Background
Patients with 2000 FIGO low-risk gestational trophoblastic neoplasia are commonly treated with single-agent chemotherapy. Methotrexate is widely used in this indication in Europe. Analysis of relapse after treatment and identification of factors associated with relapse would help understand their potential impacts on 2000 FIGO score evolution and chemotherapy management of gestational trophoblastic neoplasia patients.
Objective
This retrospective study analyzes the predictive factors of relapse in low-risk gestational trophoblastic neoplasia patients whose hormone chorionic gonadotropin (hCG) normalized with methotrexate alone.
Study Design
Between 1999 and 2014, 993 patients with gestational trophoblastic neoplasia were identified in the French Trophoblastic Disease Reference Center database, of which 465 were low-risk patients whose hCG normalized with methotrexate alone. Using univariate and multivariate analysis we identified significant predictive factors for relapse after methotrexate. The Kaplan-Meier method was used to plot the outcome of patients.
Results
The 5-year recurrence rate of low-risk gestational trophoblastic neoplasia patients whose hCG normalized with methotrexate alone was 5.7% (confidence interval [IC], 3.86–8.46). Univariate analysis identified an antecedent pregnancy resulting in a delivery (HR = 5.96; 95% CI, 1.40–25.4, P = .016), a number of methotrexate courses superior to 5 courses (5–8 courses vs 1–4: HR = 6.19; 95% CI, 1.43–26.8, P = .015; 9 courses and more vs 1–4: HR = 6.80; 95% CI, 1.32–35.1, P = .022), and hCG normalization delay centered to the mean as predictive factors of recurrence (HR = 1.27; 95% CI, 1.09–1.49, P = .003). Multivariate analysis confirmed the type of antecedent pregnancy and the number of methotrexate courses as independent predictive factors of recurrence. A low-risk gestational trophoblastic neoplasia arising after a normal delivery had an 8.66 times higher relapse risk than that of a postmole gestational trophoblastic neoplasia (95% CI, 1.98–37.9], P = .0042). A patient who received 5–8 courses of methotrexate had a 6.7 times higher relapse risk than a patient who received 1–4 courses (95% CI, 1.54–29.2, P = .011). A patient who received 9 courses or more had an 8.1 times higher relapse risk than a patient who received 1–4 courses of methotrexate (95% CI, 1.54–42.6, P = .014).
Conclusion
Low-risk gestational trophoblastic neoplasia following a delivery and patients who need more than 4 courses of methotrexate to normalization are at a higher risk of relapse than other low-risk patients. Allotting a higher score to the “antecedent pregnancy” FIGO item should be considered for postdelivery gestational trophoblastic neoplasia. Further analysis of the need for consolidation courses is warranted.
Gestational trophoblastic neoplasia (GTN) including invasive moles, which arises in any type of pregnancy and typically from a hydatidiform mole, includes the malignant forms of gestational trophoblastic diseases (GTD), namely malignant invasive mole, choriocarcinoma, and, rarely, placental site trophoblastic tumor (PSTT) or epithelioid trophoblastic tumor (ETT).
After a thorough assessment of the extent of disease, patients are scored/staged according to the FIGO 2000 classification system. Those with a score of 6 or less are classified as having a low risk of resistance to single-agent chemotherapy. Different single-agent protocols are available, and methotrexate (MTX) or dactinomycin are used most often.
A debate about changing the FIGO score calculation to consider the heterogeneous risk of single-agent failure in low-risk GTN patients is currently underway. We previously published predictive factors for resistance to MTX in 154 low-risk GTN patients and identified choriocarcinoma histology and hormone chorionic gonadotropin (hCG) clearance as the only 2 independent predictive factors for resistance, while existing studies had also identified postdelivery GTN and FIGO score level as factors associated with resistance. Beyond analysis of resistance to single-agent chemotherapy, analysis of relapse after treatment and identification of factors associated with relapse would help to improve our understanding of the disease and bring useful data to the current debate. Here, we present a cohort of 465 low-risk GTN patients whose hCG normalized with MTX alone in order to define independent predictive factors for relapse and their potential impact on FIGO 2000 score evolution and chemotherapy management.
