Preterm Labor and Post-Term Delivery
J. Chris Carey
Ronald S. Gibbs
The authors wish to acknowledge the contributions of Debra Guinn, Lisa Moore, and James N. Martin Jr, to this chapter in the last edition of this text.
Preterm Labor
Preterm birth is a leading cause of neonatal morbidity and mortality. Over the past several decades, there has been a marked increase in survival of very low–birth-weight infants. This increase in survival has been attributed to increased use of corticosteroids, regionalization of perinatal care, improved methods of mechanical ventilation, availability of exogenous surfactant, and improved nutritional therapy. However, the reduction in mortality has not been accompanied by a reduction in neonatal morbidity or long-term handicaps. It is estimated that 50% of all major neurologic handicaps in children result from premature births.
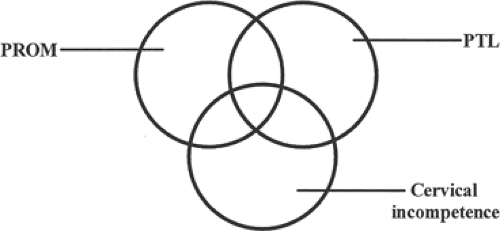
Despite widespread awareness of the problem and use of therapies believed to be beneficial to prevent preterm births, the rate of preterm delivery has increased in the United States. The majority of spontaneous premature births occur to women who develop preterm labor or preterm premature rupture of the membranes (PPROM). Cervical incompetence may also result in preterm delivery. Historically, researchers and epidemiologists have approached these conditions as being distinct processes that were mutually exclusive of one another. Recent evidence would suggest that many women have overlapping conditions that predispose them to deliver preterm. This concept is depicted in Figure 11.1. For example, a woman who has preterm delivery secondary to PPROM at 27 weeks gestation may have had weeks of “silent” or painless contractions or cervical dilation prior to developing ruptured membranes and delivery. Using this broader conceptual framework, this chapter will review the epidemiology, etiology, prevention, and treatment of women with preterm labor.
Mechanisms of Labor Onset
Labor occurs when the uterus converts from a state of containment to an environment that attempts to expel the fetus. In humans, the average gestational period is 280 days ±14 days. Therefore, term labor is defined as labor that occurs between 37 and 42 weeks gestation. Preterm labor is defined as labor that occurs between 20 and 37 weeks gestation. In theory, pathologic activation of the normal parturition process results in preterm labor and delivery.
In both term and preterm labor, following an unknown stimulus, the mechanisms that produce labor override those that maintain the pregnancy. Activation of the parturition process results in membrane activation, cervical ripening, and an increase in myometrial responsiveness to endogenous and exogenous signals. Subsequently, labor progresses along a common pathway that results in uterine contractions that are sufficient to cause progressive cervical dilation to allow for expulsion of the fetus. A number of inciting events have been implicated in premature births. These events include decidual hemorrhage (abruption), mechanical factors (overdistension of the uterus, cervical incompetence), hormonal changes (fetal or maternal stress), or subclinical/clinical infection. Infection is associated with as many as one third of preterm deliveries, particularly those occurring at the earliest gestational ages. The role of infection in preterm labor will be reviewed separately in this chapter.
Animal models have helped in understanding labor. Important findings in animal labor models include an increase in oxytocin receptors present in the myometrium, gap junctions developing between myometrial cells, an increased response to agents capable of producing contractions in the uterus, and physical and biochemical changes of the cervix resulting in a softened consistency. Uterine smooth muscle contractility is produced by the actin–myosin interaction, following myosin light chain phosphorylation, which is controlled by myosin light chain kinase. Myosin light chain kinase is activated by calcium as a calmodulin–calcium complex. Cyclic adenosine monophosphate (cAMP) also regulates kinase by inhibiting phosphorylation. Many factors are involved in this control. Some of the proposed theories of labor will be discussed in the following sections.
Hormonal
Alteration in systemic or local levels of steroid hormones is an initiating factor of labor in some animals. The role of hormonal changes in initiating human labor is less clear. The withdrawal of the uterine inhibitor hormone progesterone has been shown to play a major role in many animals (e.g., sheep, rats, rabbits). In sheep, progesterone withdrawal seems to be caused by an increased responsiveness of fetal adrenal cells to adrenocorticotropic hormone (ACTH), resulting in increased production of cortisol. Through several steps, cortisol redirects placental steroid biosynthesis and decreases progesterone secretion. The decreased circulating progesterone in the sheep leads to increased myometrial gap junction formation, an increase in prostaglandin formation, and increased response of the uterus to agents capable of producing contractions. In this sheep model, fetal ACTH secretion controls the onset of labor.
