Scoliosis
Raymond R. Brodeur
J. Michael Menke
Richard A. Elbert
Scoliosis is defined as an appreciable lateral deviation of the spine. It can affect patients of all age groups with complications varying from cosmetic deformity to severe cardiac and pulmonary compression and death. When viewed from the frontal plane, and assuming relative anatomical and loading symmetry, the ideal shape is a straight spinal column; however, anatomists more than 200 years ago described everyone as having a slight scoliosis (1). Most children are not posturally symmetrical; most have a slight right scoliosis and slight right rib hump. In a recent study, only 2 of 265 children were symmetrical, with most of the children having a short left leg, a left lumbar hump, and a right thoracic rib hump (2). Because true symmetry is rare, the clinician needs to consider the point at which spinal asymmetry is a concern to the patient and the parents.
Currently, the Scoliosis Research Society defines scoliosis as a lateral deviation of the spine of >10 degrees. This may be adequate for the orthopedic surgeon, who has no treatment modality to recommend until a curve exceeds 20 degrees. However, the chiropractor is likely to assume that any lateral deviation is of concern and should be treated as soon as possible. Recent reports have used 5 degrees as the minimum degree of curvature as an inclusion criterion for the presence of scoliosis (3,4).
In this chapter, we discuss the current state of knowledge regarding scoliosis diagnosis and patient treatment, concentrating on progressive adolescent scoliosis, the type that is of most concern to clinicians and patients alike.
SCOLIOSIS IDENTIFICATION AND MEASUREMENT
The apex of a scoliosis is at the vertebra that has the largest lateral deviation from the mid-line of the spine when viewed on an anteroposterior (AP) radiograph. A scoliotic curve is named according to the location of the apex of the curve. For example, a scoliosis is a thoracic curve if the apex is in the thoracic spine.
The curve is either a “right” or “left” scoliosis, as defined by the convexity. A right scoliosis is convex to the right and a right thoracic scoliosis indicates that the apex of the curve is in the thoracic spine and that the curve is convex to the right. If the apex is in a transitional area, the curve is classified as transitional. For example, if the apex is between T11 and L1, then the curve is called a thoraco-lumbar scoliosis.
Cobb Angle
Cobb (5) first defined his method for measuring scoliosis in 1948. His method is well known to many clinicians and remains the primary measurement tool for analyzing scoliosis, despite many attempts to develop improvements.
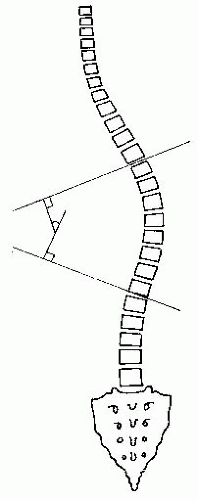
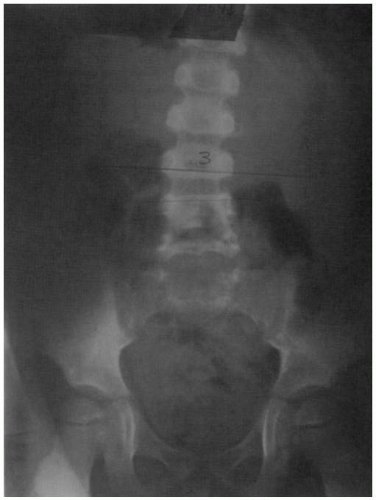
The end-vertebrae of the curve are those that have the greatest angulation toward the apex of the curvature. Lines are drawn parallel to the superior endplate of the cephalic end-vertebra and the inferior endplate of the caudal end-vertebra. The angle between these two lines is the Cobb angle (Fig. 14-1).
The Cobb angle has been shown to have a high measurement error, with repeated measure standard deviations of between 2 to 3 degrees for the same examiner measuring the same film (6), and it has been reported to be as large as 4 degrees for multiple examiners (7). In addition to technical variabilities in the measurement, the Cobb angle does not provide any description of the three-dimensional aspects of scoliosis and has been shown to under-estimate the actual severity of the curve (7). However, in spite of these short comings, it is likely to remain the primary method for measuring scoliosis curves for the foreseeable future.
Other Measurements of Scoliotic Curves
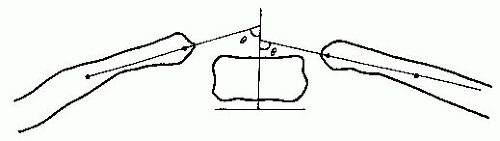
The Cobb angle is independent of the number of vertebrae involved in a scoliosis and provides only a limited description of the true shape of a scoliotic spine. Voutsinas and MacEwen (8) have suggested additional measurements for describing spinal curves. It is possible for two curves to have the same Cobb angle, as shown in Figure 14-2, but the distance of the apex of the curve from the long-axis of the spine may vary significantly, as depicted. The ratio of the width of the curve to the length of the curve is a descriptor that requires further investigation (6).
Many methods have been proposed for describing scoliotic curves. Moire topography (9) and other photographic methods have been proposed to describe the trunk topography (10). However, it is difficult to determine underlying skeletal changes from surface features, and thus these approaches are still experimental as well as controversial. More recently, computed tomography scans have been used to describe scoliotic curves more thoroughly (11). Three-dimensional methods using stereo or bi-planar radiography have also been proposed for describing scoliotic shapes (7). With the increasing use of powerful computers, the means for describing the full three-dimensional aspect of the scoliotic curve will be easier for the clinician (12). At the present time, the measurement tools described above are either too controversial or too experimental to be used by most clinicians.
