Background
Cervical dilation in the second trimester is associated with a greater than 90% rate of spontaneous preterm birth and a poor perinatal prognosis.
Objective
To compare the perinatal outcomes of twin pregnancies with dilated cervix in women who underwent either cerclage or expectant management.
Study Design
Retrospective cohort study of asymptomatic twin pregnancies identified with cervical dilation of ≥1 cm at 16–24 weeks (1997–2014) at 7 institutions. Exclusion criteria were genetic or major fetal anomaly, multifetal reduction at >14 weeks, prior cerclage placement, monochorionic–monoamniotic placentation, active vaginal bleeding, labor, chorioamnionitis, elective termination of pregnancy, or medically indicated preterm birth. The primary outcome was incidence of spontaneous preterm birth at <34 weeks. Secondary outcomes were incidence of spontaneous preterm birth at <32 weeks, <28 weeks, and <24 weeks; perinatal mortality; and composite adverse neonatal outcome (respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and sepsis).
Results
A total of 76 women with twin pregnancy with dilated cervix of 1.0–4.5 cm were managed with either cerclage (n = 38) or expectant management (n = 38). Demographic characteristics were not significantly different. Analysis was adjusted for amniocentesis and vaginal progesterone use. In the cerclage group, 29 women (76%) received prophylactic indomethacin and 36 (94%) received prophylactic antibiotics, whereas the expectant management group did not. Interval from time at diagnosis of open cervix to delivery in the cerclage group was 10.46 ± 5.6 weeks vs 3.7 ± 3.2 weeks in the expectant management group, with a mean difference of 6.76 weeks (95% confidence interval [CI], 4.71–8.81). There were significant decreases in spontaneous preterm birth at <34 weeks (52.6% vs 94.7%; adjusted odds ratio [aOR], 0.06; 95% CI, 0.03–0.34), at <32 weeks (44.7% vs 89.4%; aOR, 0.08; 95% CI, 0.03–0.34); at <28 weeks (31.6% vs 89.4%; aOR, 0.05; 95% CI, 0.01–0.2); and at <24 weeks (13.1% vs 47.3%; aOR, 0.17; 95% CI, 0.05–0.54). There were also significant reductions in perinatal mortality (27.6% vs 59.2%; aOR, 0.24; 95% CI, 0.11–0.5), neonatal intensive care unit admission (75.9% vs 97.6%; aOR, 0.07; 95% CI, 0.01–0.66), and composite adverse neonatal outcome (33.9% vs 90.5%; aOR, 0.05; 95% CI, 0.01–0.21).
Conclusion
Cerclage, indomethacin, and antibiotics in twin pregnancies with dilated cervix ≥1 cm before 24 weeks were associated with significant longer latency period from diagnosis to delivery (6.7 weeks), decreased incidence of spontaneous preterm birth at any given gestational age, and improved perinatal outcome when compared with expectant management.
In the United States, the twin birth rate increased by 76% from 1980 through 2009 (from 18.9 to 33.2 per 1,000 total births), mostly due to the increased use of assisted reproductive technology and older maternal age. Preterm birth (PTB) in twin pregnancies is 5 times greater than in singletons. In 2013, 56.5% of twin pregnancies delivered before 37 weeks and 11.3% before 32 weeks, whereas in singleton pregnancies 11.3% delivered before 37 weeks and 1.5% before 32 weeks. Twins are also at increased risk for being low-birthweight infants (LBW), and for early neonatal and infant death and complications related to prematurity and LBW.
In previous publications, a singleton pregnancy with second-trimester (16–28 weeks) cervical dilation of >1 cm was associated with a poor prognosis, with a greater than 90% rate of spontaneous PTB (SPTB), regardless of prior cervical length, obstetric history, or other risk factors for PTB. Cerclage performed secondary to dilated cervix has also been called rescue, emergency, or urgent cerclage. It is defined as a cerclage placed in the presence of cervical changes of the internal os (eg, ≥1 cm dilated, or prolapsed membranes) detected on physical examination (with a speculum or digital examination); effacement is not required for this diagnosis. After clinical examination to rule out uterine activity, intraamniotic infection, or both, placement of cerclage (if technically feasible) in patients with singleton gestations who have cervical change of the internal os may be beneficial.