However, major differences exist, between sheep hormonal status and that of primates, including humans. In humans, there is not a great increase in cortisol from the fetal adrenal gland before labor, nor has a dramatic decrease in progesterone been consistently demonstrated. Yet, progesterone is important in human pregnancy, and numerous studies have examined the role of the progesterone-to-estrogen ratio before the onset of labor. In 1974, investigators demonstrated a significant fall in serum progesterone levels and a rise in estrogen levels in many women before labor. This finding has not been reproduced consistently. Estriol may be a signal from the fetus indicating that it is mature and ready for delivery. Production of estriol increases during the last month of pregnancy. In the large amounts produced, estriol is as active as estradiol in stimulating uterine growth. There are reports of an elevation in the estradiol/progesterone ratio at the end of pregnancy.
The antiprogesterones—RU-486 (mifepristone) and ZK-98299 (onapristone)—in humans and other primates can enhance the responsiveness of the uterus and induce cervical change within 12 to 48 hours, again suggesting a role for progesterone in preventing labor onset.
Administration of progesterone has been demonstrated to prevent preterm birth in humans. The National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network progesterone trial demonstrated that women at high risk for preterm birth who were treated with progesterone were significantly less likely to deliver preterm than those treated with placebo. In that trial, women with a previous preterm birth were treated with weekly injections of 250 mg of 17-alpha-hydroxyprogesterone caproate or placebo from 17 to 20 weeks until 36 weeks or delivery. They reported that 111/306 (36.3%) of women treated with progesterone delivered at less that 37 weeks compared with 84/153 (54.9%) treated with placebo (relative risk [RR] 0.66; 95% confidence interval [CI] 0.54 to 0.81). Significantly fewer women treated with progesterone also delivered at <35 and <32 weeks. Several subsequent studies have shown that progesterone therapy reduces the risk of preterm birth in women at high risk for preterm birth. A meta-analysis concluded that progestational therapy reduced the risk of preterm birth and low birth-weight (LBW) infants. The authors concluded that with progesterone therapy, there was a reduction in the risk of preterm birth less than 37 weeks (six studies; 988 participants; RR 0.65; 95% CI 0.54 to 0.79) and preterm birth less than 34 weeks (one study; 142 participants; RR 0.15; 95% CI 0.04 to 0.64). Infants born to mothers administered progesterone were less likely to have birth weight less than 2,500 grams (four studies; 763 infants; RR 0.63; 95% CI 0.49 to 0.81) or intraventricular hemorrhage (one study; 458 infants; RR 0.25; 95% CI 0.08 to 0.82).
As of this writing, the optimal route and dose of progesterone have not been established. Published studies have used intramuscular injections of 17-alpha-hydroxyprogesterone caproate, progesterone suppositories, oral progesterone, and intramuscular progesterone tablets. The Food and Drug Administration (FDA) has not approved any progesterone preparation for the prevention of preterm birth, and the injectable formulations must be compounded prior to use. Compounded formulations are
not overseen by the FDA, and accuracy of dosing and sterility are in the hands of the compounding pharmacy.
not overseen by the FDA, and accuracy of dosing and sterility are in the hands of the compounding pharmacy.
Oxytocin
It is well known that oxytocin produces uterine activity when administered to pregnant women. The role of endogenous oxytocin as an initiator of term or preterm labor is less well defined. Some reasons to suspect that oxytocin is a universal initiator of labor are its ability to induce labor when given exogenously and the increase in blood levels that accompanies labor in most species. Because of the pulsatile manner of oxytocin release and the difficulty in measuring the hormone, its precise role in humans has been difficult to ascertain. Compared with nonlaboring patients, oxytocin levels appear to be significantly increased during the first stage of labor and increase to a greater amount during the second stage of labor. Oxytocin levels are higher in umbilical artery blood than in umbilical vein or maternal blood. This finding suggests that the fetus is a source of oxytocin production and release during labor. It is clear that the uterus becomes more sensitive to oxytocin in the days preceding labor. The number of myometrial cell membrane oxytocin receptors greatly increases as pregnancy advances, with a further increase during labor itself. In humans as well as in other species, the concentration of oxytocin receptors is a major reason for increased contractility of the uterus. The increase in oxytocin receptors is the result of increased estrogen levels.
