Background
The annual procedure volume is an accepted marker for quality of care and has been documented in various medical fields. Surgeon volume has been shown to correlate with morbidity and mortality rates in surgical and high-risk medical procedures. Although cesarean delivery is 1 of the most common surgical procedures in the United States, the link between a surgeon’s annual cesarean delivery volume and maternal outcome has never been tested.
Objective
The purpose of this study was to evaluate the impact of a surgeon’s annual volume on short-term maternal outcome in cesarean deliveries.
Study Design
We performed a retrospective cohort study in a single tertiary center between 2006 and 2013. Cesarean deliveries were categorized into 2 groups based on the annual volume of cesarean delivery of the attending obstetrician. The “low” group included obstetricians with a low annual volume, whose annual volume of cesarean delivery was lower than median. The “high” group comprised obstetricians with a high annual volume whose annual volume was at median and above. Further analyses were done for quartiles and for 4 clinical relevant groups according to the annual number of cesarean deliveries that were performed/supervised by the attending obstetrician (≤20, 21–60, 61–120, and >120). The primary outcome was a composite adverse maternal outcome that included ≥1 of the following outcomes: urinary or gastrointestinal tract injuries, hemoglobin drop >3 g/dL, blood transfusion, relaparotomy, puerperal fever, prolonged maternal hospitalization, and readmission. Secondary outcomes were operative times (skin incision to delivery and overall).
Results
A total of 11,954 cesarean deliveries were included; the median annual number of cesarean deliveries that were performed/supervised by 1 obstetrician was 48. Unadjusted analysis suggested that the patients in the high group had fewer urinary and gastrointestinal injuries (18/9278 [0.2%] vs 16/2676 [0.6%] injuries; P < .001), less blood loss as measured by hemoglobin drop >3 g/dL (1053/9278 [11.5%] vs 366/2676 [13.8%]; P < .001), and fewer cases of prolonged maternal hospitalization (80/9278 [0.9%] vs 39/2676 [1.5%]; P = .006). The rate of blood transfusion, relaparotomy, puerperal febrile morbidity, and readmission to hospital did not differ between groups. Multivariable regression analysis showed that cesarean delivery performed/supervised by the high group resulted in a significantly lower composite adverse maternal outcome (15.8% vs 18.9%; odds ratio, 0.86; 95% confidence interval, 0.78–0.95; P = .004). This was related primarily to a decreased frequency of urinary and gastrointestinal injuries, lower likelihood of hemoglobin drop >3 g/dL, and lower incidence of prolonged maternal hospitalization. Operative times were significantly shorter for the high group. Composite adverse maternal outcome ranged from 21.8% in the lowest quartile to 17.9% in quartile 2, to 17.4% in quartile 3, and 15.6% in quartile 4. quartile 4 served as the reference; quartile 3 had an odds ratio of 1.14 (95% confidence interval, 1.01–1.29; P = .029); quartile 2 had an odds ratio of 1.18 (95% confidence interval, 1.02–1.36; P = .021, and quartile 1 had an odds ratio of 1.51 (95% confidence interval, 1.14–1.99; P = .004) for composite adverse maternal outcome. Composite adverse maternal outcome ranged from 21.5% in clinical group 1 to 17.5% in clinical group 2, to 17.9% in clinical group 3, and 15.2% in clinical group 4 ( P = .001). Cesarean delivery performed/supervised by clinical groups 2, 3, and 4 in comparison with clinical group 1 were associated with a statistically significant risk reduction, (23%, 25%, and 34% respectively).
Conclusion
Maternal composite morbidity is decreased as the volume of cesarean deliveries that are performed or supervised by obstetricians increases.
The annual procedure volume is an accepted marker for quality of care and has been documented in various medical fields. Surgeon volume has been shown to be correlated directly with morbidity and mortality rates in surgical and high-risk medical procedures. It has been suggested that volume-outcome relationship is not always linear and that, in some instances, there appears to be a threshold.