In twins, data on the efficacy of cerclage based on dilated cervix are limited. In contrast to singleton pregnancies, the use of cerclage for dilated cervix in twin pregnancies has not been studied in a dedicated randomized controlled trial (RCT). The only published RCT evaluating cerclage for cervical dilation compared 13 women who received cerclage and indomethacin and 10 women who received bed rest only; all women received antibiotics (the cohort included 7 twin pregnancies, 3 in the cerclage and 4 in the bed rest group). This RCT showed a significant decrease in PTB at <34 weeks of gestation and a longer latency interval from diagnosis to delivery (by 30 days); however, twin outcomes were not reported separately. There are a few case series of twin pregnancies with second-trimester cervical dilation in which cerclage was associated with favorable outcomes. Three studies compared cerclage in twin vs singleton pregnancies with cervical dilation, showing a high likelihood of delivery at >32 weeks with improved neonatal survival. However, there are no studies in twin pregancies comparing the efficacy of cerclage based on physical examination with the appropriate control, namely, twin pregnancies with dilated cervix and expectant management. The risk of adverse perinatal outcome of twin pregnancies with dilated cervix ≥1 cm diagnosed before 24 weeks is unknown.
The risk of intraoperative rupture of membranes during the placement of cerclage in the presence of dilated cervix has been reported to be between 4% and 19%. Common techniques to avoid this complication include the following: amnioreduction, Trendelenburg position, gentle traction of the cervix with ring forceps, bladder filling with an infusion of 500 mL of saline solution, and/or reduction of membranes using a sponge stick or Foley balloon.
The aim of our study was to evaluate whether the use of cerclage placement in twin pregnancies with asymptomatic cervical dilation of ≥1 cm before 24 weeks decreased the incidence of SPTB at <34 weeks’ gestation and adverse neonatal outcomes when compared with expectant management.
Materials and Methods
This was a retrospective cohort study of twin pregnancies with asymptomatic cervical dilation of the internal os ≥1 cm or prolapsed membranes up to the external os, without signs of labor or chorioamnionitis at 16–24 weeks between 1997 and 2014 at Thomas Jefferson University Hospital (PA), North Shore University Hospital (NY), Long Island Jewish Medical Center (NY), University of Naples Federico II (Italy), Columbia University Medical Center (NY), Beth Israel Deaconess Medical Center (MA), and Robert Wood Johnson Medical School Rutgers University (NJ). Exclusion criteria were as follows: genetic or major fetal anomalies, history of multifetal pregnancy reduction to twins >14 weeks, elective termination of pregnancy, monochorionic–monoamniotic placentation, medically indicated PTB (twin–twin transfusion syndrome, severe preeclampsia, placental abruption, or placenta previa), cerclage placed for another indication (history or ultrasound indicated cerclage) or if, at diagnosis, prolapsed amniotic membranes beyond the external os, active vaginal bleeding, labor, preterm premature rupture of membranes (PPROM), or chorioamnionitis (clinical or subclinical).
Some patients were identified in the ultrasound unit when cervical length was suspected to be short based on either transabdominal or transvaginal ultrasound, and this prompted a physical examination because of concern for cervical insufficiency (the inclusion criteria were dilated cervix and no short cervix). Other patients were identified in the provider’s office or the emergency room if the patients reported contractions or vaginal discharge. Patients were then evaluated in the labor and delivery suite for active labor or chorioamnionitis (either clinically or by amniocentesis of the presenting twin). Patients were deemed asymptomatic if, after an observation period, the symptoms subsided and the patients were clinically stable to be discharged from hospital care. Cerclage or expectant management was offered to those women who were considered asymptomatic by the physician. The management group was determined by the preference of the treating physician only.
The following variables were collected by retrospective chart review: age, parity, race/ethnicity, chorionicity, use of artificial reproductive technology, gestational age (GA) at the time of cervical dilation, cervical dilation (in centimeters), GA at the time of cerclage, type of cerclage (Shirodkar or McDonald), type of suture, amniocentesis, amnioreduction, manipulation of membranes during the cerclage, maternal comorbidities, PPROM, admission to the antenatal unit, hospital length of stay (LOS), administration of antenatal corticosteroids and tocolysis, GA at delivery, interval from diagnosis of cervical dilation to delivery, delivery indications, and mode of delivery. Neonatal outcomes were also collected, including the following: birthweight (BW), Apgar score at 5 minutes, admission to the neonatal intensive care unit (NICU), NICU LOS, and neonatal morbidities (respiratory distress syndrome [RDS], intraventricular hemorrhage [IVH] grade 3 or 4, necrotizing enterocolitis [NEC] grade 3 or 4 requiring surgery, sepsis, retinopathy of prematurity [ROP] requiring laser treatment, and neonatal survival at discharge).
