Background
Preterm birth (PTB) is a significant cause of neonatal morbidity and mortality. Studies have shown that vaginal progesterone therapy for women diagnosed with shortened cervical length can reduce the risk of PTB. However, published cost-effectiveness analyses of vaginal progesterone for short cervix have not considered an appropriate range of clinically important parameters.
Objective
To evaluate the cost-effectiveness of universal cervical length screening in women without a history of spontaneous PTB, assuming that all women with shortened cervical length receive progesterone to reduce the likelihood of PTB.
Study Design
A decision analysis model was developed to compare universal screening and no-screening strategies. The primary outcome was the cost-effectiveness ratio of both the strategies, defined as the estimated patient cost per quality-adjusted life-year (QALY) realized by the children. One-way sensitivity analyses were performed by varying progesterone efficacy to prevent PTB. A probabilistic sensitivity analysis was performed to address uncertainties in model parameter estimates.
Results
In our base-case analysis, assuming that progesterone reduces the likelihood of PTB by 11%, the incremental cost-effectiveness ratio for screening was $158,000/QALY. Sensitivity analyses show that these results are highly sensitive to the presumed efficacy of progesterone to prevent PTB. In a 1-way sensitivity analysis, screening results in cost-saving if progesterone can reduce PTB by 36%. Additionally, for screening to be cost-effective at WTP=$60,000 in three clinical scenarios, progesterone therapy has to reduce PTB by 60%, 34% and 93%. Screening is never cost-saving in the worst-case scenario or when serial ultrasounds are employed, but could be cost-saving with a two-day hospitalization only if progesterone were 64% effective.
Conclusion
Cervical length screening and treatment with progesterone is a not a dominant, cost-effective strategy unless progesterone is more effective than has been suggested by available data for US women. Until future trials demonstrate greater progesterone efficacy, and effectiveness studies confirm a benefit from screening and treatment, the cost-effectiveness of universal cervical length screening in the United States remains questionable.
Preterm birth (PTB), defined as a birth less than 37 weeks of gestation, is a major public health problem and imposes an economic burden on society. In the United States, approximately 450,000 infants each year are born prematurely; that is, 1 in every 9 births. The majority of these PTB are spontaneous and not the result of iatrogenic delivery due to maternal or fetal indications. Annual United States health care expenditures associated with PTB total at least $26.2 billion dollars, or $51,600 per PTB. Preterm infants are more likely to develop cerebral palsy, developmental delays, and intellectual disabilities that reduce their quality of life. PTB is also a burden for families, both emotionally and financially.
The risk of a PTB is affected by factors that include prior birth history, multiple gestation, and cervical length. Investigators have found that shortened cervical length in the second trimester of pregnancy is a major risk factor, demonstrating that cervical length is inversely related to the risk of PTB. One randomized, controlled trial conducted in the United Kingdom, Greece, Brazil, and Chile found that vaginal progesterone (200 mg) treatment of women diagnosed with shortened cervical length reduces the risk of PTB before 33 weeks by 44%. A recent multinational, phase III, double-blind clinical trial that studied 206 US women of a total 459 enrolled women demonstrated that administration of daily 8% vaginal progesterone gel (90 mg) to women diagnosed with shortened cervical length (10-20 mm), measured using vaginal ultrasonography in the mid-trimester, was associated with a 45% reduction in PTB before 33 weeks and with improved neonatal outcomes. Four published cost-effectiveness analyses of universal cervical length screening and treatment with vaginal progesterone concluded that universal screening was a cost-effective strategy to prevent PTB. These analyses assumed 45%, 41%, 39%, and 45% PTB reductions in the progesterone groups, respectively. Based on the existing literature of cost-effectiveness analyses, a recent report recommends universal cervical length screening at 18 to 24 weeks of gestation in women with singleton gestations and offering vaginal progesterone to those with a CL ≤25 mm, regardless of the history of spontaneous preterm birth.
In 2012, the Reproductive Health Drugs Advisory committee of the United States Food and Drug Administration (FDA) considered the benefits and risks of progesterone gel for the proposed indication of PTB prevention in women with shortened cervical length. The primary aim of the review was to evaluate progesterone efficacy. In the review, reanalysis of the phase III, randomized, placebo-controlled double-blind trial showed that progesterone reduced PTB less than 33 weeks by only 11% in the US cohort compared with an 80% reduction in non-US women. Thus, the efficacy of progesterone for women with shortened cervical length assumed in prior cost-effectiveness analyses may not be applicable to US women. The aim of this study was to perform a cost-effectiveness evaluation of universal cervical length screening and treatment with progesterone to prevent PTB (≤33 weeks) compared with no screening, considering various levels of progesterone efficacy (ie, percent PTB reduction compared with no treatment).
