history should also be assessed, because many chronic illnesses (diabetes, hypertension, cardiovascular diseases, cancer, neurologic disease), mental health issues (depression, anxiety), pain syndromes, or previous pelvic surgery (cystocele, rectocele repair) may influence sexual function. Many cardiovascular and mental health medications can contribute to sexual dysfunction.
A paper-based sexual function questionnaire, the Female Sexual Function Index, is available at the Web site: http://www.fsf-questionnaire.com/, along with a scoring system. The 19 question instrument permits the differentiation of disorders of desire, arousal, lubrication, orgasm, satisfaction, and pain.



