Level 2:
The mid portion of the vagina is attached by endofascial condensation (endopelvic fascia) laterally to the pelvic sidewalls.
Level 3:
The lower third of the vagina is supported by the levator ani muscles and the perineal body. The levator ani muscles form the floor of the pelvis from attachments on the bony pelvic walls and incorporate the perineal body in the perineum. The levator ani, together with its associated fascia, is termed the pelvic diaphragm.
Prolapse
Types of Prolapse
Types of uterovaginal prolapse are classified anatomically according to the site of the defect and the pelvic viscera that are involved (Fig. 7.2).
Fig. 7.2 Types of prolapse. (a) Normal pelvis, (b) uterine prolapse, (c) cystocoele, (d) rectocoele, (e) enterocoele.
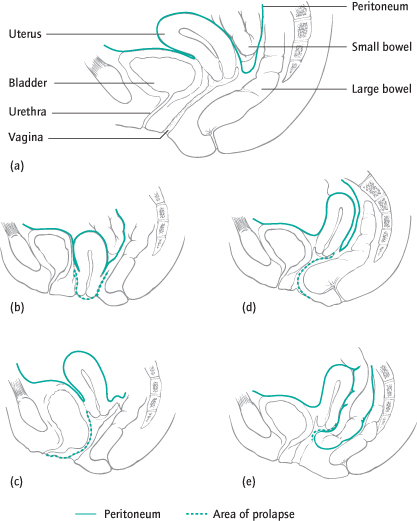
Urethrocoele is prolapse of the lower anterior vaginal wall, involving the urethra only.
Cystocoele is prolapse of the upper anterior vaginal wall, involving the bladder. Often there is an associated prolapse of the urethra, in which case the term cystourethrocoele is used (Fig. 7.2c).
Apical prolapse is the term used to describe prolapse of the uterus, cervix and upper vagina (Fig. 7.2b). If the uterus has been removed, the vault or top of the vagina, where the uterus used to be, can itself prolapse.
Enterocoele is prolapse of the upper posterior wall of the vagina (Fig. 7.2e). The resulting pouch usually contains loops of small bowel.
Rectocoele is prolapse of the lower posterior wall of the vagina, involving the anterior wall of the rectum (Fig. 7.2d).
Grading of Prolapse
There are many grading systems. None is perfect and some are complex and impractical. The Pelvic Organ Prolapse (POP) scoring system of the International Continence Society (ICS) is widely used.
For all measurements, the condition of the examination must be specified, i.e. position of the patient, at rest or straining and whether traction is employed.
The ICS Pelvic Organ Prolapse (POP) Scoring System
| 0 | No descent of pelvic organs during straining |
| 1 | Leading surface of prolapse does not descend below 1 cm above the hymenal ring |
| 2 | Leading edge of prolapse extends from 1 cm above to 1 cm below the hymenal ring |
| 3 | Prolapse extends 1 cm or more below the hymenal ring but without complete vaginal eversion |
| 4 | Vagina completely everted (complete procidentia) |
Female Genital Prolapse
| Anterior wall: | bladder (cystocoele) and/or urethra (urethrocoele) |
| Apical: | uterus, cervix and upper vagina; vaginal vault if previous hysterectomy |
| Posterior wall: | rectum (rectocoele) and/or pouch of Douglas (enterocoele) |
Epidemiology
Half of all parous women have some degree of prolapse and 10–20% seek medical attention.
Aetiology of Prolapse
Attenuation of the vaginal support mechanisms may occur as a result of:
Vaginal Delivery and Pregnancy:
Prolapse is uncommon in nulliparous women. Vaginal delivery may cause mechanical injuries and denervation of the pelvic floor, which contribute to subsequent prolapse. These risks are increased with large infants, prolonged second stage and instrumental delivery.
Congenital Factors:
Abnormal collagen metabolism, e.g. Ehlers–Danlos syndrome, can predispose to prolapse.
Menopause:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