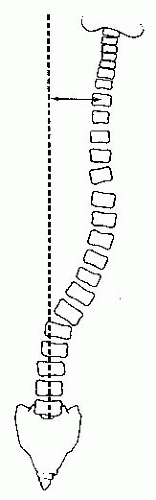
Torso Balance
Ideally, when viewing a full-spine standing AP or posteroanterior (PA) radiograph, a line connecting T1 to S1 should be vertical. The extent to which there is some deviation in this line is graded as the torso balance (13). A vertical line is drawn from S1 to the top of the radiograph. The horizontal distance from T1 to the vertical line is used to describe the torso balance grade (Fig. 14-3). A grade 1 corresponds to <1.5 cm from T1 to the vertical line passing through the mid-line of the sacrum. Grade 2 corresponds to a distance between 1.6 to 3.0 cm, grade 3 from between 3.1 to 5.0 cm, and grade 4 if the distance from T1 to the sacral mid-line is >5 cm.
Vertebral Rotation
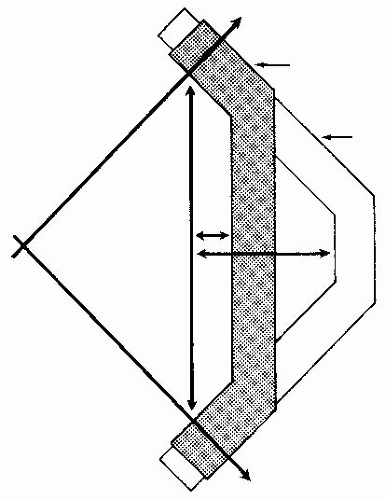
Nash and Moe (14) suggested measuring relative vertebral rotation based on the distance between the pedicles. Normally the pedicles are symmetrical relative to the spinous process and are oval in shape. The pedicles shift toward the concave side of the scoliosis (the spinous points toward the concavity). The amount of rotation is graded from 0 to 4, and the grade for the patient is defined by the most rotated vertebra, which is usually at the apex. The vertebral body is divided into segments, as shown in Figure 14-4. No rotation
corresponds to a grade 0; grade 1 is the rotation of the pedicle into the first segment; at a grade 2, the pedicle is in the second segment; with a grade 3, the pedicle is at the mid-line of the vertebra; and grade 4 occurs when the pedicle crosses the mid-line of the vertebra. The pedicle position can also be used to estimate the number of degrees of vertebral rotation (13,14), as shown in Figure 14-4. Pedicle rotation is described as a percentage of the position on the vertebral body, with each percentage point corresponding to one degree. For example, if the pedicle is at 25% of the body, it corresponds to a rotation of 25 degrees.
corresponds to a grade 0; grade 1 is the rotation of the pedicle into the first segment; at a grade 2, the pedicle is in the second segment; with a grade 3, the pedicle is at the mid-line of the vertebra; and grade 4 occurs when the pedicle crosses the mid-line of the vertebra. The pedicle position can also be used to estimate the number of degrees of vertebral rotation (13,14), as shown in Figure 14-4. Pedicle rotation is described as a percentage of the position on the vertebral body, with each percentage point corresponding to one degree. For example, if the pedicle is at 25% of the body, it corresponds to a rotation of 25 degrees.
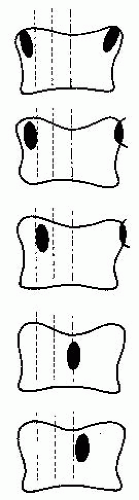 FIGURE 14-4 Vertebral rotation using the method of Nash and Moe. Modified from McAlister WH, Shackelford MGD. Measurement of spinal curvatures. Radiol Clin North Am 1975;13:119. |
The vertebra with the most rotation occurs at the apex of a structural scoliosis. However, the relative rotation is smallest at the apex and largest at the junction of the structural curve with the upper and lower compensatory curves (15). Thus, although the total amount of rotation is largest at the apical vertebra, it is a result of the summing of rotations from the vertebrae above and below the apex. The vertebra at the apex has very little rotation relative to the vertebrae above and below. When assessing the relative rotations at an individual motion segment, as is the case when determining a listing for a specific adjustment, it is important to carefully compare the relative pedicle sizes with the neighboring levels.
Vertebral Wedging
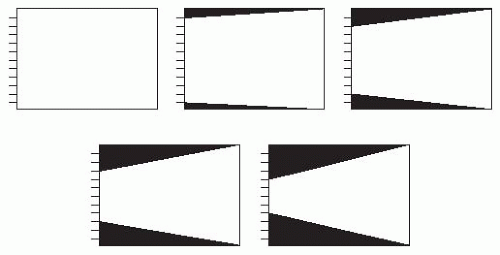
In moderate to severe scoliosis, the vertebrae often become wedge-shaped when viewed on AP or PA radiographs. Wedging may also occur as a result of a congenital anomaly. If the vertebral body height decreases laterally by less than one-sixth, it is considered grade 1 wedging (13). A decrease in vertebral height of between one-sixth to one-third the contralateral height is considered grade 2 wedging; one-third to one-half is grade 3 wedging; and a difference in left-right vertebral height of more than one-half the contralateral height is considered grade 4 wedging (Fig. 14-5).
Wedging of vertebrae may develop as a result of unequal loading on the vertebral endplates (i.e., Heuter-Volkmann Law) (16). Some structural curves may begin without initial osseous deformity, but start with changes in the viscoelastic elements instead (e.g., in discs, muscles, etc.). Any treatment likely would be optimally effective if it could alter the initial soft tissue deformity rather than attempting to change the secondary osseous changes that have occurred.