Prostaglandins
Another important part of the parturition model is the synthesis and release of prostaglandins E2 and F2. This is supported by an increase in prostaglandins or metabolites in the amniotic fluid, endometrium, decidua, myometrium, and blood at the time of labor; the administration of prostaglandins inducing labor; and inhibitors to prostaglandin synthesis delaying labor. It is likely that the prostaglandins have a role in parturition originating from the decidua and myometrium. Oxytocin has the ability to stimulate prostaglandin release through the decidual receptors. In addition, infection of the membranes can release prostaglandins and may be an initiating factor in many cases of preterm labor.
Bacterial by-products may be directly responsible for the stimulation of prostaglandin release in the following ways. Bacterial phospholipase releases the precursor arachidonic acid from the amnion, leading to increased prostaglandin synthesis. Gram-negative organisms also may be able to produce prostaglandins through endotoxin stimulation of the decidua or membranes. Gram-positive organisms also may have prostaglandin-stimulating abilities through peptidoglycans. Phospholipase A2 is contained within the lysosome of the fetal membranes. As phospholipase A2 is released from the lysosome, prostaglandin may be synthesized, resulting in uterine contractions.
Cytokines
Cytokines are proteins secreted by the immune system in response to infection. There is recent interest in the role of cytokines and growth factors (e.g., epidermal growth factor, insulinlike growth factors 1 and 2) as potential initiators of labor. The cytokines interleukin 1 (IL-1), IL-6, and tumor necrosis factor (TNF) stimulate the amnion and decidua to produce prostaglandins and increase at time of labor, while transforming growth factor-β (TGF-β) inhibits prostaglandin production by other cytokines and may have antiprogestin properties. Finally, several different cytokines have been found in the amniotic fluid of patients with preterm labor.
Other Factors
Endothelins are potent vasoconstrictors in the sarafotoxinlike family. Some isoforms of endothelins are potent uterotonics. Although endothelin does not appear to increase at time of labor, uterine sensitivity and endothelin-receptor numbers do increase in the pregnant uterus. There is some decrease of endothelin-1 in the amniotic fluid of patients in labor, but this may be a consequence rather than an initiator of labor. Nitric oxide, produced from l-arginine by the enzyme nitric oxide synthase (NOS), mediates relaxation of vascular smooth muscle. It has been shown in various animal tissues, including human, that the NOS enzyme is decreased in myometrial tissue at term. Thus, nitric oxide may have a role in maintaining a quiescent uterus.
It can be hypothesized that parturition is a development of an estrogen environment. This estrogen environment promotes changes in the maternal pituitary with increased oxytocin synthesis and release. Estrogen may also be acting directly on the placenta and cervix. As the antiestrogen progesterone level decreases, estrogen can act to increase oxytocin receptors, prostaglandin production, and gap junction number and size. As the cervix ripens, the underlying membranes and decidua become exposed to the vaginal bacteria, triggering an inflammatory response with release of cytokines and prostaglandins. At this point, the paracrine events take dominance over the endocrine effects. Some conditions, such as infection, can overwhelm the endocrine phase of parturition.
Infection as a Cause of Preterm Birth
Preterm birth has been linked with symptomatic nongenital infections such as acute pyelonephritis and pneumonia. A large body of evidence suggests that subclinical infection
may be an important cause of premature labor, especially labors resulting in very early delivery.
may be an important cause of premature labor, especially labors resulting in very early delivery.
The hypothesis linking subclinical infection and premature birth may be summarized as follows. Microbes or their products such as endotoxin enter the uterine cavity during pregnancy, most commonly ascending from the lower genital tract. Blood-borne infection from a nongenital focus occurs less commonly. Microbes or their products then interact, most likely with the decidua or possibly with the membranes, producing prostaglandins or directly leading to uterine muscle contraction. This interaction is most likely mediated through a cytokine cascade. As a result, there is cervical dilation, entry of more microbes into the uterus, and continuation of “the vicious cycle” resulting in premature birth.