Materials and Methods
We developed a base-case decision analysis model to compare universal screening with no screening for PTB prevention in asymptomatic women with a singleton pregnancy and no history of spontaneous PTB. Our base-case model included a mixed population, both nulliparous women and multiparous women with one or more prior term births and no prior PTB. The screening strategy was based on the American College of Obstetricians and Gynecologists guidelines, which considers, but does not recommend, universal cervical length screening for asymptomatic, low-risk women. We defined PTB as ≤33 weeks, based on the Hassan trial. We defined short cervical length as ≤20 mm, to be consistent with both ACOG and SMFM guidelines and previous cost-effectiveness analyses. This is in contrast to the definition of shortened cervical length actually used in the Hassan trial and Pizzi cost-effectiveness analysis (ie, 10-20 mm). The screening strategy included the cost of a single transvaginal sonogram performed between 19 and 23 weeks of gestation. Because this study used data available through other published literature, University of Alabama at Birmingham IRB review or approval was not required. We used TreeAge Pro 2014 software to perform all the analyses.
The primary outcome of our study was the cost-effectiveness ratio, defined as the cost in US dollars to achieve one quality-adjusted life-year (QALY) for the progeny of women with shortened cervical length. The incremental cost-effectiveness ratio (ICER) was calculated for the base case model. The ICER represents the incremental cost for screening associated with incremental QALYs gained. We compared cost-effectiveness ratios for both the screening and no-screening strategies using baseline estimates (from literature-based sources) as depicted in Tables 1 and 2 . Costs and QALYs were discounted at a baseline rate of 3% per year.
| Variables | Estimate | SD |
|---|---|---|
| Prevalence of cervical length ≤20 mm | 0.0228 | 0.0008 |
| PTB reduction with progesterone | 11% | |
| Probability of PTB ≤33 weeks | ||
| Cervical length ≤20 mm | 0.2270 | 0.0375 |
| Cervical length >20 mm | 0.0903 | 0.0345 |
| Probability of neonatal death if delivered | ||
| ≤33 weeks | 0.0352 | 0.0041 |
| >33 weeks | 0.0008 | 0.0001 |
| Probability of disability of newborn if delivered | ||
| ≤33 weeks | 0.1132 | 0.0003 |
| >33 weeks | 0.0291 | 0.0018 |
| Variable | Estimate | Low | High |
|---|---|---|---|
| Cost of maternal care if delivered | |||
| ≤33 weeks | 9052 | 4526 | 18,104 |
| >33 weeks | 4015 | 2008 | 8031 |
| Cost of neonatal care if delivered | |||
| ≤33 weeks | 104,174 | 52,087 | 208,349 |
| >33 weeks | 4352 | 2176 | 8705 |
| Cost of early intervention if delivered | |||
| ≤33 weeks | 6388 | 3194 | 12,775 |
| >33 weeks | 1132 | 566 | 2264 |
| Cost of severe disability in progeny | 110,462 | 55,231 | 220,923 |
| Cost of each cervical ultrasound | 77 | 53 | 306 |
| Cost of vaginal progesterone course | 625 | 420 | 3125 |
| Cost of 2-day maternal hospitalization | 7787 | 5900 | 9675 |
| QALY for death | 0 | — | — |
| QALY for disability | 18.01 | 15 | 24.01 |
| QALY for healthy | 30.01 | — | — |
The probability of PTB with cervical length >20 mm was calculated using data published in a systematic review by Honest et al. The prevalence of PTB in US women was obtained from national vital statistics. For our base-case model, the prevalence of short cervix and the probability of PTB with short cervix were derived from 2 randomized, controlled trials. The efficacy of progesterone for reducing PTB in the base-case model was acquired from the FDA report on reanalysis of trial data for US women. We also developed 3 other analogous models. On the basis of data from Facco and Simhan, we estimated the effect of birth history and developed one model for nulliparous women and another for multiparas with only prior term birth(s). The third model included the costs of additional (serial) screening to find a shortened cervix and a 2-day hospital admission for women with shortened cervical lengths (eg, for observation and to receive antenatal corticosteroids for fetal lung maturation).
To address inherent uncertainties in the model parameter estimates, we conducted a probabilistic sensitivity analysis of our base-case model using Monte Carlo simulations (a computational algorithm that relies on repeated random sampling) with 1000 trials and 1000 samples within each trial. For this analysis, we estimated the effects of two types of distributions. First, for the probabilities we estimated distributions based on the probability and the sample size from which the probability was estimated. The variable estimates and associated standard deviations of the distributions are shown in Table 1 . Second, we used triangular distributions, where the variable estimate ( x ) is the mode; with ( y ) and ( z ) representing the upper and lower limits for the distributions for cost and QALY estimates. QALY for different health states were calculated by discounted life expectancy and utility of health states. Health states were evaluated using the 3 categories of utility used by Werner et al, where utility = 1 and utility = 0.61 were assigned to normal health and severe disability, respectively; the utility for death was set at 0 ( Table 2 ).
Results
In our base-case model, the screening strategy was more costly, $22,913 per delivery, compared with $22,755 per delivery for no screening, but yielded slightly more QALYs, 29.453 compared with 29.452 for no-screening. The ICER for screening was $158,000/QALY. Consistent with the FDA reanalysis of US data, our base case assumed that progesterone only reduces the likelihood of PTB by 11% in US women with shortened cervical length.
Varying progesterone efficacy from 0% to 90% PTB reduction in a 1-way sensitivity analysis, we found that screening would be a dominant strategy (ie, less costly and more effective) when progesterone reduced PTB by more than 36% ( Table 3 ). For any progesterone efficacy level less than a 36% reduction in PTB, the ICER of screening had positive values, which indicated that screening was more effective but also more costly. Similar analyses were performed for nulliparous women and multiparous women with only prior term birth(s). For nulliparous women, a progesterone efficacy had to result in a 27% reduction, and for women with only prior term birth(s), progesterone had to be more effective, requiring a 59% PTB reduction for universal screening to be cost-saving.
| PTB reduction with progesterone | Strategy | Cost | Effect | ΔC | ΔE | ICER (ΔC/ΔE) |
|---|---|---|---|---|---|---|
| 0% | No screen Screen | 22,755.41 22,983.71 | 29.452 29.452 | — 228.30 | — 0 | 0 |
| 18% | No screen Screen | 22,755.41 22,868.70 | 29.452 29.454 | — 113.29 | — 0.002 | 56,645.00 |
| 36% | No screen Screen | 22,755.41 22,753.68 | 29.452 29.456 | — -1.73 | — 0.004 | (Dominated) |
| 54% | No screen Screen | 22,755.41 22,638.67 | 29.452 29.458 | — -116.74 | — 0.006 | (Dominated) |
| 72% | No screen Screen | 22,755.41 22,523.65 | 29.452 29.460 | — -231.76 | — 0.008 | (Dominated) |
| 90% | No screen Screen | 22,755.41 22,408.64 | 29.452 29.461 | — -346.77 | — 0.009 | (Dominated) |
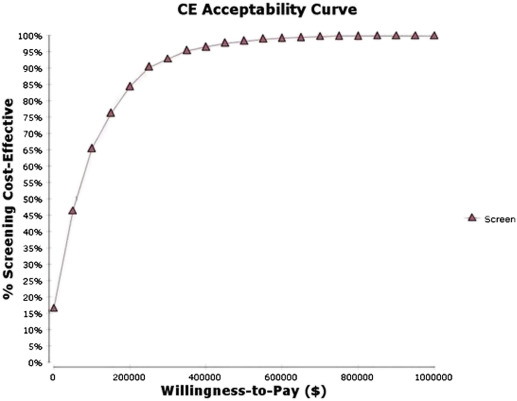
Monte Carlo simulations were used to perform a probabilistic sensitivity analysis in which all model parameters were varied simultaneously. Figure 1 provides a cost-effectiveness acceptability curve derived from these simulations, plotting the probability that screening would be preferred to no-screening against willingness-to-pay (WTP). There is a 15% chance that universal screening would be cost-saving, indicating it would be preferred even if WTP were $0. As WTP increased, so did the likelihood that screening would be the preferred strategy. However, the probability that screening would be the preferred strategy did not exceed 50% until WTP exceeded $60,000. Screening would be a preferred strategy 64% of the time if WTP were $100,000, and WTP would have to be $1,000,000 or more for screening to be the preferred strategy 100% of the time.
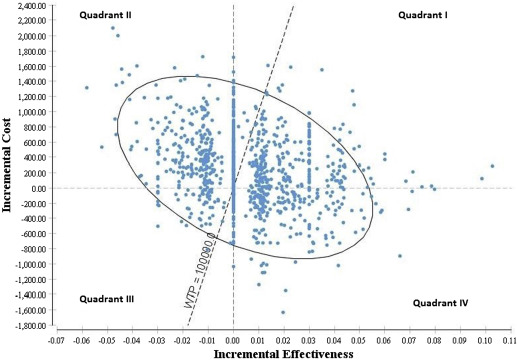
The cost-effectiveness plane ( Figure 2 ) shows a 4-quadrant diagram in which the x -axis represents the incremental QALYs (▵E) and the y -axis represents the additional cost of gaining (▵C) those QALYs for screening versus no screening. We analyzed 1000 iterations of screening compared with the no-screening strategy, represented by a scatterplot in Figure 2 . Screening dominated (ie, less costly and more effective) no screening only 23% of the time, represented in the lower right quadrant (Quadrant IV). Screening was inferior to no screening (ie, more costly and less effective; upper left quadrant; Quadrant II) 44% of the time. The upper right quadrant (Quadrant I) reflects the situation in which screening would be more effective but at an increased cost (+▵C; +▵E). The lower left quadrant (Quadrant III) represents situations where screening would be less effective but with lower cost (−▵C; −▵E). The $100,000 WTP line in the graph represents the ceiling ICER (ie, all the points below the line represent iterations in which screening would be considered cost-effective at the specified WTP of $100,000). The ellipse in the graph represents the 95% confidence interval.