CLASSFICATIONS FOR SCOLIOSIS
Structural and Non-structural Scoliosis
There are many different causes for scoliosis, but the vast majority are considered to be idiopathic in origin. Table 14.1 is a summary of scoliosis classifications originally described by Winter (17) and modified by Plaugher and Lopes (18). Essentially, scoliosis can be divided into structural curves and nonstructural, or functional, curves. A structural scoliosis will not straighten when the patient flexes during forward bending, whereas functional curves will reduce or disappear upon forward bending and lateral bending to the side of the convexity.
A functional scoliosis is caused by factors external to the spine. A short leg or a pelvic asymmetry are common causes. Lateral flexion subluxations can occur (Fig. 14-6). In some cases, structural scoliosis may begin as a functional curve. If such asymmetries occur at a young age, it has been proposed that the stresses on the vertebral growth plates may be sufficient to cause bone remodeling and thereby create a structural curve (18).
TABLE 14.1 Classifications of Structural and Functional Scoliosis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Curve Patterns
Structural curves are classified into commonly occurring patterns (13):
1. Cervicothoracic
2. Thoracic
3. Thoracolumbar
4. Lumbar
Double structural curves:
1. Double thoracic
2. Combined thoracic and lumbar
3. Combined thoracic and thoracolumbar
Right thoracic structural curves are far more common than left thoracic curves and extend from about T5 to T11 with the apex near T8. In fact, the right thoracic pattern is so common that if the opposite (left thoracic scoliosis) is found, then further examination of the patient is warranted. Patients with syringomyelia or Arnold-Chiari type 1 malformation have a greater likelihood of having a left convex thoracic scoliosis (19,20). In a review of more than 1,600 scoliosis cases, Coonrad
et al. (21) identified only 27 left thoracic curve patterns. Of these 27 cases, 9 had a neurologic etiology.
et al. (21) identified only 27 left thoracic curve patterns. Of these 27 cases, 9 had a neurologic etiology.
With the right thoracic structural curve, there is usually a compensatory lumbar curve that is often confused with a double structural curve. The difference is that the compensatory lumbar curve is functional and can be completely reduced with flexion or lateral flexion, whereas the thoracic curve cannot. Patients with a large thoracic structural curve have more severe cardiorespiratory distress and statistics show that they die earlier (22,23).
The thoracolumbar curve extends from about T8 to L3 with the apex near T11. These curves are less likely to have any associated compensatory curves and the center of gravity of the head is often displaced slightly lateral to the mid-line of the pelvis. Patients with thoracolumbar curves suffer from fewer cardiopulmonary problems; however, curve progression in adulthood is more likely (24).
The structural lumbar curves range from about T12 to L4 with the apex near L3. This curve is most often convex to the left and usually has a pelvic obliquity associated with it, giving the appearance of a short leg on the side of the concavity. A thoracic compensatory curve is commonly found, but the thoracic curve is mild by comparison. These patients often suffer from arthritic changes in the lumbar spine later in life. Lateralisthesis at the apex of the curve is a late sequelae of annular injury. Lumbar curves are less likely to progress than other types (24).
The most common double structural curve is the combined thoracic and lumbar. As the name implies, both curves are structural; that is, neither curve will disappear on forward flexion or lateral bending. Generally they have a right thoracic and a left lumbar curve. Patients with combined thoracic and lumbar curves are more likely to maintain torso balance and to have less cosmetic deformity. However, they usually have a smaller torso height because of the increased curvature as well as more arthritic changes and pain in the lumbar spine in later life (24).
IDIOPATHIC SCOLIOSIS
Infantile
Infantile scoliosis is defined as that occurring during the first three years. It is more common in men than women (3:2), and the curve is most often in the thoracic spine and is usually convex to the left. This condition is rare in North America. The positioning of a baby in its crib may play a role in the development of this type of scoliosis, but this does not explain why it is more common among men (25). The condition has been highly correlated with low birth weight, prematurity, mental retardation, and delayed muscle development. Although most cases resolve on their own (74%-97%), progressive curves become very severe and disabling.
The difference in the left and right rib-vertebra angle (RVA) can be used to indicate the probability of progression for infantile scoliosis (Fig. 14-7). Mehta (26) and others (27) have reported that RVA differences >20 degrees are more likely to progress. Also, if the RVA is <68 degrees at the apex, then progression is also likely.
Juvenile
Juvenile scoliosis is defined as that occurring after 3 years of age and before the onset of puberty. It occurs more often in girls and most cases begin before the age
of 10. There are many who argue that adolescent idiopathic scoliosis (AIS) cases are simply cases of juvenile scoliosis that went undetected. The current trend in scoliosis screenings is to try to detect the onset of scoliosis before puberty begins (15,18,28). Juvenile curves are most likely to progress and must be monitored radiologically at a minimum of 3- to 6-month intervals. Curves that show no sign of progression after follow-up can be monitored less frequently with radiographs. Individual patients with objective signs of subluxation (e.g., tenderness, motion restriction) may require more frequent clinical examinations and treatment (e.g., chiropractic).
of 10. There are many who argue that adolescent idiopathic scoliosis (AIS) cases are simply cases of juvenile scoliosis that went undetected. The current trend in scoliosis screenings is to try to detect the onset of scoliosis before puberty begins (15,18,28). Juvenile curves are most likely to progress and must be monitored radiologically at a minimum of 3- to 6-month intervals. Curves that show no sign of progression after follow-up can be monitored less frequently with radiographs. Individual patients with objective signs of subluxation (e.g., tenderness, motion restriction) may require more frequent clinical examinations and treatment (e.g., chiropractic).