The first piece of evidence linking subclinical infection to preterm birth is that the prevalence of histologic chorioamnionitis is increased among preterm births. In membranes from preterm deliveries, there is a consistent and very strong association between positive membrane cultures and the likelihood of membrane infiltration. For example, when the birth weight is greater than 3,000 g, the percentage of placentae showing histologic chorioamnionitis is less than 20%; when the birth weight is below 1,500 g, the percentage is 60% to 70%. Most cases of histologic chorioamnionitis are caused by infection.
TABLE 11.1 Prenatal Infections as a Cause of Preterm Birth: Association and Treatment Recommendations | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Second, clinically recognized infections are increased in mothers and neonates after preterm birth. Sepsis and meningitis are increased 3- to 10-fold in preterm infants. Less widely recognized is the increase in maternal infection after preterm birth. These observations suggest that subclinical infection underlies preterm birth and that the infection became clinically evident during or shortly after birth.
Third, there are associations of preterm birth with various maternal lower genital infections or microbes (Table 11.1). Although Ureaplasma urealyticum in the lower genital tract had been associated with LBW infants in earlier studies, a large National Institutes of Health (NIH) study reported no associations of U. urealyticum in the vagina with any adverse pregnancy outcome (preterm birth, PPROM, LBW, or birth weight <1,500 g). Interestingly, then, U. urealyticum in the lower genital tract is not associated with LBW/preterm pregnancies, even though this organism is one of the most common isolates from the amniotic fluid of women in preterm labor. Lower genital infection with
Chlamydia trachomatis has also not been consistently associated with adverse pregnancy outcome. However, women with active chlamydial infection and with a positive serum antichlamydial immunoglobulin M (IgM) have an increased risk of preterm delivery. Although a consistent association has not been observed between maternal group B streptococci (GBS) colonization and premature birth in several small studies, a large investigation of approximately 13,000 women showed that pregnant women with heavy GBS colonization had a small but significant increase in risk for LBW (odds ratio [OR] 1.2; 95% CI 1.01 to 1.50). There were no significant increases in other adverse outcomes, including preterm birth, among heavily colonized women. Women with light colonization were not at an increased risk for any adverse outcomes. There is increasing evidence of an association between Trichomonas vaginalis and premature birth. Although small, earlier studies had conflicting results, the large Vaginal Infections and Prematurity Study found that the presence of T. vaginalis in the vagina at midpregnancy was significantly associated with preterm LBW (7.1% of women with T. vaginalis vs. 4.5% without T. vaginalis; OR 1.6; 95% CI 1.3 to 1.9). The MFMU Network bacterial vaginosis/T. vaginalis trial showed an association between carriage of T. vaginalis and preterm birth. Considerable data have linked lower genital tract anaerobes with preterm labor. Further, bacterial vaginosis, in which there is a predominance of anaerobes, has been consistently associated with approximately a two- to threefold increase in spontaneous preterm delivery. Among other infections, untreated pyelonephritis has been associated with a risk of preterm delivery of approximately 30%, and asymptomatic bacteriuria is associated with a 60% higher rate of LBW (95% CI 1.4 to 1.9) and a 90% higher rate of preterm delivery (95% CI 1.3 to 2.9).
Chlamydia trachomatis has also not been consistently associated with adverse pregnancy outcome. However, women with active chlamydial infection and with a positive serum antichlamydial immunoglobulin M (IgM) have an increased risk of preterm delivery. Although a consistent association has not been observed between maternal group B streptococci (GBS) colonization and premature birth in several small studies, a large investigation of approximately 13,000 women showed that pregnant women with heavy GBS colonization had a small but significant increase in risk for LBW (odds ratio [OR] 1.2; 95% CI 1.01 to 1.50). There were no significant increases in other adverse outcomes, including preterm birth, among heavily colonized women. Women with light colonization were not at an increased risk for any adverse outcomes. There is increasing evidence of an association between Trichomonas vaginalis and premature birth. Although small, earlier studies had conflicting results, the large Vaginal Infections and Prematurity Study found that the presence of T. vaginalis in the vagina at midpregnancy was significantly associated with preterm LBW (7.1% of women with T. vaginalis vs. 4.5% without T. vaginalis; OR 1.6; 95% CI 1.3 to 1.9). The MFMU Network bacterial vaginosis/T. vaginalis trial showed an association between carriage of T. vaginalis and preterm birth. Considerable data have linked lower genital tract anaerobes with preterm labor. Further, bacterial vaginosis, in which there is a predominance of anaerobes, has been consistently associated with approximately a two- to threefold increase in spontaneous preterm delivery. Among other infections, untreated pyelonephritis has been associated with a risk of preterm delivery of approximately 30%, and asymptomatic bacteriuria is associated with a 60% higher rate of LBW (95% CI 1.4 to 1.9) and a 90% higher rate of preterm delivery (95% CI 1.3 to 2.9).
