Intrapartum
Types of spontaneous abortion
Spontaneous abortions occur without medical intervention and in various ways.
Complete abortion
The uterus passes all products of conception. Minimal bleeding usually accompanies complete abortion because the uterus contracts and compresses the maternal blood vessels that feed the placenta.
Habitual abortion
Spontaneous loss of three or more consecutive pregnancies constitutes habitual abortion.
Incomplete abortion
The uterus retains part or all of the placenta. Before 10 weeks’ gestation, the fetus and placenta are usually expelled together; after the 10th week, they’re expelled separately. Because part of the placenta may adhere to the uterine wall, bleeding continues. Hemorrhage is possible because the uterus doesn’t contract and seal the large vessels that feed the placenta.
Inevitable abortion
Membranes rupture and the cervix dilates. As labor continues, the uterus expels the products of conception.
Missed abortion
The uterus retains the products of conception for 2 months or more after the fetus has died. Uterine growth ceases; uterine size may even seem to decrease. Prolonged retention of the dead products of conception may cause coagulation defects such as disseminated intravascular coagulation.
Septic abortion
Infection accompanies abortion. This may occur with spontaneous abortion but usually results from a lapse in sterile technique during therapeutic abortion.
Threatened abortion
Bloody vaginal discharge occurs during the first half of pregnancy. About 20% of pregnant women have vaginal spotting or actual bleeding early in pregnancy. Of these, about 50% abort.
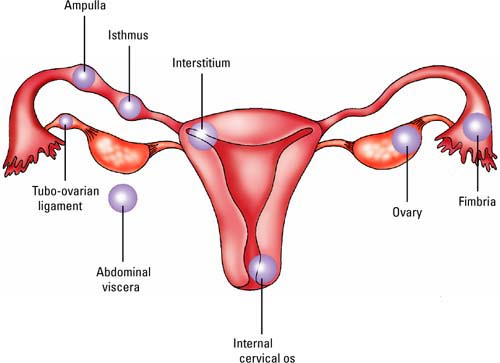
Sites of ectopic pregnancy
In most women with ectopic pregnancy, the ovum implants in the fallopian tube, either in the fimbria, ampulla, or isthmus. Other possible sites of implantation include the interstitium, tubo-ovarian ligament, ovary, abdominal viscera, and internal cervical os.
 |
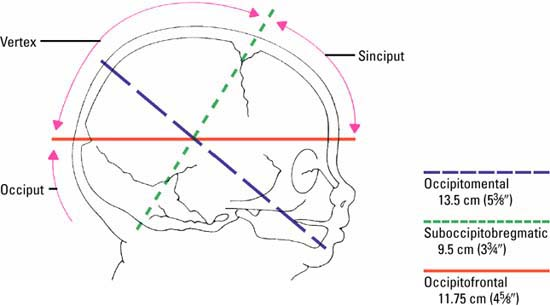
Head diameters at term
This illustration depicts three commonly used measurements of fetal head diameters. The measurements are averages for term neonates. Individual measurements vary with fetal size, attitude, and presentation.
 |
Distinguishing between true and false labor
| True labor | False labor |
|---|---|
|
|
Stages of labor
Stage 1
It begins at onset of true labor.
It lasts until complete dilation, which is about 6 to 18 hours in the primipara and 2 to 20 in the multipara.
It’s divided into the latent, active, and transitional phases.
Latent phase
Cervical dilation measures 0 to 3 cm.
Contractions are irregular, short, and last 20 to 40 seconds.
Phase lasts about 6 hours for a primipara and 4½ hours for a multipara.
Active phase
Cervical dilation measures 4 to 7 cm.
Contractions are 5 to 8 minutes apart and last 45 to 60 seconds.
Phase lasts about 3 hours for a primipara and 2 hours for a multipara.
Transitional phase
Cervical dilation measures 8 to 10 cm.
Contractions are 1 to 2 minutes apart and last 60 to 90 seconds.
At the end of this phase, the patient feels the urge to push.
Stage 2
It extends from complete dilation to delivery of the neonate.
It lasts from 1 to 3 hours for the primipara and 30 to 60 minutes for the multipara.
It occurs in seven cardinal movements.
It’s divided into the latent, active, and transitional phases.
Latent phase
It begins at onset of contractions and ends when rapid cervical dilation begins.
Phase lasts about 10 to 30 minutes.
Active phase
Cervical dilation rapidly moves from 4 to 7 cm.
Phase duration varies.
Transitional phase
Maximum dilation is 8 to 10 cm.
Average duration is 5 to 15 minutes.
Stage 3
It extends from the delivery of the neonate to delivery of the placenta.
It lasts from 5 to 30 minutes.
It’s divided into the placental separation and the placental expulsion phases.
Stage 4
It covers the time immediately after delivery of the placenta.
Typically, it’s the first hour after delivery.
It’s referred to as the recovery period.
Classifying fetal presentation
Fetal presentation may be broadly classified as cephalic, breech, shoulder, or compound. Cephalic presentations occur in almost all deliveries. Of the remaining three, breech deliveries are most common.
Cephalic
In the cephalic, or head-down, presentation, the fetus’ position may be classified by the presenting skull landmark: vertex, brow, sinciput, or mentum (chin).