Juvenile patients must be monitored throughout adolescence because curve progression is most likely to occur during this growth period. Severe spinal deformity results if progressive curves are left untreated.
Adolescent
AIS occurs at any time between puberty and adulthood. It is the most common type of idiopathic scoliosis. Because it occurs at a time when physical appearance is most important to an individual, progressive cases can leave physical as well as emotional scars. For curves of <20 degrees, the female to male ratio is 1:1, but for curves >20 degrees the occurrence is much higher for women (up to 5.4:1) (29).
Progression of a scoliotic curve varies greatly between individuals. For the most part, adolescent curves are not progressive. It is estimated that only one to six per 1,000 will ever require treatment for scoliosis (29,30,31,32). However, because we can only know in retrospect which curves progress, deciding which cases need to be monitored is a challenge. All authorities agree that monitoring is most important during the rapid growth phase of puberty. However, there is a great variability in the growth rate as well as the onset of growth. The sections below will describe the natural history of AIS and the many variables that have been shown to affect curve progression.
Natural History of Adolescent Scoliosis Present screening procedures are based on a limited knowledge of the natural history of adolescent scoliosis. The early symptomatic stage shows slight postural asymmetry as well as a rib hump on forward flexion. However, the point at which the lateral deviation requires referral for diagnosis and treatment is not well defined (30,33,34,35,36,37,38).
The cause of progressive spinal scoliosis is far from being understood, but our knowledge of its clinical course is improving. Dickson (15,34) has reported that progressive idiopathic scoliosis has a characteristic loss of the normal thoracic kyphosis at the area of the apex of the scoliosis. This loss of kyphosis is often a local thoracic lordosis. Loss of thoracic kyphosis in the presence of progressive spinal scoliosis is supported by Willner (39) and Somerville (40). Willner reports a consistent loss of the thoracic kyphosis in children with scoliosis compared with a normal population. Somerville hypothesized that progressive scoliosis consists of a local lordosis, rotation, and lateral flexion of the vertebrae involved. In studies involving clinical, cadaveric, biomechanical, and radiological investigations of the pathogenesis of progressive spinal scoliosis, Dickson et al. (15,41,42,43) have concluded that there is always the presence of a local lordosis at the level of the apex of the scoliosis.
Investigations into the normal spinal development of children reveal a constant decrease of the thoracic kyphosis from the age of 8 to 12 years. After the 12th year the angle of the kyphosis begins to increase again (44). Dickson et al. (41) has proposed that this normal loss of kyphosis in combination with the rapid growth spurt of adolescence may be a primary consideration in the cause of progressive scoliosis. When the thoracic kyphosis is at its minimum in girls, they are at their peak growth velocity; whereas boys’ peak growth velocity does not occur for another 2 years. This may be why girls are more prone to suffer from progressive scoliosis than boys. In a study by Archer and Dickson (45), girls with adolescent progressive scoliosis did not differ from girls with pelvic tilt scoliosis or normal girls in growth velocity. However, there was an increase in standing height among the girls with progressive scoliosis. Archer and Dickson (45) propose that the increase in height was caused by the uncoiling of the spine as the thoracic kyphosis decreased and that the scoliosis progression was accelerated by the loss of the thoracic kyphosis. Girls with progressive scoliosis have been reported to reach menarche sooner, are taller than their peers when initially diagnosed with scoliosis, and have an earlier pubertal growth spurt (46).
Another consideration is the height to width (slenderness) ratio of adolescent vertebrae. In women, vertebral body height increases by 50% during adolescent growth, but vertebral body width only increases 15%. Men have wider vertebrae during their adolescent growth period and their thoracic kyphosis is at or near its maximum (47).
Epidemiology The prevalence of scoliosis (proportion of the population affected at a given time period) as reported by various screening programs varies over a range, from 0.29% to 14.4% (34,48,49,50,51,52,53). This range is primarily because of the criteria for referral (51,53). The prevalence for scoliosis treatments has a much smaller range of one to six per 1,000 children screened (51,53). This indicates there is a need for improvement in the current screening methods. The small range of variation for treatment indicates that there is more agreement on when to treat scoliosis than on when to refer.
CASE REPORT TWO BROTHERS
Two Brothers
CHRISTOPHER
The first brother is a 14-year-old Filipino boy with a history of “allergies,” consisting of a runny nose, sneezing, itching of the chest and eyes, and watering of the eyes. The child’s only recorded trauma was a fall he sustained while riding a bicycle approximately 6 years before presentation.
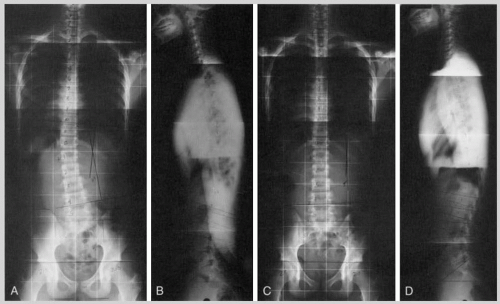
Clinical and Radiologic Findings The clinical signs of subluxation such as fixation dysfunction, edema, tenderness, and skin temperature differentials are present at the L5 segment, the right sacroiliac joint, L1, and C7-T1. The initial AP full-spine radiograph demonstrates an 11-degree thoracolumbar scoliosis (Fig. 14-8A). The lateral full-spine radiograph (in two exposures) shows a retrolisthesis at L5 and hyperextension of the upper lumbar spine (Fig. 14-8B). The thoracic kyphosis appears reduced and the cervical spine has a straight posture with anterior carriage of the head.
