Background
More than a decade ago, researchers described a survey of Maternal Fetal Medicine fellows that showed that chorionic villus sampling training was limited for Maternal Fetal Medicine fellows in the United States. Prenatal screening and diagnosis have rapidly evolved since then and include the introduction of noninvasive aneuploidy screening that uses cell-free fetal DNA. Yet, chorionic villus sampling remains the only method available for first-trimester genetic diagnosis.
Objective
This study evaluated the chorionic villus sampling training of Maternal Fetal Medicine fellows with respect to availability, competency standards, and education methods.
Study Design
In November 2015, an electronic survey was sent to Maternal Fetal Medicine fellows and fellowship directors of accredited Maternal Fetal Medicine fellowship programs in the United States.
Results
Fifty-eight percent of fellows (179/310) and 46% of program directors (35/76) responded. Ninety-five percent of Maternal Fetal Medicine fellows think that invasive diagnostic testing is essential to their training; 100% of fellows have amniocentesis training; and 65% have chorionic villus sampling training. The median number of chorionic villus sampling procedures that are expected during a fellowship in those who trained was 10. Eighty-eight percent of fellows and 89% of program directors state that chorionic villus sampling training could be better; 89% of fellows and 97% of directors would like access to simulated models. Barriers to training included lack of patients (71%) and lack of proficient attending supervisors (43%).
Conclusion
Since the last survey, >10 years ago, chorionic villus sampling training has declined further. A decrease in the number of procedures that are performed is the leading barrier to this training.
Over a decade ago, Jenkins et al described a survey of Maternal Fetal Medicine (MFM) fellows that showed chorionic villus sampling (CVS) training was limited; the average number of procedures that were performed by graduating fellows were <30. At the time, there was a great desire by those graduating fellows to perform the procedure. The low numbers were especially concerning considering the relationship between procedure-related loss and practitioner experience. Over the same decade, the number of United States trained MFM fellows has tripled and has created greater stress on training programs.
In the years since the initial survey, the field of prenatal diagnosis has evolved rapidly. The American College of Obstetrics and Gynecology and American College of Genetics and Genomics published guidelines recommending that invasive prenatal testing be made available to all pregnant patients in 2007 and 2008, respectively. This led to a brief rise in the overall number of procedures until the introduction of noninvasive prenatal screening with cell-free DNA screening in 2011. Screening for fetal aneuploidy with the use of cell-free DNA has a higher sensitivity than conventional screening and has led to a decrease in CVS procedures. The overall impact on procedure rates because of the introduction of chromosomal microarray as a valuable tool to detect clinically relevant copy number variants is unclear, although it may swing the pendulum back towards increased uptake of prenatal diagnosis. When cell-free DNA screening results are positive, providers may lean towards confirmatory testing with amniocentesis, thereby further decreasing the volume of CVS procedures. Despite this, CVS remains the only option for definitive first-trimester genetic diagnosis. Entering the placenta to withdraw villi requires precision and can be made more challenging by placental location, maternal habitus, and multiple gestations and inherently carries a risk of procedure-related loss.
Training in CVS and amniocentesis has long been an expected component of MFM fellowship, with a strong belief that learning curves for CVS are longer than that for amniocentesis. When CVS was introduced originally, requirements for a minimum number of procedures performed was strongly suggested. To date, there is no consensus about the number of CVS procedures that are required to ensure competency. The Society for Maternal Fetal Medicine does not specify requirements for the numbers of procedures that trainees must or should have performed before graduation and defers policies to individual programs. Currently, a leading manufacturer of transcervical catheters requires practitioners to attest to supervision and performance of at least 25 procedures before receiving supplies. California was the first, and so far only, state to regulate this procedure in 2011 by requiring 25 procedures annually to supervise trainees and/or practice independently. It is likely that over time other states, insurance companies, and hospital boards will require proof of volume of procedures to achieve and maintain certification and receive payment.
Training in prenatal diagnostic procedures always has created a challenge because of the nature of the procedure, the inability of a trainer to know exactly what the trainee is feeling/doing, financial pressures for increased efficiency, and the concern for a complication that results in pregnancy loss. The historic medical training construct of “see one, do one, teach one” is no longer the only method for teaching invasive procedure skills to trainees. Some programs begin training on patients who undergo pregnancy termination, and others initiate training on simulation models. A variety of task trainers for amniocentesis and CVS have become commercially available over the last several years. Furthermore, CVS models that use an assortment of rare synthetic substances, supermarket items (ie, raw chicken and gelatin), animal parts, and basic surgical supplies have been reported in the literature.
We aimed to reassess the climate of CVS education ≥10 years after the original report by surveying fellows and program directors. We sought to elucidate current barriers to CVS training, how programs have addressed those barriers, and what training modalities are acceptable to both fellowship directors and trainees.
Materials and Methods
A survey was drafted that used multiple choice and ordinal and categoric scale questions; Institutional Review Board approval was obtained. Data were collected on demographics, clinical experience, program information, and satisfaction with their current invasive training availabilities. This was distributed electronically to 310 MFM fellows who were enrolled in accredited programs within the United States. We expanded on the original study and developed a second survey that was constructed with similar questions that was sent to fellowship directors.
Results
Response rates for MFM fellows and fellowship directors were 58% (179/310) and 46% (35/76), respectively. Representation was from all geographic areas of the United States, with a majority of fellow participation from university-based programs (86%).
All fellowship directors reported that CVS was performed at their institution; 69% reported 0-3 procedures weekly and 92% reported <10 procedures weekly. Training in CVS was offered by 83% of fellowship directors and was initiated at variable times across the fellowship: 46% first year, 27% second year, 27% third year. Most programs (68%) have no requirement for the number of CVS procedures that are required before completion of the fellowship graduation. The median was 22 procedures for the 32% that reported a requirement, with a range of 8–30 procedures.
Of the MFM fellows who responded, 29% were first-year fellows; 35% were second-year fellows; 36% were third-year fellows, and <1% were fourth-year fellows. Fifty percent of fellows reported their program had 1 fellow per fellowship year; 36% had 2, and 13% had 3. Ninety-two percent of fellows reported that CVS was done in their institution, and 65% of fellows had access to training. Eighty-one percent reported that there were 0–3 CVSs per week at their institution, and 92% reported <10 procedures at their institution in total each week. Sixty-nine percent stated that prenatal diagnosis was offered for multiple gestations; 26% were not sure. Seventy-three percent reported that selective reductions were performed at their institutions.
One hundred percent of fellows receive training for amniocentesis; 12% initiate training using simulation, and 22% train on noncontinuing pregnancies, ultimately all moving on to continuing pregnancies. Only 65% of the fellows (116/179) reported availability of training in CVS during their fellowship. The initiation of performing CVS procedures occurred in the first year in 33%, second year in 27%, third year in 39% and 1% in the fifth year of a combined program. Of these, 60% had some training on noncontinuing pregnancies (including those pregnancies that undergo elective termination and those with missed abortions before curettage), and 24% had training on simulators, with all eventually moving on to continuing pregnancies.
Seventy-five percent of fellows report that there is no absolute number of procedures required for proficiency. Twenty-five percent had a specified number of procedures to be completed to be deemed proficient with a median of 20 procedures required and a range of 0–50. Fellows anticipated that they would perform an average of 12 CVS procedures during their fellowship.
When fellows were asked about barriers to adequate CVS training ( Figure 1 ), 71% reported lack of patients, and 43% said they lacked proficient attending physicians. Other barriers to CVS included being too busy with other clinical duties (14%) and not prioritizing CVS training 12%. Fellows were given the opportunity to write in other barriers and reported that procedures were “taken” by attending physicians when they needed them for their own certification and patients’ or attending physicians’ preferences to decline the involvement of trainees.
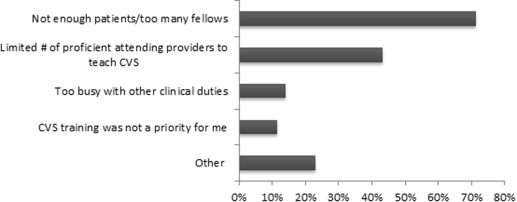
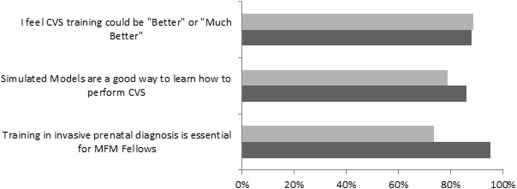
Figure 2 highlights fellow and fellowship directors’ perceptions on CVS training. Eighty-eight percent of fellows and 89% of program directors think that their training in CVS could be better; 89% of fellows and 97% of directors would like access to simulated models, and 93% of fellows and 97% of program directors believe that CVS should be a part of MFM fellowship.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