Fourth, positive cultures of the amniotic fluid/membranes/decidua are found in some patients in premature labor. The range of positive amniotic fluid cultures obtained by amniocentesis from asymptomatic women in premature labor is 3% to 24%. When more sensitive testing for detection of bacteria (polymerase chain reaction) is carried out in amniotic fluid from women in preterm labor, bacteria are detected in 30% to 50%. The most likely route of upper genital tract infection in preterm labor is an ascending path through the vagina and cervix. Similarities in organisms isolated from the amniotic fluid and the lower genital tract support this pathogenic route. It is also possible that bacteria may enter the uterine cavity hematogenously through spread via the placenta, by contamination at the time of instrumentation such as during amniocentesis or chorionic villus sampling, or even by spread from the abdominal cavity via the fallopian tubes. Other sources of organisms for hematogenous spread include bacteremia from periodontal disease or procedures. Among women in spontaneous preterm labor with intact membranes, genital mycoplasmas, anaerobic organisms, and Gardnerella vaginalis (the so-called bacterial vaginosis organisms) are the organisms most commonly found in the amniotic fluid. Sexually transmitted organisms such as Neisseria gonorrhoeae and C. trachomatis are rarely found in the amniotic fluid, and GBS and Escherichia coli are found occasionally. Patients in preterm labor at early gestational ages have the highest likelihood of having a positive culture of the amniotic fluid. It may be speculated that intrauterine infection occurs early in pregnancy (or even has preceded the pregnancy) and may remain without clinical detection for months.
Fifth, biochemical “markers” of infection are often present among women in premature labor. In infection-induced premature labor, the primary site of infection is probably not the amniotic fluid but the decidua or membranes. More sensitive markers of infection potentially include amniotic fluid glucose concentrations, serum white blood cell counts, C-reactive protein, and amniotic or serum cytokines. Unfortunately, relatively few are clinically useful. Among patients in preterm labor, a low amniotic fluid glucose (<14 mg/dL) correlates well with the likelihood of a positive culture. Among the cytokines, an elevated amniotic fluid IL-6 level is probably the most sensitive marker for infection but is not yet widely available for clinical use.
Sixth, bacteria or their products induce preterm birth in animal models. Animal models have provided direct evidence that infection triggers preterm birth in the rabbit, monkey, and mouse.
The evidence linking infection to preterm birth has led to many trials of antibiotic therapy to prevent preterm birth. Antibiotic treatment trials may be classified as one of four designs:
Those conducted prenatally in patients at high risk for preterm delivery
Those directed toward a specific organism or condition
Those conducted in women in preterm labor with intact membranes, as adjuncts to tocolytic therapy
Those conducted in women with PPROM.
Chapter 12 discusses antibiotics in PPROM. Table 11.2 summarizes current practices for use of antibiotics to prevent preterm birth. The discordant results in antibiotic trials raise the question as to why antibiotics have not consistently prevented preterm birth or neonatal morbidity associated with preterm birth. One explanation is that infection is simply not a significant cause of preterm labor, but this seems unlikely in view of all the other evidence. Another explanation is that studies have had too low a power. However, large meta-analyses, the MFMU Network trials, and the ORACLE trial appear to exclude this possibility. Further, because preterm labor has multiple causes, a true effect of antibiotics may be diluted by those cases of preterm labor not caused by infection. It may also be that only a subset of pregnant women (e.g., perhaps genetically predisposed women) with high cytokine response are at risk for preterm labor after subclinical infection. Another explanation is that the antibiotics studied in most
of the trials were simply the wrong ones (e.g., not including antibiotics with better anaerobic activity), the antibiotics were given too late, or the antibiotic dose or timing were incorrect. Because infection is more likely to cause very early preterm birth (<32 weeks), trials focusing on women at later gestational ages may not show an effect. For example, the ORACLE I trial enrolled women up to 37 weeks gestation, and only 10% delivered at less than 32 weeks. It has also been speculated that bacterial lysis as a result of antibiotic therapy may lead to increased exposure to lipopolysaccharide and thus enhance preterm labor. Finally, it is possible that changes in the vaginal flora during pregnancy are responsible for preterm labor. Early screening and treatment may not identify women who are at risk. Antibiotic therapy may actually increase the risk of preterm birth by changing the vaginal flora. The MFMU bacterial vaginosis/T. vaginalis trial found that women with T. vaginalis who were treated with metronidazole were more likely to deliver preterm than those treated with placebo. The PREMET trial also found that women with a positive fetal fibronectin were more likely to deliver preterm if they were treated with metronidazole than placebo. It is possible that metronidazole therapy changes the vaginal flora in women who do not have bacterial vaginosis in such a way as to increase the risk of preterm birth.