Treatment and Follow-Up Short lever arm specific contact manual adjustments (i.e., Gonstead) were primarily directed at L5, the sacrum, L1, and C7. A total of 50 visits over approximately 5 months were made before comparative x-rays were obtained. The AP view shows a reduction of the scoliosis to approximately 4 degrees (Fig. 14-8C). The lateral radiograph demonstrates a slight reduction in the retrolisthesis of L5 (Fig. 14-8D). The cervical lordosis is improved in the lower region of the neck but persists in a kyphotic posture at the segments above. There is less anterior carriage of the head.
CHARLES
This 16-year-old boy is the older brother of the child described above. His symptoms are mostly neuromusculoskeletal in nature, including low back and upper lumbar pain.
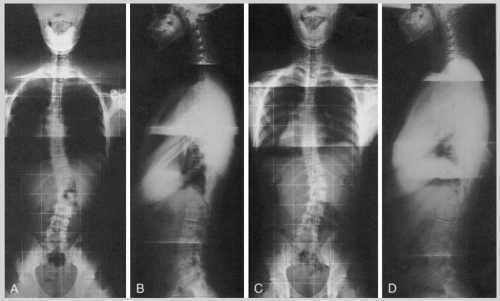
Clinical and Radiologic Findings Signs of subluxation, including motion restriction, skin temperature differentials, edema, and tenderness, were present at L5 and at various levels (e.g., T12, L1, L2) of the thoracolumbar junction. The initial AP radiograph demonstrates a moderate thoracolumbar scoliosis of approximately 30 degrees (Fig. 14-9A). The lateral radiograph shows a hypolordotic upper lumbar spine, a hypokyphotic/lordotic thoracic spine, and a kyphotic cervical spine (Fig. 14-9B). Anterior carriage of the head is present.
Treatment and Follow-Up Short lever arm specific contact manual adjustments (i.e., Gonstead), were primarily directed at L5 and at the apex of the scoliosis. Approximately 50 visits were made during an approximately 6-month period. Follow-up radiographs were obtained. The comparative AP view shows a nearly identical magnitude of the thoracolumbar scoliosis (i.e., ˜30 degrees) (Fig. 14-9C). The comparative lateral findings (Fig. 14-9D) are virtually identical to the initial radiograph (see Fig. 14-9B).
The incidence of scoliosis (rate of new cases) is difficult to determine because many studies that claim to be incidence studies are in fact prevalence studies (51). However, the following facts have been reported: male-to-female ratios at screening vary from 1:1 to 1:3.2 (48,50,51,52); for small curves (6 to 10 degrees), the ratio is 1:1 (52); for larger curves (>20 degrees), the ratio is 1:5.4. Rogala et al. (52) concluded that scoliosis was equally prevalent in both sexes but that larger curves are predominant in women, possibly because of hormonal and familial influences. Others also report a familial tendency for scoliosis (31,50,52) (see case study).
Physical Findings of Progressive Scoliosis
The progressive curve is most often in the thoracic spine, where there is either a local lordosis or a loss of the thoracic kyphosis at the apex when viewed from the true lateral of the apical vertebra as opposed to the lateral view of the patient (41,42,43). In addition, there is usually a decrease in the lumbar lordosis. The clinician should be alert to the
presence of subluxations in the lumbar spine or pelvis that might cause hypolordosis of the lumbar spine (54).
presence of subluxations in the lumbar spine or pelvis that might cause hypolordosis of the lumbar spine (54).
Studies of spinal posture during puberty indicate there is a loss of thoracic kyphosis during the growth spurt (44). The patient is generally taller than his or her peers and his or her pelvis also appears taller than normal (28,45). This may be because of the loss in the lumbar lordosis, increasing the pelvic height on radiographs (44,45).
The patient has less thoracolumbar range of motion (ROM) on flexion/extension as well as lateral flexion and rotation. The loss of ROM is highly correlated with the degree of curvature. Patients with more than a 35-degree Cobb angle have an average of an 8-degree loss in forward flexion, a 7-degree loss in right rotation, a 9-degree loss in left rotation, and an 8-degree loss in both right and left lateral flexion when compared with patients with a Cobb angle of <25 degrees (55).
An examination of the patient’s x-ray will show that, in the thoracic spine, a functional scoliosis has an associated spinous rotation to the convex side (i.e., the spinous process rotates right for a right convex functional scoliosis). With a structural scoliosis, the spinous processes of the thoracic spine rotate to the concavity (spinous process rotates left with a right convex structural scoliosis) (56,57).
Hand Dominance
For small angles there is a significant correlation to hand dominance. However, this is not true for large angles. In a study of 14 subjects with over a 20-degree left convex curve, 10 were right-handed, two were left-handed, and two others were ambidextrous (58). As discussed earlier, the clinician should examine the patient for other neurological conditions if a left scoliosis is found. A high incidence of neurological diseases such as syringomyelia or Arnold-Chiari type 1 malformation have been associated with left convex scoliosis (21).
Back Pain
When compared with adolescents in general, the incidence of back pain is not significantly larger for adolescent scoliotic patients; however, adult scoliotic patients have been reported to have a higher incidence of back pain (59).
