Inflammatory bowel diseases (IBD), most commonly Crohn’s disease and ulcerative colitis, have the highest incidence during the reproductive years. IBD and its treatments increase the risk of sexual dysfunction for both men and women with these diseases. Women with IBD often seek care from their gynecologist and may preferentially discuss sexual experiences with them over other providers. An understanding of IBD and its impact on sexual functioning and satisfaction will improve screening, evaluation, and management for these patients. Identifying interdisciplinary providers for referrals, such as pelvic floor physical therapists and health psychologists, is a key component to long-term improvements in sexual satisfaction for women with IBD.
Inflammatory bowel diseases (IBD) are chronic, relapsing, and remitting autoimmune disorders made up of Crohn’s disease, ulcerative colitis, and, in a small proportion of individuals, indeterminate colitis. The peak age of incidence is between 15 and 30 years, coinciding with peak reproductive years for women. There are 1.6 million Americans affected by these diseases and 70,000 new cases annually, with increasing incidence and prevalence worldwide. The spectrum of symptoms and anatomic location of the disease is different for each patient and directs treatment choices. Treatment primarily consists of medical management of symptoms with immunosuppressant agents, although surgery may be indicated for bowel obstruction or perianal fistulas. Surgical treatment may even be curative in certain cases, as in a colectomy for ulcerative colitis patients. The extraintestinal manifestations, such as chronic fatigue, mood changes, or sexual dysfunction, are common–even when the disease is in remission. As reproductive-age women with IBD regularly see both their gastroenterologist (GI) and an obstetrician-gynecologist (OBGYN), coordination of care to screen for and manage sexual dysfunction can improve quality of life in those diagnosed with this chronic, lifelong condition.
Background
Female sexual response cycle
Research in female sexuality is a dynamic and evolving field. Pioneers in female sexuality research first proposed a 4-stage linear model of the female sexual response cycle in the 1960s. The 4 stages included excitement/arousal, plateau, orgasm, and resolution. A decade later this linear model was amended to include desire. A more recent understanding of the biopsychosocial aspects of female sexual experiences placed an increasing emphasis on pleasure, satisfaction, emotional intimacy, sexual stimuli, relationship structure, and relationship satisfaction. These contemporary views of the female sexual response cycle acknowledge that women may enter into sexual activity for reasons other than sexual desire and allow for an expanded understanding of sexual activity for the purpose of personal satisfaction, which includes physical, emotional, and social satisfaction, rather than just orgasm alone.
Sexual response in female subjects is complex and coordinated by neuroendocrine mechanisms and vascular systems. The results are increased blood flow and lubricating secretions from the vasculature and the potential for a peak sensation (orgasm) accompanied by a release of opioids, serotonin, prolactin, and oxytocin. These response patterns are also impacted by personal sexual experiences, including cultural norms, societal and religious beliefs, general health status, interpersonal relationships, physical health, and previous personal experiences. Sexual problems can emerge if there is a breakdown in any point in the female sexual response cycle.
Epidemiology of sexual dysfunction
The epidemiology of female sexual dysfunction (FSD) is diffuse and understudied, yet the prevalence of sexual problems among women is common. In the United States around 40% of women report some form of sexual problems at different times in their lives. However, less than a quarter (12–25%) of women who report some difficulty with their sexual response associate it with personal distress , which is one of the diagnostic criteria for FSD. The prevalence of FSD increases as women age, with peak incidence among women aged 40–60 and among women who have recently undergone surgical menopause. The etiology of FSD may also include chronic diseases (as in IBD), which affect mobility, activity, and body image. Prior physical or sexual abuse, minor ailments, or medications can also play a role in FSD.
Classification of female sexual disorders
“Female sexual dysfunction” is the general term for disturbances in women’s sexual functioning. There are 3 major categories of FSD: (1) sexual desire/arousal disorders, (2) orgasmic disorder, and (3) genito-pelvic pain/penetration disorder.
Hypoactive sexual desire disorder (HSDD) is the most common sexual desire disorder and is defined as a deficiency or absence of sexual fantasies and desire for sexual activity that causes marked distress or interpersonal difficulty. The prevalence of HSDD ranges between 5% and 14% and the diagnosis is more common among perimenopausal women. HSDD is associated with situational circumstances, including relationships, chronic disease, gynecological disorders, and the use of certain medications among younger women. Antidepressants, corticosteroids, and oral contraceptives are also associated with HSDD. Sexual arousal disorders are an inability to maintain adequate lubrication throughout sexual activity, resulting in interpersonal difficulty or marked distress. In US population studies, 5% of women report significant difficulty with sexual arousal. Sexual arousal disorders are commonly associated with other dyspareunia disorders that impair normal sexual functioning.
