Postpartum
Highlighting the phases of the postpartum period
This chart summarizes the three phases of the postpartum period as identified by Reva Rubin.
| Phase | Maternal behavior and tasks |
|---|---|
| Taking in (1 to 2 days after delivery) |
|
| Taking hold (2 to 7 days after delivery) |
|
| Letting go (7 days after delivery) |
|
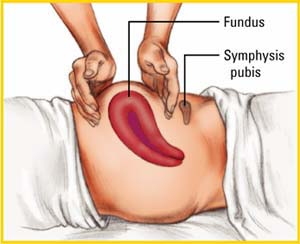
Palpating the fundus
A full-term pregnancy stretches the ligaments supporting the uterus, placing it at risk for inversion during palpation and massage. To guard against this, place one hand against the patient’s abdo-men at the symphysis pubis level, as shown at right. This steadies the fundus and prevents downward displacement. Then place the other hand at the top of the fundus, cupping it, as shown.
 |
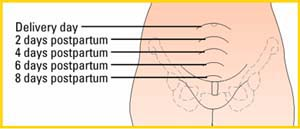
Uterine involution
After delivery, the uterus begins its descent back into the pelvic cavity. It continues to descend about 1 cm/day until it isn’t palpable above the symphysis at about 9 days after delivery.
 |
Assessing lochia flow
Character
Lochia typically is described as lochia rubra, serosa, or alba, depending on the color of the discharge. Lochia should always be present during the first 3 weeks postpartum. The patient who has had a cesarean birth may have a scant amount of lochia; however, lochia is never absent.
Amount
Although it varies, the amount can be compared to that of a menstrual flow. Saturating a perineal pad in less than 1 hour is considered excessive; the doctor should be notified. Expect women who are breast-feeding to have less lochia. Lochia flow also increases with activity—for example, when the patient gets out of bed the first few times (due to pooled lochia being released) or when the patient engages in strenuous exercise, such as lifting a heavy object or walking up stairs (due to an actual increase in amount).
Color
Depending on the postpartum day, lochia typically ranges from red to pinkish brown to creamy white or colorless. A sudden change in the color of lochia—for example, to bright red after having been pink—suggests new bleeding or retained placental fragments.
Odor
Lochia has an odor similar to that of menstrual flow. Foul or offensive odor suggests infection.
Consistency
Lochia should have minimal or small clots, if any. Evidence of large or numerous clots indicates poor uterine contraction, which requires intervention.
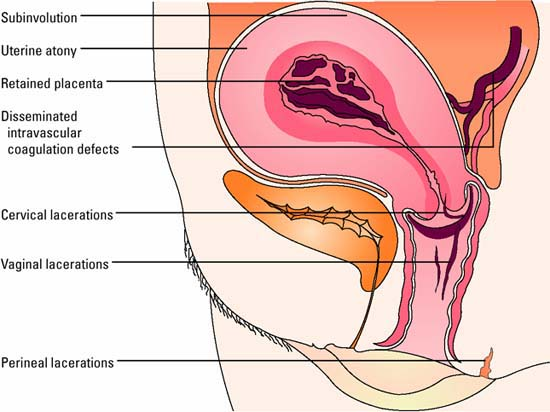
Common causes of postpartal hemorrhage
This illustration highlights the common causes of postpartal hemorrhage.
 |
Risks factors for developing postpartal hemorrhage
Cervical or uterine lacerations
Operative birth (episiotomy, forceps application)
Rapid birth
Inadequate blood coagulation
Fetal death
Disseminated intravascular coagulation
Placental problems
Placenta previa
Placenta accreta
Premature separation of the placenta
Retained placental fragments
Uterine distention
Multiple gestation
Hydramnios (excessive amniotic fluid)
Large fetus (> 9 pounds)
Uterine myomas (fibroid tumors)
Uterine incontractability
Deep anesthesia or analgesia
Previous history of postpartum hemorrhage
Secondary maternal illness such as anemia
Endometritis
Prolonged and difficult labor
Labor augmentation or initiation by oxytocin (Pitocin)
Possible chorioamnionitis
High parity
Maternal age > 30
Prolonged use of magnesium sulfate or other tocolytic drugs
Previous uterine surgery
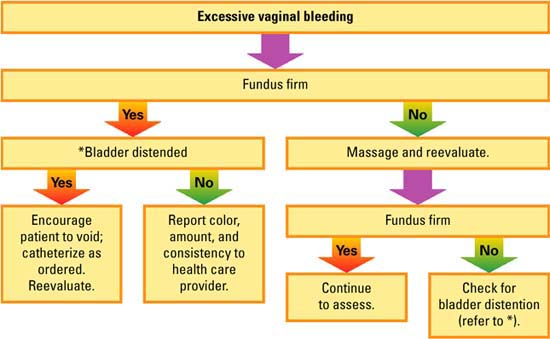
Assessing excessive vaginal bleeding
Use this flowchart to help guide your interventions when you determine that your patient has excessive vaginal bleeding.
 |
Assessing puerperal infection
Localized perineal infection
Pain
Elevated temperature
Edema
Redness, firmness, and tenderness at the site of the wound
Sensation of heat
Burning on urination
Discharge from the wound
Endometritis
Heavy, sometimes foul-smelling lochia
Tender, enlarged uterus
Backache
Severe uterine contractions persisting after childbirth
Parametritis (pelvic cellulitis)
Vaginal tenderness
Abdominal pain and tenderness (pain may become more intense as infection spreads)
Inflammation may remain localized, may lead to abscess formation, or may spread through the blood or lymphatic system
Septic pelvic thrombophlebitis
Caused by widespread inflammation
Severe, repeated chills and dramatic swings in body temp-erature
Lower abdominal or flank pain
Possible palpable tender mass over the affected area, usually developing near the second postpartum week
Peritonitis
Caused by widespread inflammation
Rigid, boardlike abdomen with guarding (commonly the first manifestation)
Elevated body temperature accompanied by tachycardia (heart rate greater than 140 beats/minute), weak pulse, hiccups, nausea, vomiting, and diarrhea
Constant and possibly excruciating abdominal pain
Comparing femoral and pelvic deep vein thrombosis (DVT)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