Surgery and Back Pain
The conventional theory is that the more vertebrae fused during a scoliosis surgery, the greater the risk of future back pain (60). Paonessa and Engler (61) found that 92% of patients fused from L3 or caudally had suffered from at least one episode of severe low back pain during the past 2 years. They also found that patients with a lumbar lordosis >30 degrees suffered from fewer and less severe episodes of low back pain. They recommended that spinal fusions allow motion below L2 if possible or contouring the fusion so that a lordosis of at least 30 degrees is maintained. However, in a recent cohort study, Poitras et al. (60) investigated the prevalence and nature of back pain for patients who had Harrington rod surgery for AIS. They found that 73% of subjects had back pain during the previous year, but found no correlation with the level of lumbar fusion. Poitras et al. (60) found a slight increase in the incidence of back pain if more lumbar vertebra were fused (69% for L1, 88% for S1), but this increase was not statistically significant. Furthermore, they could not show any relationship between the degree of scoliosis correction and back pain. In a related study, Mayo et al. (62) showed that adult scoliosis patients (including those that had Harrington rod surgery when first diagnosed with AIS) had a greater incidence of back pain compared with the general adult population (73% vs. 56%).
Grubb et al. (63) studied adults with both scoliosis and back pain. They reported that spinal fusion resulted in a reduction of pain by 80% and that the patients had improved tolerance when walking and sitting.
Cosmetic Deformity
In a recent survey (3,60,62,64), scoliosis patients were reported to have a poor body image as well as more visits to their physician and more sick days than the general population. In addition, the effect on social life may be important; it has been reported that 76% of women with scoliosis did not marry (22). However, despite a poor body image, scoliosis patients do have a positive perception of themselves as a whole and are capable of coping with their affliction (4). One might expect that scoliosis patients who were treated using surgery would have a poorer self image than those treated with braces. Paonessa and Engler (61) reported that 79% of Harrington rod surgery patients were satisfied with their appearance after surgery. Patients who received thoracoplasty for the reduction of rib hump reported higher satisfaction with their post-operative appearance than patients who underwent fusion without thoracoplasty (65). This may be a significant finding since conventional surgery has been shown to decrease the Cobb angle as well as the lateral deviation from the spinal axis (mid-sagittal plane), although it does not correct the axial rotation of the vertebra (66).
The reaction of others is probably the principal factor in forming a self-image for those afflicted with scoliosis. This is probably even more important to adolescents, especially girls. Theologis et al. (67) described a cosmetic index whereby others quantified the cosmetic deformity caused by scoliosis. They found that the slight reduction in rib hump when treated with bracing did not significantly change the cosmetic index.
However, for those who underwent Harrington instrumentation, all parameters characterized within the index improved.
However, for those who underwent Harrington instrumentation, all parameters characterized within the index improved.
SCOLIOSIS SCREENING
The U.S. Preventive Services Task Force reports that “there is insufficient evidence to recommend for or against routine screening of asymptomatic adolescents for idiopathic scoliosis” (68), mainly as a result of the lack of evidence indicating that early detection results in better patient outcomes. However, at this point in time several states require all children to undergo screening for scoliosis. The current objective of screening is early detection, including the referral and monitoring of positive cases. The greatest worry is over-referral of healthy children who may then be exposed to unnecessary radiographs and mental stress. When screening, the examiner must keep in mind that the incidence of scoliosis more than 5 degrees is about 4.5%, and for curves more than 20 degrees the incidence is between one and five individuals per 1,000 cases.
A study of current screening methods reveals questionable validity, with a sensitivity of 26%, specificity of 98%, and false positives of 75% (33). This large degree of error is unacceptable, and there is a need to evaluate further the validity of current scoliosis screening. Burwell et al. (35) emphasized the need to define “normal” before screening for abnormal can be performed, and Dickson (34) stressed the need for understanding the clinical course of the disease.
Other studies indicate there is a problem with over-referral and, hence, the over-exposure of children to unnecessary x-ray. Leaver et al. (30) state that screening programs can lead to 10% of 11- to 15-year-old children being referred for x-ray when only one in five of those referred would have a scoliosis, and of those, only one in 10 would require treatment (i.e., bracing or surgery). Burwell et al. (35) describe the forward bending test (visual inspection for scoliosis followed by forward bending for the presence of a rib hump) as being highly sensitive but having too many false positives. When using this procedure, between 1.9% and 15% of the children are referred for x-ray, but only two or three per 1,000 are treated. Howell (36) concludes that educational methods for screeners must be improved and that the criteria for referral need to be better established.
Vercauteren et al. (2) studied the normal variations in symmetry of children aged 7 to 18 years. The study was designed to determine the ranges of physiological normal values for a child’s posture. The left-right measurement discrepancies were quite common among the children: shoulder height, 1.0 cm; scapular height, 1.0 cm; iliac crest height, 1.0 cm; rib hump on forward flexion, 0.8 cm.
The primary purpose of any screening program is to detect the existence of a particular disease or condition. Screening tests are not meant to be diagnostic, but they must sort out the person who may have the disease or condition from those who probably do not. A properly designed screening program requires that the epidemiology and the natural history be well understood (30,37). Epidemiology provides the information that allows society as a whole to determine if the cost of screening programs are economically feasible (30). The natural history allows early diagnosis through understanding the early symptomatic stages of a disease (37). In addition, a thorough understanding of the natural history may aid in treatment as well as in measuring the effect of treatments. Unfortunately, the natural history of scoliosis is not very well understood. There has been a great increase in our understanding of progressive idiopathic scoliosis, and ongoing studies will add to our knowledge base.
For a screening program to be successful, Cochrane and Holland (38) state that it must be simple to administer, acceptable to the subjects, sensitive (give a positive finding when the subject has a scoliosis), and specific (give a negative finding when the subject does not have the disease). In addition, the cost of the program to the community must be compared with the cost of the problem if there was not early detection. Very little information is available on screening cost; however, in a recent U.S. Preventive Services Task Force policy statement, the cost of screening was reported to range between $0.41 and $2.31 per child, and the average cost of treatment of confirmed cases ranged between $3,500 to $3,900 per case (68).
Screening Procedure
Children should be screened at or before 10 years of age. The screening procedure must involve inspection of the entire back from the cervicals to the pelvis:
Children should be wearing shorts or swimsuits; girls should wear a two-piece swimsuit. Gowns exposing the back are not acceptable because gowns hide postural attitudes.
Inspect for lateral spinal deviation, pelvic asymmetry, and/or shoulder asymmetry.
Adams test (forward flexion) differentiates structural from functional scoliosis. The back should be inspected in at least three forward bending positions. The patient holds his/her hands together while bending forward so that they hang in the mid-line of the body:
Bending forward at about 45 degrees, the thoracic spine is examined for rib-hump
Bending forward a few degrees further, the thoracolumbar spine is examined
Bending full forward to examine the lumbar region
Any trunk rotation (rib hump or lumbar hump) should be measured using an inclinometer (also called a scoliometer), or the difference between left and right should be measured in millimeters
The side bending test further differentiates a structural from a functional scoliosis. Functional curves disappear during lateral flexion to the side of convexity, whereas structural curves remain.
Screening Effectiveness
Torrel et al. (71) described the effectiveness of a Swedish screening and treatment program over a 10-year period. The number of patients younger the age of 20 years detected as having a scoliosis of 20 degrees or greater tripled during the first 4 years of the program and reached a plateau after the sixth year. Between the 6th and 10th year, the incidence of scoliosis of 20 degrees or greater was 0.4%. The mean referral age of the patients dropped from 15 to 13 years by the end of the 10-year period reported on by the study. In addition, the Cobb angle of the average scoliosis referral decreased from an average of 46 to 28 degrees. The average Cobb angle of the 10 worse cases for each year also decreased from 63 to 46 degrees.
Screening Thermography
Cooke et al. (72) studied the use of thermography (infrared) for the detection of scoliosis. One hundred fifty-four children were included in the study. Twenty-nine subjects had previously been identified through clinical examination and radiography for the presence of scoliosis (mean, 27 degrees; SD, 12 degrees). A second group of 125 individuals had no history of scoliosis and were asymptomatic. All subjects underwent full-spine radiologic examinations and thermography. Assessment of thermograms selected at random from these two subject pools showed that thermography had a sensitivity of 98.2% and a specificity of 91.0% when compared with the gold standard of radiography. The authors conclude that thermographic examination is a noninvasive and simple means for screening adolescents for scoliosis and recommended it for further prospective large-scale investigations.
CLINICAL EXAMINATION
Posture
When a patient is referred because of a suspected scoliosis, a thorough examination of the patient’s posture is required. The patient’s entire back area including the shoulders must be exposed to determine the presence of any asymmetries or spine humps. It is important to compare postural findings with full-spine radiographs as well as functional testing. The most common causes of functional scoliosis are leg length differences caused by a true anatomical short leg, pelvic asymmetry, or foot pronation. Muscle spasm and pain can also cause a functional scoliosis.
If a scoliosis is obvious during a postural examination, then it must be determined if the curve is structural or functional. Adams test (forward flexion) should be performed as described above. The curve will disappear on flexion if it is functional. If the curve does not disappear, it is common for the torso to rotate during flexion, giving the appearance of a rib hump or lumbar hump. The extent of rib or lumbar humping should be measured with an inclinometer; the left-right difference in the hump can be measured in millimeters. As stated earlier, trunk rotations (rib or lumbar humps) of 7 degrees or more indicate the need for a radiographic examination (69). Rib and lumbar humps having a left-right difference of 11 mm or more also indicate the need for a radiographic examination (70). A lateral flexion test should also be performed. If the curve disappears on lateral flexion to the side of convexity, then the curve is functional.
The clinician should further examine the patient if the scoliosis is a left thoracic scoliosis. As mentioned earlier, a left thoracic curve has a greater likelihood of occurring in patients with syringomyelia or Arnold-Chiari type 1 malformation. In addition, cafe-au-lait spots may be indicative of neurofibromatosis. A patch of hair over the lumbosacral region may indicate diastematomyelia. Ehlers-Danlos syndrome is associated with abnormal scarring and extreme elasticity of the skin. Additional spinal examination procedures that are usually performed are covered in Chapter 5.
Radiography
If it is determined that radiographs are necessary, then a minimum of two radiographs must be taken: (1) full spine AP (or PA) and (2) full-spine lateral (see Chapter 4). The PA radiograph has been advocated because it provides better protection of breast and/or reproductive tissue from radiation exposure (73). However, if adequate prepatient shielding is available, then the AP view is preferred because the patient can be positioned closer to the bucky without head or cervical spine rotation. In addition, the use of rare-earth gradient screens, three-phase or high-frequency generators, gonadal shielding, and a high-density grid all reduce the radiation exposure to the patient (74).
A full view of the spine from the ischial tuberosities to the top of the cervical spine is the ideal exposure.
This allows for an examination of the pelvis and femur heads as well as the location of the head relative to the pelvis. Complete visibility of the ischial crest is also important because the degree of apophyseal fusion is a key method for determining skeletal age (Risser’s sign; this method is described in more detail in the next section).
This allows for an examination of the pelvis and femur heads as well as the location of the head relative to the pelvis. Complete visibility of the ischial crest is also important because the degree of apophyseal fusion is a key method for determining skeletal age (Risser’s sign; this method is described in more detail in the next section).