GA was determined by last menstrual period and early ultrasound. Chorionicity was determined by early ultrasound. Cervical dilation was determined by pelvic and/or speculum examination between 16 and 24 weeks (by digital examination with dilated internal os ≥1 cm and palpable amniotic membranes, and/or by speculum examination with visible dilated cervix and visible membranes into the endocervical canal or at the external os but not beyond the external os). PPROM was defined by gross rupture of amniotic fluid, visualizing amniotic fluid on sterile speculum examination, and a positive nitrazine test result with a ferning pattern on microscopy. Active labor was defined as the presence of regular uterine contractions of 3 or more in 10 minutes with cervical change. Subclinical chorioamnionitis was defined by the following: (1) the combination of the presence of any bacteria in amniotic fluid Gram stain, amniotic fluid leukocyte count (≥6 leukocytes per high-power field or >30 cells/mm 3 ) and/or amniotic fluid glucose concentration of ≤15 mg/dL ; or (2) positive amniotic fluid culture results. Clinical chorioamnionitis was defined as follows: maternal fever ≥38°C (≥100.4° F) plus 1 of the following: maternal tachycardia (>100 beats/min), fetal tachycardia, (>160 beats/min), marked leukocytosis (>15,000 cells/mm 3 ), uterine tenderness, or foul odor of the amniotic fluid. Subjects were not randomly assigned to a particular management strategy; patients underwent cerclage or expectant management or any other particular therapy according to physician preference. Decisions to perform amniocentesis, amnioreduction, cerclage, and the surgical technique used were at the discretion of the attending physician after informed consent was obtained from the patient. Cerclage was performed if the patient had a dilated cervix of ≥1 cm, if the patient was clinically asymptomatic, and if preliminary results of amniotic fluid showed no evidence of inflammation (absence of bacteria or leukocytes in the Gram stain, negative leukocyte esterase, and normal levels of glucose in the amniotic fluid), without waiting for culture results.
The primary outcome was SPTB at <34 weeks. The main secondary outcomes were as follows: SPTB at <32 weeks, <28 weeks, or <24 weeks; perinatal mortality and composite neonatal adverse outcome, which required at least 1 of the following: RDS (ventilator support, intubation, continuous positive airway pressure [CPAP], or use of surfactant), IVH grade 3 and 4 as determined by cranial ultrasound or computed tomography (CT) according to the Papile classification, NEC grade 3 and 4 requiring surgery, proven sepsis (clinically ill infant with suspected infection plus positive blood, cerebrospinal fluid [CSF], or catheterized/suprapubic urine culture or cardiovascular collapse or unequivocal x-ray finding), or ROP requiring laser treatment. The primary and secondary outcomes were evaluated in the subgroup of women with cervical dilation of <2 cm and ≥2 cm, to evaluate the efficacy of cerclage in less severe or more severe cases.
The institutional review boards at the participating institutions approved this study. Statistical analysis was conducted using Statistical Package for Social Sciences (SPSS) version 19.0 (IBM Inc, Armonk, NY). Data are shown as mean ± standard deviation (SD) or number (percentage). Differences between women who received cerclage and controls were analyzed using the χ 2 test or Fisher exact test for categorical variables. Results of primary and secondary outcomes were presented as odds ratio (OR) or as mean difference with 95% confidence interval (CI). An adjusted OR (aOR) was calculated after adjusting for confounders that were statistically different. Within-group comparison was performed using the Wilcoxon and Mann–Whitney tests. Kaplan–Meier curves were generated for gestational age at delivery by cervical dilation and compared using the log-rank test. A P value of <.05 was considered statistically significant. This study was performed following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement guidelines.
