FIGURE 17-1 Elbow radiographs of a congenital RUS.
CLINICAL QUESTIONS
- What is the cause of a congenital radioulnar synostosis (RUS)?
- Is it hereditary? Are there any associated syndromes?
- How is congenital RUS classified?
- What are the indications for surgical treatment?
- What are the surgical treatment options?
- Is there an optimal position for fixed forearm rotation?
- What are the complications of surgery for RUS?
- What are the expected outcomes?
THE FUNDAMENTALS
Etiology and Epidemiology
Congenital RUS refers to an abnormal connection between the radius and the ulna due to an embryological failure of formation.1 During the fourth to sixth week of gestation, the upper limb bud develops into the fully formed upper extremity. Between roughly the 37th and 57th day of gestation, a distinct humerus, radius, and ulna are formed. During this period, the forearm arises from a single cartilaginous anlage, which seindenttes longitudinally to form a radius and ulna. Failure of seindenttion results in a congenital RUS. As the seindenttion occurs sequentially from distal to proximal, the RUS characteristically involves the proximal third of the forearm. Furthermore, as the forearm is positioned in pronation in utero, the resulting fusion between the radius and ulna results in varying degrees of fixed forearm pronation.2–5 It has been hypothesized that both congenital RUS and radial head dislocation are developmentally related, distinguished only by subtle differences in the timing of the developmental insult.6
Given that up to 20% of patients will have a positive family history, it is thought that congenital RUS may be inherited in an autosomal dominant fashion with variable penetrance and expressivity.7
Approximately one-third of patients with RUS will have associated syndromes or anomalies, including Apert syndrome, Carpenter syndrome, arthrogryposis, Williams syndrome, and Klinefelter syndrome.3 Other conditions, including polydactyly, syndactyly, carpal coalition, and radial longitudinal dysplasia, have also been associated with RUS. Sex chromosomal anomalies have also been associated with RUS.8
Clinical Evaluation
Given the infrequency with which the condition occurs, diagnosis is often not made until patients are of school age.7 As elbow flexion and wrist flexion-extension are typically unaffected, and young children demonstrate great compensatory rotation through the radiocarpal and midcarpal joints, patients with RUS have little initial functional limitations. The lack of true forearm rotation and usually mild elbow flexion contracture (~20 degrees) are not usually noted early on in life. Later, relatives, teachers, or coaches will identify limitations of forearm rotation with specific activities (e.g., hand washing at school, toilet training due to inability to place the supinated hand to the perineum, catching a ball, swinging a racquet or baseball bat). It is not uncommon for the diagnosis to be made incidentally on radiographs obtained after traumatic events.
Patients will present with fixed forearm pronation (Figure 17-2). In severe cases, “backhanding” may be seen with hand-to-mouth activities or in placing objects in the affected palm. Careful physical examination should be performed, as compensatory rotation through the wrist may mask fixed forearm position. Forearm position can be reliably assessed by determining the axis between the radial and ulnar styloids when the arm is adducted and elbow flexed 90 degrees. Elbow flexion and wrist flexion and extension are preserved, and the distal radioulnar joint is typically stable. In severe cases, forearm segment shortening and abnormal elbow carrying angle may be seen. The majority of patients, however, will have minimal impairment of hand function.9
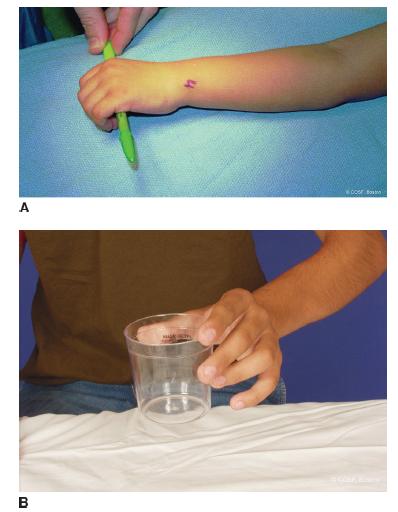
FIGURE 17-2 A: Clinical photographs demonstrating fixed left forearm pronation. B: Compensatory motion is seen through the wrist, simulating forearm supination to neutral.