Orgasmic disorders are reported among 3–6% of the population. These disorders include both primary orgasmic disorder, among women who have never had the ability to achieve orgasm either alone or during partnered sexual activity; and secondary orgasmic disorder, which involves a persistent delay in or absence of orgasm after normal arousal. Secondary orgasmic disorder is commonly associated with HSDD and has many of the same mitigating factors, including psychosocial contribution, general health, and/or certain medications.
The final category of FSD is sexual pain/penetration disorder. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) merges pain, pelvic floor tightening, and fear or anxiety of potential pain with vaginal penetration into diagnosis criteria for this disorder. This category is where a careful evaluation by an OBGYN will guide treatment planning.
Inflammatory bowel diseases and sexual function
Epidemiology in IBD
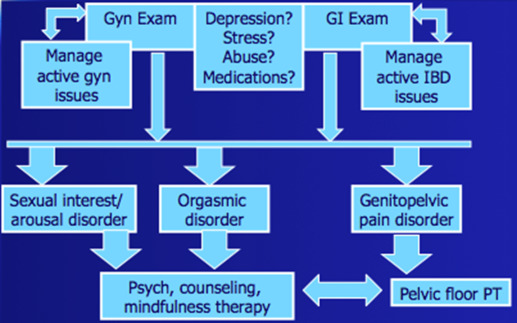
It is not surprising that IBD should affect sexual function, given the multiple medications, surgeries, and debilitating symptoms, such as perianal fistulas, diarrhea, incontinence, and abdominal pain, that patients experience. Several studies have shown that 40–60% of women and 44% of men with IBD report sexual dysfunction. The Crohns and Colitis Foundation of America (CCFA) Partners, an ongoing large Internet cohort study of 12,000 patients with IBD, is helping to determine the prevalence of the problem. In a survey of 2151 patients with active IBD, 80% indicated that symptoms affected their sexual satisfaction, and decreased sexual satisfaction correlated with increased disease activity. Patients desire information from their healthcare providers on this issue; 61% of women and 46% of men wanted information about the impact of IBD on intimacy and sexuality at the time of IBD diagnosis. Yet, only 40% of patients had discussed these concerns with their doctor. There is an additional reluctance in both male and female patients to discuss this topic when there is a physician-patient gender mismatch. The role of interdisciplinary care and communication between the GI, OBGYN, and, potentially, the colorectal surgeon could help fill the gaps and meet the patient’s needs on this sensitive issue ( Figure ).
Sexual function screening
Guidance on the diagnosis and evidence-based management of female sexual dysfunction is limited. A panel of experts convened in 2010 for the 2nd International Consultation on Sexual Medicine to update recommendations based on current data. The consensus statement from this meeting highlights the importance of screening for sexual dysfunction using a biopsychosocial context that assesses both the patient’s and her sexual partner’s experiences. A comprehensive medical and psychosocial history should be undertaken, including experiences with sexual abuse, depression, substance abuse, and the degree of distress associated with sexual experiences. The committee recommended further revision of definitions of FSD and prioritized future research goals, including multidisciplinary approaches.
Since the prevalence of sexual dysfunction is reported at around 50% in IBD patients, screening should be a part of health maintenance. Validated FSD screening tools exist, such as the Female Sexual Function Index, yet each tool has its limitations when administered to women with a chronic disease and ongoing interventions. Although there is no validated screening system specific to IBD, we propose several questions more specific to the disease and its treatments that can be administered by any healthcare provider:
“IBD and its management can sometimes interfere with a woman’s sexual life.”
Are you bothered by symptoms such as…
- –
Fear of passing stool during intercourse
- –
Painful intercourse (dyspareunia)
- –
Embarrassment due to setons (used to drain a sinus/fistula/abscess)
- –
Inhibitions due to stoma
- –
Embarrassment in addressing these issues with partner/healthcare provider
If any of these responses is positive, the provider can work with the patient to determine which risk factor or factors the patient has for sexual dysfunction and engage interdisciplinary support to meet the patient’s needs.