Results
We identified 76 women with a twin pregnancy and asymptomatic cervical dilation from 1.0 cm to 4.5 cm by physical examination. Of the women, 38 underwent cerclage and 38 were followed up without a cerclage, with expectant management (controls). Demographic characteristics were not significantly different except for rate of amniocentesis. Use of vaginal progesterone was not significantly different between the 2 groups. However, because of the high frequency in the cerclage group (15.8% vs 5.2%, P = .15), we included this variable in the logistic regression ( Table 1 ). Analysis was adjusted for amniocentesis and vaginal progesterone administration.
| Variable | Cerclage n = 38 | Control n = 38 | P value |
|---|---|---|---|
| Maternal age, y | 31.5 ± 5.8 | 30.0 ± 6.6 | .51 |
| Race/ethnicity | |||
| White | 24 (63.1) | 22 (57.9) | .64 |
| African American | 9 (23.6) | 9 (23.6) | 1.00 |
| Hispanic | 4 (10.5) | 4 (10.5) | 1.00 |
| Asian/Indian | 1 (2.6) | 3 (7.9) | .32 |
| Nuliparity | 22 (57.9) | 22 (57.9) | 1.00 |
| Diamniotic–dichorionic | 30 (78.9) | 31 (81.5) | 1.00 |
| Assisted reproductive technology | 17 (44.7) | 19 (50) | .85 |
| Prior PTB | 3 (7.9) | 4 (10.5) | .73 |
| Prior cervical surgery, LEEP/CKC | 1 (2.6) | 2 (5.2) | 1.0 |
| Smoking | 4 (10.5) | 8 (21) | .22 |
| BMI | 31.37 ± 5.36 | 30.7 ± 5.8 | .68 |
| BMI ≥30 | 23 (60) | 19 (50) | .36 |
| GA at diagnosis, wk | 20.7 ± 1.6 | 20.6 ± 1.9 | .67 |
| Cervical dilation at diagnosis, cm | 2.0 ± 1.1 | 2.1 ± 0.9 | 0.52 |
| Cervical dilation ≥2 cm at diagnosis | 24 (63.1) | 24 (63.1) | 1.00 |
| Membrane prolapse | |||
| None | 2 | 3 | 1.0 |
| Into cervical canal | 36 | 35 | 1.0 |
| Amniocentesis | 30 (79) | 5 (13.1) | <.0001 |
| Vaginal progesterone | 6 (15.8) | 2 (5.2) | .15 |
| Prophylaxis at time of cervical dilation diagnosis | |||
| Indomethacin | 29 (76%) | 0 (0) | <.0001 |
| Antibiotics | 36 (94%) | 0 (0) | <.0001 |
The primary outcome of SPTB at <34 weeks was significantly decreased in the cerclage group: 20 (52.6%) vs 36 (94.7%); adjusted odds ratio (OR): 0.06; 95% confidence interval (CI), 0.03– 0.34. Secondary outcomes (rates of SPTB at different gestational ages, admission to antepartum unit, perinatal mortality, and neonatal outcomes) were all significantly decreased in the cerclage group when compared with the control ( Table 2 ). Cerclage was associated with a longer latency period from diagnosis to delivery of 10.5 ± 5.6 vs 3.7 ± 3.2 weeks, with a mean difference of 6.76 weeks (95% CI, 4.71–8.81). The cerclage group also had less admissions to the antenatal unit, and less need of steroids for fetal maturation. Delivery occurred at a later GA in the cerclage group compared with the control group (31.2 ± 5.6 vs 24.3 ± 4.2 weeks; mean difference, 6.90 weeks; 95% CI, 4.67–9.13) ( Table 2 ). PPROM presented also at a later GA (28.2 ± 6.1 vs 22.15 ± 2.5 weeks; mean difference, 6.05; 95% CI, 3.95–8.15). However, the incidence of PPROM or latency from PPROM to delivery were not significantly different. The perinatal mortality was significantly lower in the cerclage group when compared with the control group (21/76 [27.6%] vs 45/76 [59.2%], aOR, 0.24; 95% CI, 0.11–0.5; P < .0001). Among the 96 neonates born alive (54 [73.6%] in the cerclage group vs 42 [55.2%] in the control group), NICU admission, NICU LOS, perinatal mortality, and composite adverse neonatal outcome were significantly decreased in the cerclage group compared to the control group ( Table 3 ).