Cesarean delivery (CD) is 1 of the most common surgical procedures in the United States and worldwide. Compared with vaginal delivery it is associated with increased maternal morbidity that includes hemorrhage, infection, damage to pelvic organs, and increased readmissions. In contrast to other surgical fields, there are no reports regarding the correlation between caregiver annual CD volume and outcome, although other factors of obstetric volume vs outcome have been studied extensively. Examples of variables that that have been assessed include overall hospital delivery volume, timing of delivery and multiple other factors. A nationwide study had found the provider delivery volume to be related to maternal complications, yet the study did not assess the risk of complications related to physician annual CD volume. Physician annual volume has also been linked to the risk of CD. A literature search using Mesh of “Cesarean Section” and outcome, clinical trials published in the English literature on humans between 1995 and 2015 using PubMed revealed 783 publications. These 783 publications titles were read by 2 authors (L.D., H.Y.S.); all relevant abstracts (n = 35) and manuscripts (n = 13) were read. We failed to find an answer to the question whether obstetricians annual CD volume impacts CD outcome.
We hypothesized that obstetricians who perform or supervise more CDs have fewer maternal complications and shorter operative times. The purpose of our study was to explore whether CD outcomes differ when performed/supervised by low vs high annual CD volume obstetricians.
Materials and Methods
We performed a retrospective cohort study of all CD births (defined as ≥24 weeks of gestation) in a single large tertiary center between January 2006 and December 2013. Stillbirths, cesarean hysterectomies, and CD with missing crucial data (defined as CD performed by residents only without attending obstetrician) were excluded. Anonymized patient data were extracted from our computerized database, which included demographic parameters, procedures, and diagnoses all of which are updated during hospital admission.
The study protocol was approved by the Institutional Review Board/Institutional Ethical Committee.
Setting
Shaare Zedek Medical Center is a university-affiliated medical center with a large obstetric service. The Labor and Delivery Department consists of 12 delivery rooms with 2 operating rooms. There are roughly 15,000 deliveries annually, with an annual CD rate of 11% (national CD rate, 19%).
All CDs are performed either by an attending physician or by a resident who is supervised by a scrub attending physician. In elective CD cases, surgery teams are assigned by the chair of the Maternal Fetal Medicine Division, based on medical and surgical history; usually the more complicated cases are assigned a more senior attending physician. Attending physicians performing CDs are general obstetricians, maternal fetal medicine specialists, or other practitioners of obstetrics/gynecology subspecialties (board-certified obstetrics/gynecology) with privileges to perform/supervise CDs, who were either on call or performed CD in their private patients. Attending obstetricians who performed/supervised at least 1 CD during the study period were included in this study. Postoperative and postpartum care routinely is provided by residents who are postgraduate year 1 or 2 and is supervised by a maternal-fetal medicine specialist when necessary. The decision regarding discharge is based on maternal medical status.
Any cutoff of number of CDs performed/supervised annually by a single obstetrician would be arbitrary and, because our aim was to assess whether the obstetrician with a high annual volume had a lower incidence of maternal complications, we decided initially to use the median as a cutoff. The overall median CD performed/supervised annually, based on all the attending physicians, was calculated. The median number of CDs performed/supervised annually was determined for individual obstetricians and was used for group assignment. Physicians who performed fewer than the median were defined as low-volume obstetricians; those who performed from the median and above were defined as high-volume obstetricians. We assigned each CD to 1 of 2 groups: low group (CD was performed/supervised by a low-volume obstetrician) and high group (CD was performed/supervised by a high-volume obstetrician). The low group was chosen as the reference group for analysis. To avoid possible confounding by time, groups were assigned each year separately. All attending physician names were masked and replaced with random numbers to allow analysis to be performed blinded to the identity of the obstetrician.