of the trials were simply the wrong ones (e.g., not including antibiotics with better anaerobic activity), the antibiotics were given too late, or the antibiotic dose or timing were incorrect. Because infection is more likely to cause very early preterm birth (<32 weeks), trials focusing on women at later gestational ages may not show an effect. For example, the ORACLE I trial enrolled women up to 37 weeks gestation, and only 10% delivered at less than 32 weeks. It has also been speculated that bacterial lysis as a result of antibiotic therapy may lead to increased exposure to lipopolysaccharide and thus enhance preterm labor. Finally, it is possible that changes in the vaginal flora during pregnancy are responsible for preterm labor. Early screening and treatment may not identify women who are at risk. Antibiotic therapy may actually increase the risk of preterm birth by changing the vaginal flora. The MFMU bacterial vaginosis/T. vaginalis trial found that women with T. vaginalis who were treated with metronidazole were more likely to deliver preterm than those treated with placebo. The PREMET trial also found that women with a positive fetal fibronectin were more likely to deliver preterm if they were treated with metronidazole than placebo. It is possible that metronidazole therapy changes the vaginal flora in women who do not have bacterial vaginosis in such a way as to increase the risk of preterm birth.
TABLE 11.2 Use of Antibiotics to Prevent Preterm Birth in Women with Preterm Labor and Premature Rupture of the Membranes | |||
|---|---|---|---|
|
Epidemiology of Preterm Labor
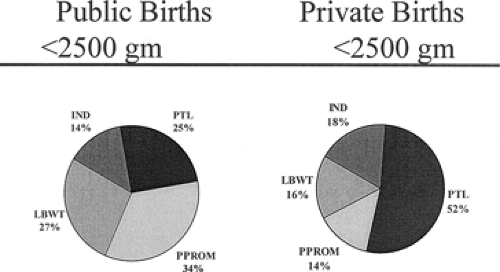
In 2004, 12.5% of women in the United States delivered preterm. The vast majority of preterm deliveries are a result of preterm labor (50%), premature rupture of the membranes (PROM) (33%), or cervical incompetence. The contributions of preterm labor and PROM to preterm deliveries vary depending on a number of factors, including socioeconomic status (Fig. 11.2). In a large study from North Carolina, Meis and colleagues found that PPROM (34%) was the most common reason for delivery of less than 2,500 g infants in women who were receiving public assistance. In contrast, in women who had private insurance, the most common reason for early delivery was preterm labor (52%). Indicated preterm deliveries accounted for 14% and 18% of preterm deliveries, respectively.
Several major and minor risk factors are associated with development of preterm labor and PROM (Tables 11.3, 11.4). One of the most obvious and important risk factors for prematurity is a prior history of preterm delivery. To better quantify this relationship, Mercer and associates performed a subgroup analysis of data collected during a large population-based observational study evaluating risk factors for preterm delivery. In this study, gravid women with any prior spontaneous preterm birth had a 2.5-fold increased risk of spontaneous preterm delivery in the current pregnancy. This risk increased to 10.6-fold if the spontaneous preterm birth occurred prior to 28 weeks gestation. Interestingly, women with a history of loss between 13 and 22 weeks gestation had rates of prematurity that were similar to women who did not have this history (10.1% vs. 8.8%; P =.69).