| Variable | Cerclage n = 38 | Control n = 38 | aOR (95% Cl) | P value |
|---|---|---|---|---|
| SPTB at <34 weeks | 20 (52.6) | 36 (94.7) | 0.06 (0.03–0.34) | <.0001 |
| SPTB at <32 weeks | 17 (44.7) | 34 (89.4) | 0.08 (0.03–0.34) | <.0001 |
| SPTB at <28 weeks | 12 (31.6) | 34 (89.4) | 0.05 (0.01–0.21) | <.0001 |
| SPTB at <24 weeks | 5 (13.1) | 18 (47.3) | 0.17 (0.05–0.54) | .02 |
| Antepartum admission | 14 (36.8) | 24 (63.1) | 0.35 (0.15–0.87) | .02 |
| Antepartum LOS (days) | 12.5 ± 16 | 4.3 ± 5.5 | 8.20 (2.79–13.61) b | .62 |
| PPROM <34 weeks | 8 (21) | 12 (31.5) | 0.5 (0.3–1.6) | .58 |
| GA at PPROM | 28.2 ± 6.1 | 22.15 ± 2.5 | 6.05 (3.95–8.15) b | .02 |
| Antenatal steroids | 11 (28.9) | 21 (55.2) | 0.33 (0.12–0.85) | .02 |
| Tocolysis | 5 (13.1) | 8 (21) | 0.55 (0.16–1.9) | .36 |
| GA at delivery (weeks) | 31.23 ± 5.6 | 24.3 ± 4.2 | 6.90 (4.67–9.13) b | <.0001 |
| Diagnosis to delivery interval (weeks) | 10.46 ± 5.6 | 3.7 ± 3.2 | 6.76 (4.71–8.81) b | <.0001 |
| Mode of delivery | ||||
| Vaginal delivery both | 15 (39.4) | 25 (65.7) | 0.61 (0.37–0.95) | .03 |
| CS both | 21 (55.3) | 11 (28.9) | 1.92 (1.07–3.39) | .03 |
| Vaginal delivery twin A and CS twin B | 2 (5.2) | 2 (5.2) | 1.00 (0.16–6.6) | 1.0 |
| Birthweight (g) a | 1776 ± 948 | 825 ± 479 | 951 (613.3–1288.7) b | <.0001 |
| Birthweight <1500g a | 33/76 (43.4) | 70/76 (92.1) | 0.06 (0.02–0.17) | <.0001 |
| Apgar score <7 at 5 min a | 18/76 (23.6) | 46/76 (60.5) | 0.22 (0.12–0.44) | <.0001 |
| Perinatal mortality a | 21/76 (27.6) | 45/76 (59.2) | 0.24 (0.11–0.5) | <.0001 |
| Both twins discharged home alive | 25/38 (65.7) | 14/38 (36.8) | 3.2 (1.27–8.4) | .01 |
| At least 1 twin discharged home alive | 29/38 (76.3) | 17/38 (44.7) | 3.8 (1.4–10.6) | <.01 |
| Variable (born alive only) | Cerclage n = 54 | Control n = 42 | aOR (95% CI) | P value |
|---|---|---|---|---|
| Composite neonatal outcome | 18 (33.9) | 38 (90.5) | 0.05 (0.01–0.21) | <.0001 |
| Admission to NICU | 41 (75.9) | 41 (97.6) | 0.07 (0.01–0.66) | .02 |
| NICU LOS (days) | 32.1 ± 41 | 87.14 ± 51.9 | –55.04 (–76.07 to –34.01) a | <.0001 |
| RDS | 25 (46.3) | 39 (92.8) | 0.06 (0.01–0.25) | <.0001 |
| IVH stage 3, 4 | 2 (3.7) | 17 (40.5) | 0.05 (0.01–0.26) | <.0001 |
| NEC stage 3, 4 | 5 (9.2) | 12 (28.5) | 0.27 (0.08–0.9) | .02 |
| Sepsis | 7 (12.9) | 10 (23.8) | 0.44 (0.1–1.3) | .18 |
| ROP/laser | 1 (1.8) | 9 (21.4) | 0.07 (0.01–0.57) | .01 |
Cerclage and control subjects were distributed evenly in the 17-year period of the study (2–5 cases per year). There were 20 cerclages before 2007 (2–5 cases in those years) vs 18 after 2007. There were no significantly differences in primary or secondary outcomes among cases or controls evaluated during the first half vs the second half of the 17-year period of evaluation.
In all, 29 of 76 women (38%) had CL evaluations before being included in the study (18 [47%] cerclage, 11 [28%] control; P = .15). The range and mean of CL were as follows: cerclage 1–16 mm with mean of 6 ± 4.8 mm; control, 1–22 mm with a mean of 9 ± 6.3 mm; P = .68. The difference in days between the CL evaluations and the physical examination that diagnosed cervical dilation was 0–1 day in 50% of cases; these women had a cervical length of <10 mm. In the other 50% of women, the time between CL measurements to cervical dilation was 7–28 days. The inclusion criterion for this study was the presence of a dilated cervix with visible membranes at physical examination, independent of cervical length measurement by ultrasound, either recent or remote.