Because the median was an arbitrary cutoff, we decided to perform additional analysis according to quartiles, to assess whether there is an association between volume and outcome in terms of “more is better,” and to determine the existence of a threshold. To this effect, we compared each quartile to its previous 1. Based on the number of CDs performed/supervised monthly by an obstetrician, we defined 4 clinically relevant groups (CG; CG1, CG2, CG3, and CG4). These groups correspond to the number of CDs performed/supervised annually by an obstetrician; ≤20 (CG1), 21–60 (CG2), 61–120 (CG3), and >120 CDs (CG4). This roughly correlates with 1-2, up to 5, up to 10, and >10 CDs a month.
Further analysis included experience of the surgeon as measured by years from residency graduation and analysis without the outliers that were defined as obstetricians who performed <10 CDs per year or >350 CDs per year
Outcome measures
Our primary outcome measure was a composite adverse maternal outcome that represented the occurrence of ≥1 of the following events: urinary and gastrointestinal tract injuries (ie, incidental cystotomy, ureterotomy, ureter obstruction, or enterotomy), hemoglobin drop >3 g/dL (calculated between pre- and postoperative hemoglobin levels), double to triple the average blood loss during CD, blood transfusion (≥1 units of packed red blood cells), relaparotomy (within initial admission), puerperal febrile morbidity (defined as temperature of ≥100.4°F [≥38°C] on any 2 of the first 10 days after delivery, exclusive of the first 24 hours), prolonged maternal hospitalization (length of stay >10 days), and/or readmission to hospital (within 42 days postoperatively ). Secondary outcomes were lengths of operative times: skin incision to delivery of the neonate and overall time from skin incision to skin closure.
Exposure
The primary exposure variable was obstetrician annual CD volume. Univariate analysis was performed for categoric variables with the use of the χ 2 or Fisher’s exact tests. Continuous variables were compared with the use of the Student t test or Mann-Whitney U test. To evaluate the independent association between obstetrician annual CD volume and each outcome, we conducted multivariate logistic regression modeling, adjusting for patient demographic parameters and comorbidities: maternal age, maternal education (>12 years), parity, assisted reproduction techniques, hypertensive disorder, diabetes mellitus, multifetal gestation, placenta previa, gestational age, trial of labor after cesarean delivery, intrapartum fever (temperature >100.4°F [38°C]), second stage CD, delivery during on-call hours, and elective vs urgent CD. Each model was constructed in 2 blocks: First, all potential confounders were assigned to the model with the use of the stepwise backward method. Next, obstetrician annual CD volume was forced into the model with the use of the “enter” method. Multiple linear regression models were used to investigate the relation of obstetrician annual CD volume with CD durations while controlling for the aforementioned potential confounders. Additional analysis was performed to assess whether there was a linear association between obstetrician’s annual volume and composite adverse maternal outcome by dividing the group into 4 quartiles of volume and 4 CGs (CG1-4). Odds ratio (OR) and 95% confidence intervals (CI) are reported. All tests are 2-tailed; a probability value below .05 was considered statistically significant. Analyses were carried out with SPSS software package (version 20.0; IBM Corporation, Armonk, NY).
Results
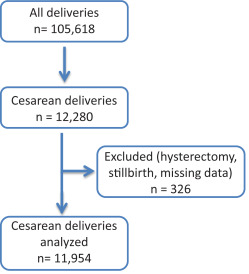
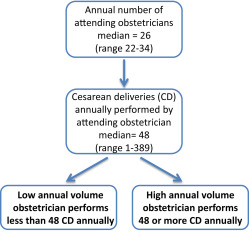
During the study period, there were a total of 105,618 deliveries of which 12,280 (11.6%) were by cesarean delivery. We excluded 50 stillbirths (0.4%), 60 cases of cesarean hysterectomy (0.5%), and 216 cases that were missing crucial data (1.7%), for a total of 11,954 CDs (97.3%) for analysis ( Figure 1 ). The annual median number of attending obstetricians was 26 (range, 22–34). Throughout the study period, the median number of CDs that were performed/supervised annually by a single attending obstetrician was 48 (range, 1–389); thus, CDs that were performed/supervised by an obstetrician who performed/supervised <48 CDs annually were assigned to the low group; and CDs that were performed/supervised by 1 of the physicians who performed/supervised ≥48 CDs annually were assigned to the high group. In total, 2676 CDs (22.4%) were assigned to the low group and 9278 CDs(77.6%) throughout the study period were assigned to the high group ( Figure 2 ). The overall percentage of CDs that were performed by the residents and supervised by the scrub attending physician was 37.3% (4567/12,239 CDs); it varied between years from 28.3–56.6%.