Materials and Methods
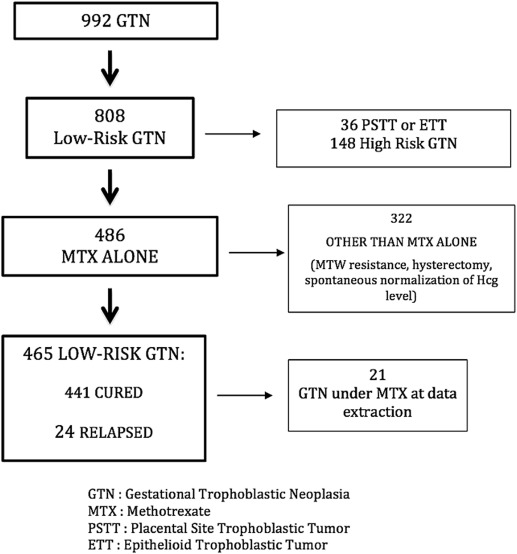
We identified 465 low-risk GTN patients whose hCG normalized with MTX alone, registered to the French Trophoblastic Disease Reference Center (FTDRC) between November 1999 and May 2014. Among 992 total GTN cases, high-risk GTN, PSTT, and ETT patients were excluded (n = 184). Low-risk patients who received treatments other than MTX were excluded, namely those with hysterectomy, MTX-resistant disease requiring second-line chemotherapy, and spontaneous normalization of hCG levels (n = 322). Twenty-one low-risk patients still under MTX treatment at the time of data extraction were not included. One patient had 2 GTN events and we decided to keep the first event in the analysis ( Figure 1 ).
The FTDRC’s functioning has already been described elsewhere. Patients are reported to the FTDRC as molar pregnancy or GTN. They receive the treatment by their physician in their own region according to national guidelines. The FTDRC currently uses MTX in an 8-day MTX regimen with 1 mg/kg intramuscular MTX on days 1, 3, 5, and 7 with 10 mg of folinic acid on days 2, 4, 6, and 8. Day 1 of each course is repeated every 14 days until hCG levels normalize; 2 additional consolidation courses of chemotherapy are given after the first hCG normalization. As patients receive the treatment in different centers, hCG concentrations are determined by different laboratories using various immunoassay kits that could impact interpretation of data.
GTN diagnosis and FIGO score/stage were established according to 2000 FIGO oncology committee recommendations. Twenty-one patients (4.5%) did not complete MTX treatment either owing to poor tolerance or because of nonobservance of the treatment. They were maintained in the study population, as hCG normalized without further treatment. Disease relapse was defined as a rise in hCG levels following the completion of MTX treatment in the absence of a new pregnancy.
The following potential predictive factors were investigated using survival log-rank tests: parameters included in the FIGO score except for location of metastasis item because no metastasis other than pulmonary were present; previous chemotherapy item because all patients were chemonaïve; age; and other potential predictive covariates except for tumor pathology (which was not available for the vast majority of postmolar GTN patients), including FIGO score (0–4 compared to 5–6), premature interruption of MTX (defined as patients who stopped the treatment before normalization or consolidation courses because of poor tolerance), delay in hCG normalization centered to the mean 1.9, number of whole MTX courses, and number of MTX consolidation courses.
For the determination of independent predictive factors for relapse, variables found to be statistically significant in univariate analysis were included in multivariate analysis using the Cox proportional hazards model with backward elimination. A P value of .05 was considered statistically significant. Median follow-up was calculated using a reverse Kaplan-Meier estimate. The Kaplan-Meier method estimated a 5-year survival rate without relapse. The analyses were carried out by SAS V9.3 software (SAS Institute, Cary, NC).
Results
Four hundred and sixty-five patients with low-risk gestational trophoblastic neoplasia normalized their hCG with MTX alone. The mean follow-up period was 56.2 months (range, 1.7–171 months; standard deviation [SD], 40.0). The antecedent pregnancy was a mole in 440 patients (94.6%) and a delivery in 8 patients (1.7%). The mean number of MTX courses was 5.8 (range, 1–18): 166 patients (35.8%) received 1–4 MTX courses, 236 patients (50.7%) received 5–8 courses, and 63 patients (13.5%) received more than 9 courses. No patient died of the disease. The characteristics of the patients are summarized in Table 1 .
| Patient characteristics | All patients (n = 465) n (%) a |
|---|---|
| Age | |
| <40 years | 384 (82.6) |
| ≥40 years | 81 (17.4) |
| Age, mean (SD) | 32.3 (8.1) |
| Interval between end of previous pregnancy and start of chemotherapy | |
| Missing data | 3 (0.7) |
| <4 months | 392 (84.3) |
| 4–6 months (<7 mo) | 63 (13.5) |
| 7–12 months (<13 mo) | 5 (1.1) |
| ≥13 months | 2 (0.4) |
| Pregnancy history | |
| Post mole | 440 (94.6) |
| Post term | 8 (1.7) |
| Post ectopic or termination | 17 (3.7) |
| Serum Hcg before start MTX (IU/L) | |
| ≤1000 | 155 (33.3) |
| 1000–10,000 | 150 (32.3) |
| 10,000–100,000 | 145 (31.2) |
| 100,000–1,000,000 | 15 (3.2) |
| >1,000,000 | 0 (0) |
| FIGO score | |
| 0–4 | 431 (92.7) |
| 5–6 | 34 (7.3) |
| FIGO stage | |
| Stage I | 387 (83.2) |
| Stage II | 17 (3.7) |
| Stage III | 60 (12.9) |
| Stage IV | 1 (0.2) |
| Site of metastases | |
| None or lung | 464 (99.8) |
| Spleen or kidney | 1 (0.2) |
| Alimentary canal | 0 (0) |
| Brain or liver | 0 (0) |
| Premature interruption of MTX | |
| No | 444 (95.5) |
| Yes | 21 (4.52) |
| Number of whole courses of MTX | |
| 1–4 | 166 (35.8) |
| 5–8 | 236 (50.7) |
| ≥9 | 63 (13.5) |
| Number of whole courses of MTX, mean (SD) | 5.8 (2.6) |
| Number of consolidation courses | |
| 0 | 37 (8) |
| 1–1.5 b | 45 (9.7) |
| 2 | 343 (73.8) |
| ≥3 | 40 (8.6) |
| Number of consolidation courses of MTX, mean (SD) | 1.9 (0.7) |
| HCG normalization delay (mo), mean (SD) | 1.9 (1.4) |
| Relapse | |
| No | 441 (94.8) |
| Yes | 24 (5.2) |
a Number and percent of patients, unless stated otherwise
b 1.5 courses: patients who did not complete the second course of MTX because of bad tolerance.
