Poverty, Homelessness, and Social Disorganization
Barry S. Zuckerman and Megan Sandel
POVERTY AND CHILD DEVELOPMENT
Children who live in poor families face pervasive challenges to their health and development. These challenges result in increased rates of illness, developmental delay, behavioral problems, school failure, and social dysfunction. Poverty, adverse exposures, and unmet basic needs amplify the impact of biological vulnerabilities on the child. However, as with other threats to health and development, poverty’s effects can be offset by individual, family, community, and professional buffering factors that offer both protection and support.
THE EPIDEMIOLOGY OF POVERTY
The official poverty level is based on the estimated cost of food multiplied by 3; this is based on the assumption that food accounts for one third of a family’s income after taxes, which for a family of four is $20,650 or less. The level is adjusted for size of household but not for regional variations in cost of living or actual expenditures and income.1 Estimates from the National Center for Children in Poverty at Columbia estimate that 13 million children lived in poverty in 2006, an increase of 1.2 million children just since 2000. Contrary to stereotypes, almost two thirds of poor children have parents who work, and over one half of poor children live in the suburbs or in rural areas. There are enormous racial disparities in poverty: a greater proportion of African American and Latino children live in poverty (ie, 33% of all African American children and 27% of all Hispanic children live in poverty, versus 10% of white children), but in absolute real numbers there are more poor white than poor African American or Latino children. However, families whose incomes are even twice the federal poverty level have trouble making ends meet. Twenty-eight million children live in such “low-income” families.2
THE DIMENSIONS OF POVERTY
The concept of “poverty” encompasses insufficient income and the range of conditions that poor families endure.3,4 Poverty’s impact varies, depending on whether it is normative within a given society; urban or rural; brief, intermittent, or chronic; relative; or at a level that compromises physical survival. Income inequality is now thought to be a more sensitive indicator of health problems than mean income. This may be mediated through social marginalization, the end product of the experience of social inequalities such as poor schools, poor health services, and poor homes. Some US families may have members who are disabled by mental illness, alcoholism, or other chronic conditions, and local economic stagnation or racism may limit their access to educational opportunities, quality health care, and better jobs, leading to multigenerational poverty.
Families in such variable settings experience different social environments and have different expectations for themselves and their children. For example, families who fall under the poverty level for shorter periods because of transient unemployment may have more economic and psychological reserves with which to endure its effects than families who have been in poverty for several generations. Families living in urban poverty have increased exposure to lead, violence, household allergens, and airborne pollutants, while rural families typically have less access to the array of helping agencies that are available in cities.
RISK AND PROTECTIVE FACTORS IN POVERTY
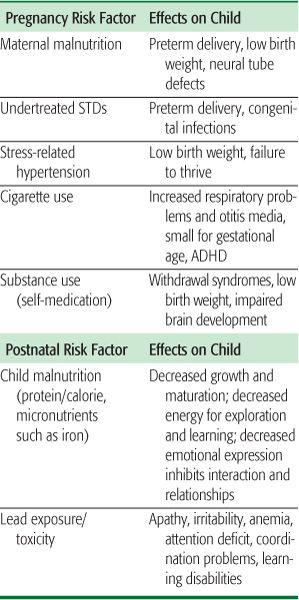
Many of the biomedical risks of poverty directly affect general health, but in children, they more specifically affect the developing brain and are linked to behavioral and developmental problems. Factors that affect poor women of childbearing age also affect pregnancy outcomes (ie, undertreated vaginal infections are associated with preterm delivery; poor nutritional status is associated with multiple perinatal risks) and child health outcomes not limited to the prenatal period. The consequences of some of these risk factors for children are summarized in Table 100-1. For example, a child who is born prematurely and has iron deficiency anemia and lead poisoning as a result of his family not being able to afford a decent home is at high risk for early language delay, later learning problems, and school failure. Such a child is less likely to succeed in school or at work unless these factors are recognized and treatment, early intervention, and support are provided.
Poverty also presents psychosocial challenges to child development. While these stressors may be conferred by poverty, coping strategies can serve as buffers that enable poor families and children to surmount such challenges. Poor families can successfully overcome these stressors by developing strong and flexible networks among extended family and friends, and among community resources such as churches and neighborhood associations. The ability to form such relationships (social capital) is critical to the survival of families in poverty.
THE IMPACT OF CHRONIC POVERTY
Prolonged poverty fosters a number of coping styles that are maladaptive in other settings. For example, children who are raised in poorer families may be socialized for early independence and toughness, traits that are adaptive to their neighborhood, if not for school. Poor children of school age are less likely to participate in extracurricular activities, and missing these activities is associated with antisocial behavior and lower scores on standardized tests. Furthermore, living amid a culture that has much higher material expectations, chronically poor families endure a sense of persistent helplessness and hopelessness, which can grow into depression and rage that are as devastating as the lack of access to goods or services.