Maternal characteristics are presented in Table 1 . Women with 1 previous CD or ≥3 previous CDs were more likely to be operated on by a high annual volume obstetrician. Cesarean deliveries of nulliparous women, CDs during on-call hours, and urgent CDs were more likely to be performed/supervised by a low annual volume obstetrician. Maternal age, education, the incidence of ≥3 previous miscarriages, multifetal gestation, placenta previa, diabetes mellitus, and hypertensive disorders did not differ between groups.
| Characteristic | Cesarean delivery group | P value | |
|---|---|---|---|
| Low volume (n = 2676) a | High volume (n = 9278) b | ||
| Maternal characteristic | |||
| Maternal age, y ± SD | 31.0 ± 6.4 | 31.2 ± 6.3 | .08 |
| AMA (>35 y), n (%) | 702 (26.2) | 2463 (26.5) | .75 |
| Education (≥12 y), n (%) | 2484 (95.7) | 8636 (95.7) | .94 |
| Previous miscarriages (≥3), n (%) | 163 (6.1) | 575 (6.2) | .84 |
| Previous cesarean delivery, n (%) | 988 (36.9) | 4292 (46.3) | <.001 |
| Previous cesarean delivery (≥3), n (%) | 151 (5.6) | 869 (9.4) | <.001 |
| Parity, y ± SD | 3.2 ± 2.6 | 3.4 ± 2.6 | <.001 |
| Nulliparous, n (%) | 916 (34.2) | 2592 (27.9) | <.001 |
| Gestation characteristic, n (%) | |||
| Artificial reproductive techniques | 409 (15.3) | 1073 (11.6) | <.001 |
| Multifetal gestation | 265 (9.9) | 889 (9.6) | .62 |
| Placenta previa | 44 (1.6) | 183 (2.0) | .27 |
| Diabetes mellitus (pregestational and gestational) | 260 (9.7) | 948 (10.2) | .45 |
| Gestational diabetes mellitus | 218 (8.1) | 796 (8.6) | .48 |
| Hypertensive disorder (chronic, gestational, preeclampsia) | 169 (6.3) | 541 (5.8) | .35 |
| Preeclampsia | 128 (4.8) | 364 (3.9) | .05 |
| Labor characteristic | |||
| Gestational age, wk ± SD | 38.0 ± 2.6 | 37.9 ± 2.6 | .001 |
| Preterm <37 weeks, n (%) | 486 (18.2) | 1610 (17.4) | .33 |
| Trial of labor after cesarean delivery, n (%) | 244 (9.1) | 874 (9.4) | .64 |
| Intrapartum fever >100.4°F (38°C), n (%) | 79 (3.0) | 185 (2.0) | .003 |
| Cesarean delivery during second stage, n (%) | 142 (5.3) | 462 (5.0) | .50 |
| Cesarean delivery characteristic, n (%) | |||
| Elective | 1418 (53.0) | 5777 (62.3) | <.001 |
| Urgent | 1258 (47) | 3501 (37.7) | |
| General anesthesia | 166 (6.2) | 574 (6.2) | .98 |
| During on-call hours | 1546 (57.8) | 4611 (49.7) | <.001 |
| Urgent cesarean delivery indication, n (%) | .016 | ||
| Dystocia | 272 (21.6) | 746 (21.3) | |
| Nonreassuring fetal heart rate | 629 (50.0) | 1614 (46.1) | |
| Other | 357 (28.4) | 1141 (32.6) | |
a Cesarean delivery performed/supervised by an obstetrician with a low annual volume
b Cesarean delivery performed/supervised by an obstetrician with a high annual volume.