Radiographs of the entire forearm will demonstrate a bony connection between the proximal radius and ulna; less commonly, there is a more extensive synostosis. At times, the lack of forearm rotation is due to a cartilaginous or fibrous connection between the two bones. The ulnohumeral is typically normal in appearance. The distal radioulnar joint may be distorted in cases of extreme forearm pronation. Depending upon the severity of involvement, there may or may not be a congenital radial head dislocation or absence of the radial head as it is a part of the synostosis. Often a subtle bow to the proximal ulna is seen. This ulnar bow may be a part of the mild elbow flexion contracture commonly noted on physical examination.
Several classification systems have been proposed. Mital classified RUS into two types.2 Type 1 refers to a synostosis between the radial epiphysis and the metaphysis. Type 2 refers to a synostosis distal to the radial physis, associated with a radial head dislocation. Cleary and Omer based their classification upon the morphology and position of the radial head.7 Type 1 patients have a normal-appearing radial head and radiocapitellar alignment with a fibrous synostosis. Type 2 denotes a bony synostosis with a normal appearing, reducted radial head. Type 3 refers to bony synostosis with a hypoplastic and posteriorly dislocated radial head. In Type 4 RUS, the radial head is dislocated anteriorly.
Surgical Indications
Keep it simple, when you get too complex you forget the obvious.
—Al McGuire
Surgery is recommended for functionally limiting loss of forearm rotation; this is dependent upon both the severity of the pronation deformity and whether there is unilateral or bilateral involvement.10 Bilateral involvement with hyperpronation of the forearms results in greater difficulties with daily activities, whereas unilateral involvement with mild pronation position leads to little functional compromise. In their series of 23 patients with RUS observed over 22 years, Cleary and Omer reported that over 95% of patients report little or no limitations with activities of daily living or work.7 Simmons et al.3 and Ogino et al.11,12 both reported that patients with >60 degrees of pronation had difficulties with daily living.
The optimal position of forearm rotation remains controversial. Historically, in cases of bilateral involvement, 30 to 45 degrees of pronation of the dominant limb and 20 to 30 degrees of supination of the nondominant limb were considered ideal.12 Simmons et al.3 advocated that the dominant limb should be positioned in 10 to 20 degrees of pronation with the nondominant limb in neutral rotation. Given the tabletop and keyboarding demands of the modern-day world, mild pronation of both limbs is currently considered ideal.13
SURGICAL PROCEDURES
Not even God can hit a one-iron.
—Lee Trevino
While theoretically reconstructing a proximal radioulnar joint would restore forearm rotation and improve function, attempts at synostosis resection and joint reconstruction have been met with nearuniversal failure. Attempts at simple bony resection have not succeeded.5,14–16 Interpositional arthroplasties with soft tissue and metallic implants have been similarly tried.17 More recently, attempts at synostosis resection and free vascularized tissue interposition have been reported, with gains in short-term forearm rotation.18–21 Given the complexity and morbidity associated with these techniques, in addition to the reliability of simpler surgical strategies, microvascular free tissue procedures have not yet become the standard of care for RUS.