Risk factors in IBD
The causes of sexual dysfunction in IBD are increased disease activity, surgery, medications, depression, and hypogonadism. Active disease affects all aspects of quality of life and can severely impair sexual function. Physicians should ask patients about perianal complications, draining cutaneous fistulae, skin lesions, arthritis deformities, abdominal pain, diarrhea, incontinence, fevers, and fatigue, as these complications are relevant not only to sexual dysfunction but to all aspects of IBD care. Pelvic surgery, especially the ileoanal J pouch anastomosis (IPAA) and permanent ostomy, can affect sexual functioning and this should be discussed with patients prior to surgery. Additionally, the risks of sexual dysfunction should be addressed prior to starting medications, such as steroids, narcotics, and antidepressants. Depression is one of the major causes of sexual dysfunction and patients can be screened for this using standard tools, such as the PHQ-9. Asking patients about amenorrhea, menstrual irregularities, hot flashes, and infertility can help elucidate hypogonadism. Narcotic and steroid use and chronic inflammation can contribute to hypogonadism, prompting a referral to gynecology and/or endocrinology.
Pathophysiology
Pelvic floor muscles are voluntary muscles important for bowel and bladder control and sexual and supportive functions. Symptoms such as abdominal or pelvic pain, diarrhea, urgency, and perianal pain or drainage can cause the pelvic floor muscles to contract as a protective mechanism or create dyssynergy in response to pain and/or fear of leakage. Pelvic surgery can also affect the pelvic floor muscles by creating adhesions and scar tissue, leading to pain and pelvic floor muscle dysfunction. Contraction and dyssynergy of the pelvic floor muscles can lead to decreased sexual response. Depression, decreased feelings of attractiveness, and body image issues can also lead to sexual dysfunction by decreasing desire for sexual activity.
Effects of IBD surgery
Sexual activity in the immediate postoperative period, specifically with IPAA or permanent ostomy, can be affected by pain, feelings of unattractiveness from scars and healing wounds, embarrassment over a stoma, or dyspareunia. Pelvic dissection can injure the sympathetic and parasympathetic nerves or cause scar tissue that affects the sexual response. Sympathetic nerve injury can result in decreased vaginal lubrication and the rate of dyspareunia after IPAA can be as high as 38%. In addition, profuse vaginal discharge, decreased vaginal proprioception, and fecal leakage during intercourse have also been reported. The results for IPAA are mixed, with various authors reporting better or worse outcomes on dyspareunia, stool leakage, ability to attain orgasm, sexual satisfaction, and body image. Although we know that laparoscopic rather than open pouch surgery may improve fertility, there are no data on laparoscopic surgery and sexual function. Women with ostomies report decreased attractiveness (52%) because of the appliance, stoma, and odor. More women (60%) than men (52%) felt less desirable and found sexual intercourse difficult psychologically (46%) and physically (32%). Another study found increased dyspareunia in women after proctocolectomy and ileostomy; 12% (8 of 66) reported dyspareunia before surgery and 27% (18 of 66) after surgery.
Effects of medical therapy
Opiates, anxiolytics, and antidepressants are commonly used in the IBD population and have a significant sexual side effect profile. In one study, 10% of the IBD patients commonly omitted regular medication use because of a perceived detrimental impact on libido and sexual activity. Selective serotonin reuptake inhibitors contribute to orgasmic and arousal disorders, with sexual dysfunction reported in 25–80% of users. Steroids affect body image and impair sexual function by causing weight gain, fluid retention, acne, increased facial hair, irritability, depression, and muscle weakness. Narcotics may decrease desire and orgasmic function. Although several studies show that anti-TNF medications can negatively affect sexual function, the cause is most likely the pre-existing disease activity itself. GIs should take a thorough medication history and let the goal of healthy sexual function help guide medical therapy for IBD. Patients may be more amenable to using biologic therapy if their sexual functioning improves as their disease activity remits.
Inflammatory bowel diseases and sexual function
Epidemiology in IBD
It is not surprising that IBD should affect sexual function, given the multiple medications, surgeries, and debilitating symptoms, such as perianal fistulas, diarrhea, incontinence, and abdominal pain, that patients experience. Several studies have shown that 40–60% of women and 44% of men with IBD report sexual dysfunction. The Crohns and Colitis Foundation of America (CCFA) Partners, an ongoing large Internet cohort study of 12,000 patients with IBD, is helping to determine the prevalence of the problem. In a survey of 2151 patients with active IBD, 80% indicated that symptoms affected their sexual satisfaction, and decreased sexual satisfaction correlated with increased disease activity. Patients desire information from their healthcare providers on this issue; 61% of women and 46% of men wanted information about the impact of IBD on intimacy and sexuality at the time of IBD diagnosis. Yet, only 40% of patients had discussed these concerns with their doctor. There is an additional reluctance in both male and female patients to discuss this topic when there is a physician-patient gender mismatch. The role of interdisciplinary care and communication between the GI, OBGYN, and, potentially, the colorectal surgeon could help fill the gaps and meet the patient’s needs on this sensitive issue ( Figure ).