Composite adverse maternal outcome was identified in 1966 of 11,954 women (16.4%) of the total study population: 500 of 2676 adverse outcomes occurred in women who were assigned to the low group (18.9%), compared with 1466 of 9278 of the women who were included in the high group (15.8%; P < .001). Detailed maternal adverse outcomes are shown in Table 2 . Unadjusted bivariate analysis suggested that high group patients, whose CDs were performed/supervised by high annual volume obstetricians, had fewer urinary and gastrointestinal tract injuries (18/9278 [0.2%] vs 16/2676 [0.6%] women; P < .001), had less blood loss as measured by hemoglobin drop >3 g/dL (1053/9278 [11.5%] vs 366/2676 [13.8%] women; P < .001), and had fewer cases of prolonged maternal hospitalization (80/9278 [0.9%] vs 39/2676 [1.5%] women; P = .006). The rate of blood transfusion, relaparotomy, puerperal febrile morbidity, and readmission to hospital did not differ between groups.
| Outcome | Cesarean delivery group, n (%) | P value | |
|---|---|---|---|
| Low volume (n = 2676) a | High volume (n = 9278) b | ||
| Adverse maternal outcome | |||
| Urinary and/or gastrointestinal tract injuries | 16 (0.6) | 18 (0.2) | .001 |
| Hemoglobin drop >3 g/dL | 366 (13.8) | 1053 (11.5) | .001 |
| Blood transfusion | 112 (4.2) | 351 (3.8) | .34 |
| Relaparotomy | 12 (0.4) | 29 (0.3) | .29 |
| Puerperal febrile morbidity | 48 (1.8) | 172 (1.9) | .84 |
| Prolonged maternal hospitalization | 39 (1.5) | 80 (0.9) | .006 |
| Readmission to hospital | 34 (1.3) | 89 (1.0) | .16 |
| Composite adverse maternal outcome | 500 (18.9) | 1466 (15.8) | <.001 |
a Cesarean delivery performed/supervised by an obstetrician with a low annual volume
b Cesarean delivery performed/supervised by an obstetrician with a high annual volume.
Cesarean deliveries performed/supervised by the high group were significantly shorter, both overall and from the time of skin incision to neonatal delivery time ( P < .001), as shown in Table 3 ; however, the absolute median decrease in surgical times was 1 minute (6 vs 7 minutes [ P < .001] and 30 vs 31 minutes [ P < .001], respectively). Multiple linear models revealed that CDs performed/supervised by high-volume obstetricians were associated independently with shorter durations of skin incision to neonate delivery (–0.93 minutes; 95% CI, –0.66 to –1.18; P < .001) and skin incision to skin closure (–1.25 minutes; 95% CI, –0.28 to –2.22; P = .012).
| Operative time | Cesarean delivery group, median (interquartile range) | P value | |
|---|---|---|---|
| Low volume (n = 2676) a | High volume (n = 9278) b | ||
| Skin incision to fetus delivery | |||
| All cesarean deliveries | 7 (5–10) | 6 (4–10) | <.001 |
| Primary cesarean deliveries | 6 (4–9) | 5 (3–8) | <.001 |
| Recurrent cesarean deliveries | 9 (6–13) | 8 (5–12) | <.001 |
| Skin incision to skin closure | |||
| All cesarean deliveries | 31 (25–40) | 30 (23–41) | <.001 |
| Primary cesarean deliveries | 30 (25–37) | 28 (21–37) | <.001 |
| Recurrent cesarean deliveries | 36 (29–48) | 35 (25–46) | <.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