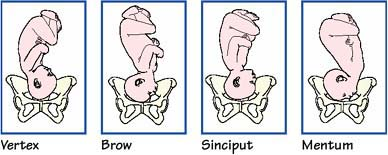 |
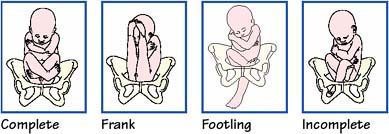
Breech
In the breech, or head-up, presentation, the fetus’ position may be classified as complete, where the knees and hips are flexed; frank, where the hips are flexed and knees remain straight; footling, where neither the thighs nor lower legs are flexed; and incomplete, where one or both hips remain extended and one or both feet or knees lie below the breech.
 |
Shoulder
Although a fetus may adopt one of several shoulder presentations, examination can’t differentiate among them; thus, all transverse lies are considered shoulder presentations.
 |
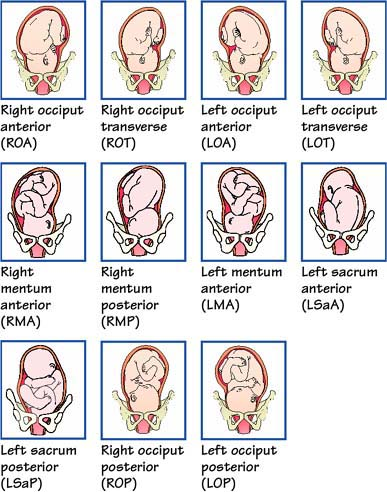
Fetal position abbreviations
These abbreviations, organized according to variations in presentation, are used when documenting fetal position.
Vertex presentation (occiput)
LOA, left occiput anterior
LOP, left occiput posterior
LOT, left occiput transverse
ROA, right occiput anterior
ROP, right occiput posterior
ROT, right occiput transverse
Breech presentation (sacrum)
LSaA, left sacrum anterior
LSaP, left sacrum posterior
LSaT, left sacrum transverse
RSaA, right sacrum anterior
RSaP, right sacrum posterior
RSaT, right sacrum transverse
Face presentation (mentum)
LMA, left mentum anterior
LMP, left mentum posterior
LMT, left mentum transverse
RMA, right mentum anterior
RMP, right mentum posterior
RMT, right mentum transverse
Shoulder presentation (acromion process)
LAA, left scapuloanterior
LAP, left scapuloposterior
RAA, right scapuloanterior
RAP, right scapuloposterior
Fetal attitude
Fetal attitude refers to the relationship of fetal body parts to one an-other. It denotes whether presenting parts are in flexion or extension.
Complete flexion
Most common
Neck is completely flexed, with the head tucked down to the chest and the chin touching the sternum
Arms are folded over the chest, with the elbows flexed
Lower legs are crossed and the thighs are drawn up onto the abdomen, with the calf of each leg pressed against the thigh of the opposite leg
Moderate flexion
Second most common
Commonly known as the military position because the head’s straightness makes the fetus appear to be “at attention”
Involves sinciput (forehead) presentation through the birth canal
Neck is slightly flexed
Head is held straight but the chin doesn’t touch the chest
Many fetuses assume this attitude early in labor but convert to a complete flexion (vertex presentation) as labor progresses
Birth usually isn’t difficult because the second smallest anteroposterior diameter of the skull is presented through the pelvis during delivery
Partial extension
Uncommon
Involves brow presentation through the birth canal
Neck is extended
Head is moved backward slightly so that the brow is the first part of the fetus to pass through the pelvis during delivery
Can cause a difficult delivery because the anteroposterior diameter of the skull may be equal to or larger than the opening in the pelvis
Complete extension
Rare; considered abnormal
Can result from various factors:
– oligohydramnios (less-than-normal amniotic fluid)
– neurologic abnormalities
– multiparity or a large abdo-men with decreased uterine tone
– nuchal cord with multiple coils around the neck
– fetal malformation (found in as many as 60% of cases)
Involves a face presentation through the birth canal
Head and neck of the fetus are hyperextended, with the occiput touching the upper back
Back is usually arched, increasing the degree of hyperextension
Usually requires cesarean birth
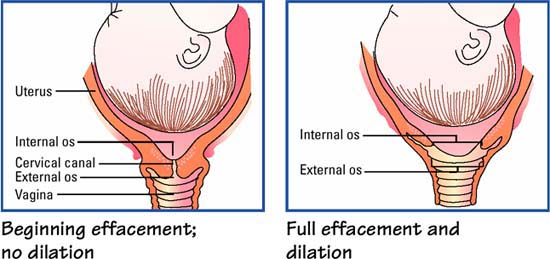
Cervical effacement and dilation
As labor advances, so do cervical effacement and dilation, which promote delivery. During effacement, the cervix shortens and its walls become thin, progressing from 0% effacement (palpable and thick) to 100% effacement (fully indistinct, or effaced, and paper thin). Full effacement obliterates the constrictive uterine neck to create a smooth, unobstructed passageway for the fetus.
At the same time, dilation occurs. This progressive widening of the cervical canal—from the upper internal cervical os to the lower external cervical os—advances from 0 to 10 cm. As the cervical canal opens, resistance decreases; this further eases fetal descent.
 |
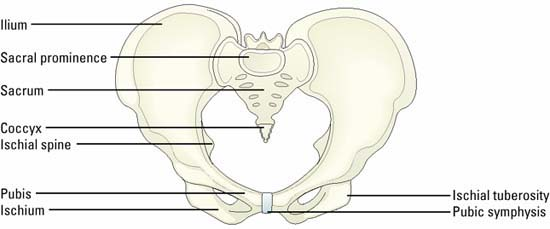
Assessing fetal engagement and station
During a cervical examination, you’ll assess the extent of the fetal presenting part into the pelvis. This is referred to as fetal engagement.
After you have determined fetal engagement, palpate the presenting part and grade the fetal station (where the presenting part lies in relation to the ischial spines of the maternal pelvis). If the presenting part isn’t fully engaged into the pelvis, you can’t assess station.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree