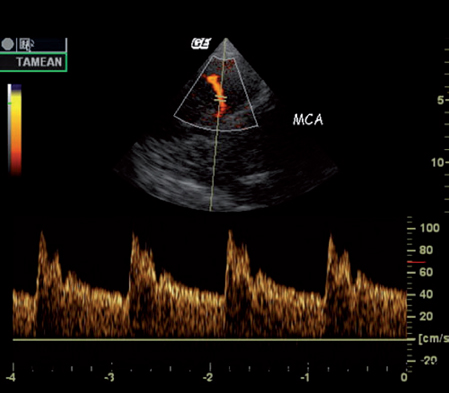
17 Rhesus Isoimmunization E. Albert Reece Rhesus (Rh) isoimmunization occurs when a pregnant woman develops antibodies in her blood in response to antigens on the surface of fetal red blood cells that have traversed the placenta. These antibodies cross the placenta and coat the fetus’ red blood cells, which are then destroyed in the fetus’ spleen. This erythrocyte-destroying, or hemolytic, process is called isoimmunization, which can result in the fetus eventually developing severe anemia and other blood disorders (Fig. 17.1). In severe cases, it can even cause death. An antibody isolated from human plasma, called RhoGAM (RH0[D] Immune Globulin), can neutralize this isoimmunization reaction between an Rh-negative woman and her Rh-positive offspring. Before the widespread use of the RhoGAM, the most common cause of isoimmunization was sensitization to the Rh or D antigen. However, because prophylactic RhoGAM has been so successful in preventing women from becoming Rh(D) sensitive, cases of isoimmunization to other red blood cell antigens have become more prevalent. Fig. 17.1 A blood smear examination of patient with hemolytic anemia reveals red blood cell fragments, an unusually large number of reticulocytes (immature erythrocytes), or atypically small, round cells (darker cells) In the management of an Rh-sensitized pregnant patient, it is important to know the blood types of the father and of the fetus. Unless documented otherwise, fetal blood should be considered Rh-positive. If, after testing, the fetus is Rh-negative, the maternal antibody will not cause hemolytic disease. If the father is homozygous Rh-positive, the fetus will be Rh-positive, and further fetal surveillance is mandatory. If he is heterozygous Rh-positive, there is a 50% chance that he has passed the D antigen to the fetus and further testing is warranted. If he is Rh-negative, further surveillance is unnecessary. The most likely zygosity at the Rh(D) locus of a father can be estimated using race, serology, and the Rh-antigen status of his offspring from previous pregnancies. Recent evidence suggests that an Rh(D) deletion results in the majority of Rh(D)-negative phenotypes among Whites. Increasingly, Doppler ultrasonography is being used to help diagnose severe hemolytic disease in the fetus, particularly of hydrops fetalis, a severe condition in which the fetus develops systemic edema and a build-up of fluid (perfusion) in body cavities such as the pericardium, thorax, and abdomen. Doppler examination of the middle cerebral artery is performed to measure the intensity of blood flow (Fig. 17.2). This measurement has been shown to correlate with the severity of anemia in the fetus (Evidence Box 17.1). Fig. 17.2 Doppler ultrasonogram of the middle cerebral artery of a fetus The incidence of Rh(D) hemolytic disease in newborns in the United States is approximately 10.6 per 10 000 total births, corresponding to approximately 4000 affected infants nationwide. However, approximately 15% of the White female population are Rh-negative and, therefore, at risk for developing Rh isoimmunization when they become pregnant. Only 5–8% of African-Americans are Rh-negative, and it is rare in other populations, except for the Basque region of Spain where it is extraordinarily high (Table 17.1).
Definitions

Diagnosis
Prevalence and Epidemiology
| Population | Incidence (%) |
| Chinese and Japanese | 1 |
| North American Indian and Inuit | 1–2 |
| Indo-Eurasian | 2 |
| African-American | 4–8 |
| Caucasian | 15–16 |
| Basque | 30–35 |
Etiology
Historically, isoimmunization to the Rh(D) antigen has been the most common and clinically important form of immune sensitization occurring in pregnancy. As a result of the development of RhoGAM, there has been a dramatic decrease in the incidence of Rh isoimmunization among pregnant women in most developed countries.
Even with the substantial decrease in Rh(D) hemolytic disease over the past 40 years, Rh isoimmunization continues to be a problem among pregnant women. This is because some women become sensitive to other blood antigens for which there is no prophylactic treatment.
Maternal antibodies to all non-D antigens are collectively referred to as “irregular antibodies.” Although they may occur naturally as a result of pregnancy, the majority develop as the result of blood transfusions. This type of sensitization occurs because most blood transfusions are compatible only with ABO and Rh(D) antigens.
Many of these irregular antibodies, similar to Rh(D), can produce severe disease in the neonate, including profound fetal anemia and hydrops fetalis. Because many others are likely, maternal antibody screening should at least search for those already demonstrated to cause problems.
Hemolytic diseases caused by sensitization to irregular antibodies now accounts for the largest percentage of isoimmunized pregnancies in the developed world. The presence of irregular antibodies is not related to the mother’s ABO type or Rh status, and it is possible to become sensitized to more than one type of red blood cell antigen.
In addition to the clinically relevant Rh group, non-Rh groups such as Kell, MNS, Dufy, and Kidd (Table 17.2) have assumed increasing importance as the incidence of Rh (D) sensitization has decreased. Nonetheless, sensitization to Rh antigens (non-D) is still responsible for the largest proportion of hemolytic disease in the newborn.
In addition to blood antigen incompatibility, various other situations, such as an amniocentesis or an abortion, may increase the risk of an Rh-negative mother developing Rh isoimmunization (Table 17.3).
| Rh: D, E, c, C, Cw, e | Dia, Dib, PP1Pk, Far, Good, |
| Kell: K1, Kpa, k, Jsa, Jsb | Lan, LW, Mta, U, Wra, Zd |
| Dufy: Fya | |
| MNS: M, S, s, N | |
| Kidd: Jka |
| Event | Incidence of significant fetomaternal hemorrhage (%) |
| Chorionic villus sampling (CVS) to identify chromosomal abnormalities and other inherited disorders | 14–18 |
| Amniocentesis | 6–15 |
| Cordocentesis | 40 |
| External cephalic version | 1.8–6 |
| Molar pregnancy | Sensitization has been reported |
| Spontaneous abortion | 1.5–2.0 |
| Elective termination | 4–5 |
| Threatened abortion | 11 |
| Third-trimester bleeding | 4–8 |
| Uneventful pregnancy | 2.6–8 |
Pathophysiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