However, families living in poverty can develop the kinds of coping strengths that are often seen in intact preindustrial cultures. These include individual resilience, resourcefulness, and endurance; flexible extended family networks that provide childcare, a sense of belonging, and help with practical needs in times of crisis; and churches and other religious institutions that further extend the family network.5
THE EFFECTS OF POVERTY ON CHILDREN AND FAMILIES
The effects of poverty influence parents’ behavior and create many pathways for poor child health. Parents in poor families may read less to their young children, which contributes to lack of school readiness. Low-income or poverty status can also lead to parents having to make budget trade-offs, such as deciding whether to pay for food or heating their house. Research shows increased hunger and malnutrition in the winter compared to the summer, a phenomena called “heat or eat.” Also, children from families that are on waiting lists for housing subsidies compared to children who received such subsidies are more likely to have nutrition problems. While there are federal subsidies for heating homes, they have never met the full needs of the poor and have decreased in real dollars since being implemented in 1981. One study showed that children who were eligible but who did not receive this subsidy were 30% more likely to be admitted to the hospital and 20% more likely to be at risk for growth problems compared to children receiving this subsidy.6
Table 100-1. The Impact of Biomedical Factors Associated with Poverty
The high, persistent levels of stress that are associated with poverty undermine parents’ physical and mental health, leading to high rates of stress-related medical conditions (such as hypertension and asthma) and psychological problems (such as depression, anxiety, troubled relationships, and substance abuse).7 Also, parental stress may interfere with daily interactions that are needed to establish trust, safety, a sense of cause and effect, and the ability to express curiosity and contributes to abuse and neglect.8 Lastly, the ability to climb out of poverty can be limited by joblessness, particularly of fathers, which is linked to domestic violence and child abuse. In addition, many institutions that are meant to serve poor families (eg, welfare and public housing agencies) impose further stress through demeaning and time-consuming hurdles. These parental stressors can impact upon their ability to provide sensitive and nurturant caregiving that optimizes brain development, and this may have a lifelong impact as discussed in Chapter 81.
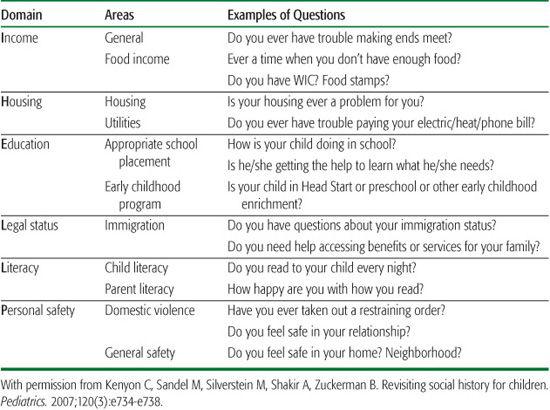
Table 100-2. Examples of Potential Social History Questions: “I HELLP” to Address Basic Needs
HOUSING: A CASE IN POINT
Stable, safe housing is necessary for children’s health and development. It has been estimated that 100,000 children in the United States are homeless every night and that many more sleep on couches and floors in the homes of relatives or friends. In addition to homelessness, marginal housing has negative biomedical and psychosocial effects, including injuries, lead poisoning, asthma, stunted growth, developmental delays, and early onset of mental health problems.
Homeless children cannot count on a quiet place to sleep or a safe place to play and learn. They do not have the security of regular routines, and their parents are often stressed and preoccupied by the struggle to survive. They may spend their days on the streets and their nights in cars or doorways, or they may live in homeless shelters. Such shelters often are noisy and dangerous, leaving children tired and hypervigilant when and if they reach school.
THE ROLE OF HEALTH CARE PROVIDERS FOR POOR CHILDREN
Although adequate health care can buffer children from some of the adverse consequences of poverty, broad-based social policies that can provide for basic needs (eg, food, shelter, income support) are what have the greatest potential to attenuate other negative impacts. Gaps in the implementation of available programs and policies are well documented. In addition to providing preventive and acute health care and supportive relationships, health care providers can screen and advocate for unmet basic needs.
Table 100-2 provides an outline of social history screening questions that focus on basic needs and factors that influence health and are amenable to direct intervention.9 While social workers, case managers, or other members of the health care team help families with these unmet basic needs, lawyers have been added to the pediatric health care team in a growing number of health settings. These professionals can remove barriers to the health care team’s efforts. In addition, lawyers have the knowledge and skills to address many of the social determinants of poor health associated with poverty, since poor people have been shown to have three to four unmet legal needs. Disenfranchised families facing multiple crises generally cannot convince service agencies, landlords, or governments of their eligibility. But health care providers working with lawyers can be particularly effective voices for such families and their children, whether through individual advocacy or through policy-related research.5
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