Twenty-four patients relapsed at a mean interval of 10.9 months (range, 1.7–37.7 months). The 5-year Kaplan-Meier recurrence rate was 5.7% (CI, 3.86–8.46).
Among the 8 patients with low-risk GTN after delivery, 25% relapsed. Figure 2 A displays the Kaplan-Meier curve for relapse-free survival according to antecedent pregnancy type. Relapse rate was significantly higher for low-risk GTN occurring after a delivery than after any other type of antecedent pregnancy ( P = .0095).
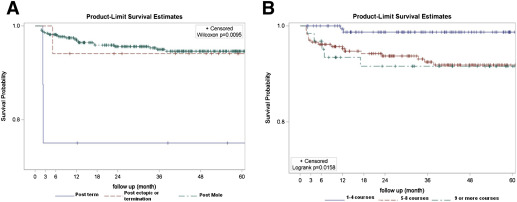
Relapse rate was also significantly higher for patients who had 5–8 courses or more than 9 courses of MTX: 1.2% for patients with 1–4 courses, and 7.2% and 7.9% for 5–8 courses and ≥9 courses, respectively ( P = .016). Figure 2 B displays the Kaplan-Meier curve for relapse-free survival according to number of MTX courses ( P = .0158).
Univariate analysis did not reveal premature interruption of MTX or number of consolidation courses to be risk factors for relapse ( Table 2 ). Further, FIGO score, time interval between last pregnancy and beginning of GTN treatment, hCG level before treatment, and presence of metastasis were not found to be risk factors of relapse for low-risk GTN patients treated with MTX only ( Table 2 ). Three factors were identified as predictive factors of relapse: low-risk GTN after delivery ( P = .016), the overall number of MTX courses ( P = .015 for 5–8 courses vs 1–4; P = .022 for 9 courses or more vs 1–4), and the hCG normalization delay centered to the mean (1.9 months) ( P = .003).
| Risk Factors | Crude hazard ratio | 95% CI HR | P |
|---|---|---|---|
| Age (y) centered at 10 | 0.96 | 0.57–1.59 | .863 |
| Time interval from antecedent pregnancy | |||
| 2–3 months | 1.43 | 0.54–3.82 | .473 |
| ≥4 months | 1.88 | 0.57–6.17 | .296 |
| Versus <2 months | |||
| Last pregnancy outcome | |||
| Delivery | 5.96 | 1.40–25.4 | .016 |
| Abortion or unknown | 1.18 | 0.16–8.78 | .871 |
| Versus mole | |||
| hCG level before treatment (IU/L) | |||
| 1000–10,000 | 1.42 | 0.49–4.10 | .513 |
| 10,000–100,000 | 1.44 | 0.50–4.16 | .496 |
| 100,000–1,000,000 | 3.43 | 0.69–17.0 | .131 |
| Versus <1000 | |||
| FIGO score | |||
| 5–6 | 1.79 | 0.53–5.99 | .348 |
| Versus 0–4 | |||
| Number of metastases | |||
| 0 | 3.87 | 0.52–28.7 | .185 |
| Versus ≥1 | |||
| Premature MTX interruption | 1.11 | 0.15–8.25 | .916 |
| Versus complete regimen | |||
| HCG normalization delay (mo) centered at mean (1.9 mo) | 1.27 | 1.09–1.49 | .003 |
| Number of consolidation courses | |||
| 0 courses | 2.01 | 0.18–22.2 | .569 |
| 1–1.5 courses a | 2.48 | 0.26–23.9 | .431 |
| 2 courses | 2.08 | 0.28–15.6 | .476 |
| Versus ≥3 courses | |||
| Number of whole courses of MTX | |||
| 5–8 courses | 6.19 | 1.43–26.8 | .015 |
| ≥9 courses | 6.80 | 1.32–35.1 | .022 |
| Versus 1–4 courses | |||
| Number of whole courses of MTX (continued value) | 1.13 | 1.00–1.28 | .055 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