Rather than attempting to create a proximal radioulnar joint where none had ever developed, most current surgical treatment strategies have focused on derotating the forearm-hand unit to a more functional position. A number of techniques have been advocated, all of which involve osteotomies of the radius and/or ulna and derotation from an extreme pronated position to a more functional one. Green and Mital12 advocated osteotomy through the synostosis and K-wire fixation (Figure 17-3). Lin et al.22 described their technique of radioulnar osteoclasis, in which percutaneous osteotomies were performed of the radial and ulnar diaphyses at different levels. After initial osteotomies, no attempt is made at derotation, and a long-arm cast is applied. Approximately 1 week later, the cast is removed and the forearm is derotated under general anesthesia to the desired position. No internal fixation was utilized in their technique, and cast immobilization for an additional 6 to 8 weeks was used until bony healing. A delayed union rate of up to 16% has been reported with this technique.23 Others have advocated variations of this technique using internal fixation with osteotomies of one or both forearm bones.24–28
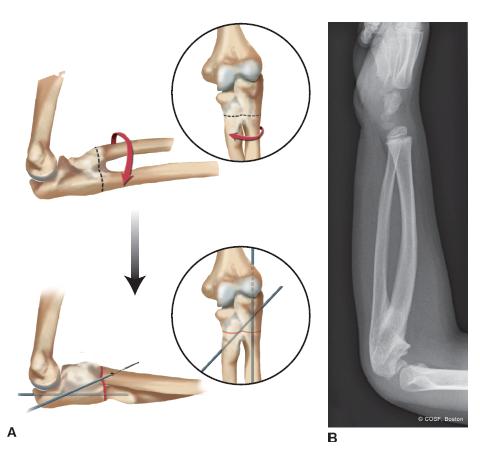
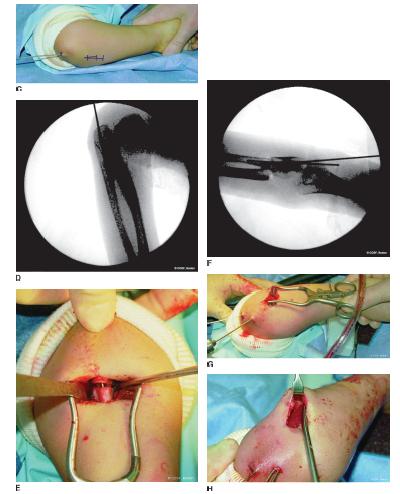
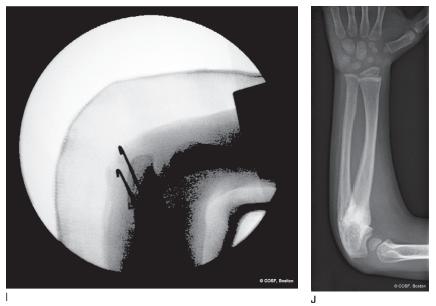
FIGURE 17-3 Derotational osteotomy for congenital RUS. A: Schematic representation of the surgical technique. B: Preoperative radiograph of a 6-year-old boy with a left RUS and hyperpronation deformity. C: Intraoperative photograph depicting the osteotomy incision and trajectory of the IM ulnar K-wire. D: Intraoperative fluoroscopic image after IM ulnar pin has been placed. E: Intraoperative photograph demonstrating the osteotomy cut with IM K-wire evident. F: Radiograph after the second oblique pin has been placed following derotation correction. G: Intraoperative photograph after the second oblique K-wire has been placed. H: Intraoperative photograph depicting the prophylactic forearm fasciotomy. I: Radiographs obtained after final position has been achieved. Note the bulky postoperative dressing and the large girth of the cast to allow for postoperative swelling. J: Follow-up radiographs after 3 months. Note complete bony healing in a position of neutral rotation to slight pronation.
 Radioulnar Synostosis Osteotomy
Radioulnar Synostosis Osteotomy
Under general anesthesia and tourniquet control, fluoroscopic guidance is used to identify the level of the RUS. A longitudinal incision is made over the subcutaneous border of the ulna at the level of the RUS. Careful sub-periosteal elevation is performed circumferentially around the synostosis, with particular attention to avoid buttonholing through the soft tissue envelope anteriorly. Care is made to avoid violation of the elbow joint. After the synostosis is exposed, an appropriately sized stainless steel K-wire is introduced into the olecranon apophysis percutaneously and passed down the intramedullary (IM) canal of the ulna, well beyond the synostosis (Figure 17-3). Care is taken to only make the cortical entry with power and then tap the remainder of the way with a mallet. This prevents false passage of the wire out the opposite cortex, a mishap that can truly prolong your operative time. The IM wire allows for derotation after the osteotomy is made while preventing angulation or translation of the osteotomy fragments.
After the IM K-wire is placed, a transverse osteotomy is performed with the use of a narrow sagittal saw at the level of the synostosis distal to the joint. Copious irrigation is used to avoid thermal necrosis. Judicious placement of small Homan or Bennett retractors will provide adequate soft tissue protection including the posterior interosseous nerve. Care is made to avoid notching or hitting the previously placed K-wire during the osteotomy cut. After the osteotomy is created, the forearm may be gradually derotated into its new position, typically 10 to 20 degrees of pronation. Rotational control and additional stability are then achieved by placing percutaneous oblique K- or C-wires across the osteotomy.