Another major risk factor for preterm labor and birth is multiple gestation. The rate of multiple gestations has increased dramatically over the past 15 years. The increase in twins and higher-order multiples is largely a reflection of
increased use of ovulation induction and assisted reproductive technologies. Fifty percent of twins deliver prematurely, with a mean gestational age at delivery of approximately 35 weeks. As expected, the percent of preterm deliveries increases in proportion to the number of fetuses. Triplets and quadruplets deliver on average at 32 weeks and 30 weeks, respectively. Until researchers develop techniques to perform artificial reproductive technologies that minimize the risk of having high-order multiples, then these women will continue to be at significant risk for delivering prematurely and suffering the consequences of preterm birth.
increased use of ovulation induction and assisted reproductive technologies. Fifty percent of twins deliver prematurely, with a mean gestational age at delivery of approximately 35 weeks. As expected, the percent of preterm deliveries increases in proportion to the number of fetuses. Triplets and quadruplets deliver on average at 32 weeks and 30 weeks, respectively. Until researchers develop techniques to perform artificial reproductive technologies that minimize the risk of having high-order multiples, then these women will continue to be at significant risk for delivering prematurely and suffering the consequences of preterm birth.
TABLE 11.3 Major Preterm Labor Risk Factors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 11.4 Minor Preterm Labor Risk Factors | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Blacks are 1.6 to 2.5 times more likely to deliver prematurely than white women of similar age and socioeconomic status. Although blacks have higher rates of prematurity, the rates of neonatal morbidity are lower in black neonates when compared with whites born at similar gestational ages. This suggests that the gestational period may be shorter in black women. Low socioeconomic status is also strongly associated with prematurity. It is not clear whether this is related to environment, genetic predisposition, infection, or access to medical care.
Table 11.4 also lists a number of “minor” risk factors for preterm labor and delivery. Several of these will be discussed in more detail later in this chapter. In general, the minor risk factors can be broken into two categories: those that are potentially modifiable and those that are not. Many of the minor risk factors are common in pregnancy. Individually, their contribution to prematurity is small; however, the risk is compounded by the addition of other risk factors. The impact of work on preterm birth remains controversial. Prolonged, physically demanding work does appear to independently increase the risk of prematurity and is potentially modifiable.
Prediction of Women at Risk for Preterm Labor
Over the past 2 decades, many researchers have focused on identification of women who are at risk for preterm delivery. Theoretically, identification of asymptomatic women at risk for preterm delivery would allow obstetricians to effectively intervene to prevent preterm delivery or to decrease neonatal morbidity and mortality in preterm neonates. In an American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin titled Assessment of Risk Factors for Preterm Birth, the authors wrote “the ability to predict whether a women is at risk of preterm delivery has value only if an intervention is available that is likely to improve the outcome.” It is believed that identification of women at risk for preterm birth will be beneficial if it allows women to:
receive a complete course of antenatal corticosteroids prior to delivery
if necessary, receive tocolytic agents to maximize the probability that antenatal corticosteroids will be given
be transported to a level III perinatal center.
Another potential benefit of screening is to identify women at low risk for preterm delivery and thereby avoid administration of potentially dangerous medications or therapies to these women.
Table 11.5 is a review of “ideal” criteria for a screening test. An ideal screening test should have high sensitivity and positive predictive value as well as high specificity and high negative predictive value. Most screening tests do not meet these requirements and trade off sensitivity for specificity. Depending on the clinical scenario where screening tests are used and the consequences of treatment or no treatment, one must decide which test characteristic to stress. For example, one could argue that given the high morbidity associated with preterm birth, the ideal screening test should have a high sensitivity to allow treatment of the majority of women “at risk” and accept a lower specificity rate. On the other hand, one could argue, as the ACOG did, that avoidance of treatment with potentially hazardous drugs is beneficial in women with symptoms who are at “low risk” for delivery, thus stressing the importance of the test’s specificity and negative predictive value. The following will review available screening tests.
TABLE 11.5 Criteria for Screening Tests | |
|---|---|
|
Risk Scoring Systems
Risk scoring systems were promoted heavily in the 1980s to identify women at risk for preterm delivery. The risk scoring systems weigh major and minor risk factors for preterm birth as well as current pregnancy complications (Tables 11.3, 11.4). The scoring systems work best in multiparous patients and worst in privately insured nulliparas with singleton gestations. Overall, the sensitivity of the screening tool ranges from 3% to 30% and the positive predictive values from 0% to 20%, depending on the population studied. While easy to use to identify women who may have modifiable risk factors for preterm delivery, the scoring systems do not reliably identify women at risk. They should not be used alone to institute interventions that may or may not be warranted.
Contraction Monitoring
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree