Replacement of a Tracheostomy Cannula
Jean Marie Kallis
Introduction
Replacing a tracheostomy cannula is typically a routine and simple procedure. Parents of children with tracheostomies perform this task on a regular basis without the assistance of a health care professional (1).
Although the actual skills involved are generally no more complicated than those used by parents at home, the degree of anxiety present in an emergent situation can make this task more challenging. In addition, with those children who present acutely in the emergency department (ED) for cannula replacement, other factors may be present that increase the complexity of the procedure. These include such things as recannulation in the very young infant, a tracheostomy performed in the previous week or two, the absence of an alternative upper airway, and certain underlying airway conditions. A calm, methodical approach is usually the key to success.
Anatomy and Physiology
A tracheostomy is designed to bypass the upper airway and to provide a direct opening to the trachea. Tracheostomies are performed after endotracheal intubation or for an immediate airway because of three broad and often overlapping clinical problems: acute or chronic airway obstruction, prolonged assisted ventilation, and problems requiring improved pulmonary toilet. More recent data demonstrate a trend toward a larger number of pediatric tracheotomies being performed for prolonged ventilation, congenital anomalies, and severe neurologic disorders, whereas inflammatory upper airway diseases have become less and less of an indication (2,3,4,5,6). Following a tracheostomy, a tract of healing tissue forms between the cervical epithelium and the tracheal endothelium. Until this is well granulated, recannulation may be difficult. Patients are usually hospitalized for a number of days, often in an intensive care setting, to reduce the risk of accidental decannulation, allow sufficient healing, and ensure the primary process is better controlled. Except in unusual circumstances, ED physicians tend to deal with the more mature tracheostomies, which makes reinsertion less challenging (1,2,7,8,9).
The younger the patient, the more likely the occurrence of accidental decannulation or obstruction. Infants have short, thick necks that make them prone to dislodgment of the tracheostomy tube (9,10). Tracheostomy ties may not be snug enough to prevent decannulation. The smaller tracheostomy tubes of young infants also have a narrower internal lumen, making the tubes more susceptible to acute obstruction. Mucous plugging occurs when viscous upper airway secretions occlude the lumen of the cannula, which may already be narrowed by secretions that have previously accumulated and dried. Because infants have less fully developed intercostal and diaphragmatic musculature, they are more likely to be unable to adequately clear a mucous plug from the cannula when it occurs.
Indications
The need to replace a tracheostomy cannula in the ED typically occurs after accidental decannulation or obstruction of the tracheostomy tube (secretions, mucous plug, foreign body) (6,9,11,12). The most life-threatening complications for a child with an artificial airway are cannula obstruction or
dislodgement (2,10). The pediatric patient who decannulates or obstructs a tracheostomy tube while in the ED for another problem can often be managed routinely. However, the child who is brought to the ED for the specific purpose of replacing a tracheostomy cannula may be in significant respiratory distress. Such a patient may arrive via an emergency services ambulance or be carried into the ED by a worried parent. As mentioned previously, the physician who is calm, unhurried, and armed with an awareness that the skills required to manage this situation are relatively straightforward will generally be most effective.
dislodgement (2,10). The pediatric patient who decannulates or obstructs a tracheostomy tube while in the ED for another problem can often be managed routinely. However, the child who is brought to the ED for the specific purpose of replacing a tracheostomy cannula may be in significant respiratory distress. Such a patient may arrive via an emergency services ambulance or be carried into the ED by a worried parent. As mentioned previously, the physician who is calm, unhurried, and armed with an awareness that the skills required to manage this situation are relatively straightforward will generally be most effective.
TABLE 80.1 Equipment for Tracheostomy Change | |
|---|---|
|
Equipment
The equipment required for tracheostomy replacement is listed in Table 80.1, and the sizes for different ages are listed in Table 80.2. There are numerous tracheotomy tubes on the market, and the more commonly used tubes are noted in the latter table. Special features are also available (e.g., cuffs, swivel devices, fenestrated tubes) (6,10,11,13), but these should not distract from establishing a patent airway in the emergency setting.
TABLE 80.2 Approximate Size of Tracheostomy Cannulas, Endotracheal Tubes, and Suction Catheters | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
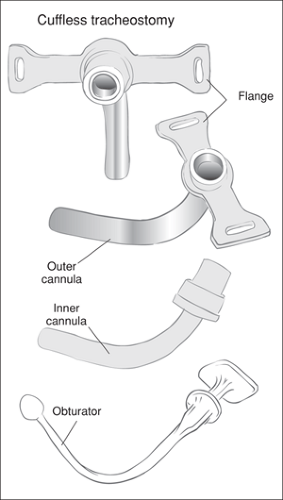 Figure 80.1 Tracheostomy tubes with tube, inner cannula, and obturator. (If the tracheostomy tube is rigid at the distal end, an obturator is necessary to pass the cannula, to reduce the risk of tissue damage. Softer cannulas may not require the use of an internal obturator.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|