Following confirmation that the appropriate forearm position has been achieved, the wires are bent and cut outside the skin. Under direct visualization and subcutaneous skin flap elevation, limited prophylactic dorsal and forearm fasciotomies are performed to lessen the risk of postoperative compartment syndrome. Periosteum is reapproximated with heavy absorbable sutures, and the wound is closed. A well-padded longarm cast is then applied, which is then bivalved to allow for postoperative swelling.
POSTOPERATIVE
Following derotational osteotomy, patients are admitted for observation, with serial clinical examinations to rule out compartment syndrome. Patients are kept in a long-arm cast for 4 weeks, after which pins are removed. Depending on the age of the patient and degree of radiographic healing, additional cast immobilization for 2 weeks may be needed before discontinuing the cast and initiating range of motion (ROM) exercises.
ANTICIPATED RESULTS
With appropriate patient selection and surgical technique, excellent outcomes can be expected with respect to bony healing and improvement in forearm position. Patients will report high levels of satisfaction with their abilities to perform activities of daily living and other recreational activities. Furthermore, as these patients never had fore arm rotation, the persistent lack of motion is not troubling.
COMPLICATIONS
Early reports of surgical treatment for RUS cite complication rates as high as 36% from surgical treatment.3 Potential complications include infection, loss of position, implant failure, neurovascular compromise, and compartment syndrome.29 Careful soft tissue dissection and retraction, use of prophylactic fasciotomies, and judicious bony resection (see Coach’s Corner) will aid in reducing the risk of these postoperative complications.
Given the tension on the neurovascular structures and the risk for compartment syndrome, percutaneous K-wire fixation confers additional advantages. Postoperatively, if a patient is demonstrating neurological deficits or signs of impending compartment syndrome, the pins may be removed at the bedside, and the forearm allowed to rotate around the IM K-wire back into a position of comfort and safety. This avoids the need for a second anesthetic and allows for immediate intervention, if necessary. This can also be achieved with an external fixation. Plate and screw fixation should clearly be avoided.
CASE OUTCOME
Radiographs demonstrate a congenital RUS. Clinically, the forearm was fixed in 90 degrees of pronation with mild compensatory radiocarpal supination. Given the radiographic findings and functional limitations, the patient underwent derotational osteotomy through the synostosis site, positioning the forearm in 10-degree pronation. Postoperatively there was no neurovascular compromise, and pins were removed at 4 weeks (Figure 17-3). He went on to successful bony union and functional improvement, particularly with personal hygiene, carrying objects, and baseball activities.
SUMMARY
Congenital RUS represents a failure of differentiation in which the proximal radius and ulna are fused, typically in a position of forearm pronation. Clinical presentation and diagnosis are often delayed due to the compensatory supination through the young, flexible wrist. In cases of extreme pronation with accompanying functional limitations, surgical treatment is indicated. Derotational osteotomy through the synostosis site is safe, reliable, and results in improved forearm position.
COACH’S CORNER
Removing the “Napkin Ring” of Bone
Simplify the game as much as possible. When you add, you must subtract
—Don Meyer
In cases of hyperpronation, a great deal of derotation is required to position the forearm and hand in the most functional position. While this can be achieved in a single-stage procedure as described above, excessive derotation can put tension on the adjacent soft tissues and, in particular, neurovascular bundles, especially the interosseous vessels. Given the additional soft tissue swelling that can be expected following any osteotomy and the change in cross-sectional dimensions of the forearm, compartment syndrome is clearly a postoperative risk. From the green circle to the black diamond level of surgery, we perform limited prophylactic dorsal and volar forearm fasciotomies to minimize these risks. With elevation and retraction of the skin flaps, long tenotomy scissors may be used to release the fascia in the region of the osteotomy under direct visualization. This maneuver also facilitates periosteal closure at the osteotomy site and, therefore, bony healing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