Vaginal progesterone was used in 6 women in the cerclage group and in 2 women in the expectant management group. The indication for the use of vaginal progesterone was a cervical length of <15 mm. If patients subsequently developed dilation of the cervix, use of vaginal progesterone was continued after the finding of the dilated cervix. There were no differences when these 2 groups were compared or when cerclage/progesterone vs cerclage/no progesterone were evaluated, likely because of the small sample size.
In all, 35 women underwent amniocentesis in the amniotic sac of twin A to assess for subclinical chorioamnionitis (cerclage, 30/38 [79%]; controls, 5/38 [13.1%]). All amniotic fluid samples had normal glucose levels, had negative Gram stains, were negative for white blood cell count, and had negative cultures at 5 days. Of the 35 women, 14 (40%) also had an amnioreduction (fluid removal of 50–500 cc) before cerclage placement. Women who underwent amnioreduction had no significant differences in SPTB at any GA compared to those who did not have this procedure. All women had a single-stitch McDonald cerclage. A total of 72 women (94%) had visible membranes on speculum examination. In the cerclage group, 17 of 38 (44.7%) required membrane manipulation with either a Foley balloon or a sponge. One of the women in the cerclage group had an intraoperative rupture of membranes, followed by vaginal delivery. Sutures used for cerclage included Mersilene tape in 28 cases (73.6%), Ethibon in 8 cases (21%), and Prolene in 2 cases (5.3%). In the cerclage group, 29 women (76%) received prophylactic indomethacin, and 36 (94%) received prophylactic antibiotics (mostly a combination of ampicillin and metronidazole), whereas none of the women in the expectant management group received indomethacin or antibiotics at the time of diagnosis with dilated cervix. During the antepartum period, women in the cerclage group had significantly fewer admissions to the hospital, and less need for antenatal corticosteroids. Women in the cerclage group had a higher rate of cesarean section ( Table 1 ). However, once we removed women with pre-viable GA (8/38 [21%] in cerclage group and 17/38 [44%] in the control group; P = .049), the rate of cesarean section was similar in both groups (23/32 [71.8%] in the cerclage group and 13/21 [62%] in the control group, P = .55).
We stratified women into those with cervical dilation <2 cm or ≥2 cm (less severe and more severe cervical dilation), and evaluated the perinatal outcomes. There were significant differences in primary and secondary outcomes in both of these groups. In women with a cervical dilation of <2 cm: (cerclage, 14; control, 14), the SPTB at <34 weeks was 5 (35.7%) vs 14 (100%) (aOR, 0.02; 95% CI, 0.01–0.33); composite neonatal outcome was 4/13 (30.7%) vs 6/7 (85.7%) (aOR, 0.07; 95% CI, 0.01–0.83); and longer latency period from diagnosis to delivery (7.9 weeks; 11.9 ± 4.7 vs 4.0 ± 2.9, mean difference 7.90 weeks, 95% CI, 6.14–9.66) in the cerclage group. In women with a cervical dilation of ≥2 cm (cerclage, 24; and control, 24), the range of cervical dilation was 2.0–4.5 cm in each group, with similar means and SD ( P = .25): SPTB at <34 weeks was 15 (62.5%) vs 22 (91.6%) (aOR, 0.15; 95% CI, 0.02–0.80); composite neonatal outcome was 9/19 (47.3%) vs 14/14 (100%) (aOR, 0.03; 95% CI, 0.01–0.62), and longer latency period from diagnosis to delivery: 6.1 weeks (9.6 ± 5.9 vs 3.5 ± 3.5, mean difference 6.10 weeks, 95% CI 3.92–8.28) in the cerclage group.
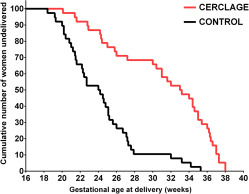
Kaplan–Meier curves were generated for GA at delivery by degree of cervical dilation comparing physical examination–indicated cerclage vs control. The log-rank test showed a significantly different hazard ratio (HR) of 0.33 (95% CI, 0.12–0.34; P < .0001) ( Figure 1 ). For the subgroup of women with cervical dilation of <2 cm, the Kaplan–Meier curve showed an HR of 0.25 (95% CI 0.04–0.27), P < .0001) ( Figure 2 ), and for women with cervical dilation of ≥2 cm an HR of 0.39 (95% CI, 0.15–0.55, P = .0004) ( Figure 3 ).