The PA radiograph gives a slightly larger distortion of the spine because the spine to film distance is increased. The distortion is greater for those vertebrae furthest from the central ray. Thus, the clinician must be consistent if comparisons are to be made. The cervical spine is sometimes distorted so that it gives the appearance of a pillar view in some PA films. Positioning of the patient is crucial, as is the anatomical location of the central ray. The slightest change in radiographic protocol can change the Cobb angle by several degrees.
On the AP (or PA) radiograph, the rotation of the spinous process should be examined in the area of the scoliotic curve. If the spinous rotation is caused by a functional lateral flexion of the spine (i.e., leg length inequality, hemivertebrae, or pelvic asymmetry), then the spinous process rotates to the contralateral side (i.e., spinous process rotates right for a right functional scoliosis). With a structural scoliosis, the spinous process rotates to the concavity (spinous process rotates left with a right scoliosis).
Barge (75) recommends that a sacral base radiograph be used to determine any asymmetry in the sacrum or L5 because the standard AP (or PA) full-spine view does not usually provide an adequate view of these structures. Barge reports that 29% of scoliosis patients have a level sacral base, 32% have a low right sacral base, and 39% a low left sacral base. In the early stages of scoliosis, Dickson et al. (76) recommend close examination of the sacrum. In a study of more than 1,700 children, Dickson et al. (76) found 2.5% to have a scoliosis of >10 degrees. Of these, 21% (0.53% of the total group) were caused by sacral tilt. None of the children with scoliosis caused by sacral tilt had any progression in the scoliosis (76).
It is also recommended that a recumbent radiograph be ordered, with the patient laterally flexing to the side of the convexity, in an effort to reduce the curve as much as possible. This provides insight on the flexibility of the curve as well as information on the effect gravity has on the curve. The more a curve corrects on the recumbent radiograph, the less the curve will progress (77).
Most chiropractic clinics do not have the ability to perform a recumbent radiograph. As an alternative, lateral flexion radiographs are recommended to determine the flexibility of the curve and examine potential sites for spinal adjustments (18). Motion segments that have a loss of normal motion should be examined closely to determine if the fixation is caused by soft tissue or anatomical changes in the vertebra.
Recently, Beauchamp et al. (78) reported that the Cobb angle has a diurnal variation of about 5 degrees. They recommend that follow-up radiographs be performed at the same time of day as the initial x-ray. It has long been known that the intervertebral disc has a diurnal variation in height, so it should not be surprising that the Cobb angle may vary as well. Gravitational forces on the disc would not be as uniform in scoliotic patients, causing changes in disc height through the day in such a way as to affect the Cobb angle.
PREDICTING SCOLIOSIS PROGRESSION
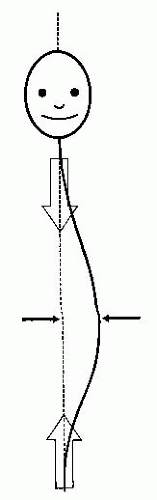
By convention, the most important factor for predicting curve progression is the Cobb angle of the patient’s scoliosis at first discovery. By one model of spinal mechanics, a large curve is more likely to progress than a small curve. Figure 14-10 shows the loads and torque acting on the apical vertebra for a scoliotic spine. The larger the Cobb angle, the larger the torque acting on the apical vertebra, and thus the greater likelihood for progression.
However, existing angle is not the only factor in scoliosis progression; age and the extent of rib-cage deformity are also factors that have been shown to play a role in affecting progression according to Lonstein and
Carlson (86). Specifically, a Cobb angle >20 degrees in a patient of a young skeletal age increases the likelihood of progression. The next few paragraphs summarize methods for estimating skeletal age.
Carlson (86). Specifically, a Cobb angle >20 degrees in a patient of a young skeletal age increases the likelihood of progression. The next few paragraphs summarize methods for estimating skeletal age.
Risser’s method (79) is one of the easier procedures for determining skeletal maturity. With age, the iliac crest epiphyseal plate closes from the caudad end towards the cephalic end of the ilium (Fig. 14-11). This progression moves from the anterior towards the posterior portion of the ilium.
The crest is divided into four quadrants, and the location of epiphyseal excursion is graded as follows:
Grade 1 = 25% excursion
Grade 2 = 50% excursion
Grade 3 = 75% excursion
Grade 4 = 100% excursion
Grade 5 = Full excursion and complete fusion
For example, a patient with a Risser’s sign of 1 is more likely to have a scoliosis progress because the skeleton is relatively immature and the patient’s growth rate is likely to be rapid in the near future.
Radiographs of the wrist are the classic means of identifying skeletal age (80). However, this requires additional radiation exposure at a time when it can be most harmful to developing tissue. In addition, it has been shown that there is an increase in spinal height after skeletal maturity has been achieved (as measured by wrist radiography). That is, the spinal column continues to grow after skeletal maturity. For girls, the sitting height increases an average of 6.9 mm 1 year after skeletal maturity and 14.2 mm 3 years after maturity. For boys, the increase is even more dramatic, averaging 13.5 mm 1 year after maturity and 16.2 mm 2 years after maturity (81). Examining the epiphyseal plates of the vertebral bodies to confirm skeletal maturity is not a reliable means of verifying maturity because the true epiphysis is not visible on radiographs. The radiographically obvious ring apophyses are the result of traction on the vertebra from the anulus of the disc (81).
TABLE 14.2 Alkaline Phosphatase Level and Skeletal Maturity | ||
|---|---|---|
|