Neonatal
Medications for neonatal resuscitation
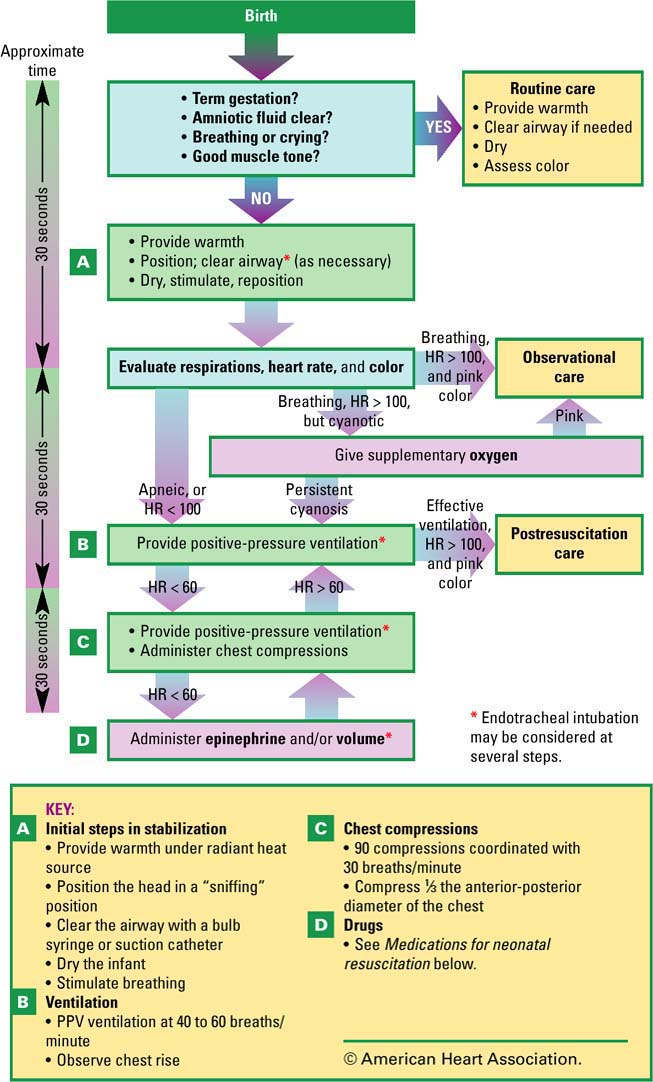
The American Heart Association and the American Academy of Pediatrics recommend you refer to this chart before giving medications for resuscitating neonates.
| Medication | Concentration to administer | Dosage and route | Rate and precautions |
|---|---|---|---|
| Epinephrine |
|
|
|
| Volume expanders |
|
|
|
Physiology of the neonate
| Body system | Physiology after birth |
|---|---|
| Cardiovascular |
|
| Respiratory |
|
| Renal |
|
| GI |
|
| Thermogenic |
|
| Immune |
|
| Hematopoietic |
|
| Neurologic |
|
| Hepatic |
|
| Integumentary |
|
| Musculoskeletal |
|
| Reproductive |
|
Neonatal assessment
Initial neonatal assessment
Ensure a proper airway via suctioning.
Administer oxygen as needed.
Dry the neonate under the warmer.
Keep the neonate’s head lower than his trunk to promote drainage of secretions.
Help determine the Apgar score.
Apply a cord clamp and monitor the neonate for abnormal bleeding from the cord.
Analyze the umbilical cord. (Two arteries and one vein should be apparent.)
Observe the neonate for voiding and meconium.
Assess the neonate for gross abnormalities and signs of suspected abnormalities.
Continue to assess the neonate by using the Apgar score criteria, even after the 5-minute score is received.
Obtain clear footprints and fingerprints.
Apply identification bands with matching numbers to the mother (one band) and neonate (two bands) before they leave the delivery room.
Promote bonding between the mother and neonate.
Review maternal prenatal and intrapartal data to determine factors that might impact neonatal well-being.
Ongoing assessment
Assess the neonate’s vital signs.
Measure and record blood pressure.
Measure and record the neonate’s size and weight.
Complete a gestational age assessment, if indicated.
Categorizing gestational age
Preterm neonate—Less than 37 weeks’ gestation
Term neonate—37 to 42 weeks’ gestation
Postterm neonate—Greater than or equal to 42 weeks’ gestation
Recording the Apgar score
Use this chart to determine the neonatal Apgar score after birth. For each category listed, assign a score of 0 to 2, as shown. A total score of 7 or higher indicates that the neonate is in good condition; 4 to 6, fair condition (the neonate may have moderate central nervous system depression, muscle flaccidity, cyanosis, and poor respirations); 0 to 3, danger (the neonate needs immediate resuscitation, as ordered). Each component should be assessed at 1, 5, 10, 15, and 20 minutes after delivery, as necessary.
| Sign | Apgar score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | ||
| Heart rate | Absent | Less than 100 beats/minute | More than 100 beats/minute | |
| Respiratory effort | Absent | Slow, irregular | Good crying | |
| Muscle tone | Flaccid | Some flexion and resistance to extension of extremities | Active motion | |
| Reflex irritability | No response | Grimace or weak cry | Vigorous cry | |
| Color | Pallor, cyanosis | Pink body, blue extremities | Completely pink | |
Normal neonatal vital signs
Respiration
30 to 50 breaths/minute
Temperature
Rectal: 96° to 99.5° F (35.6° to 37.5° C)
Axillary: 97.5° to 99° F (36.4° to 37.2° C)
Heart rate (apical)
110 to 160 beats/minute
Blood pressure
Systolic: 60 to 80 mm Hg
Diastolic: 40 to 50 mm Hg
Counting neonatal respirations
Observe abdominal excursions rather than chest excursions.
Auscultate the chest.
Place the stethoscope in front of the mouth and nares.
Average neonatal size and weight
Size
Average initial anthropometric ranges are:
head circumference—13″ to 14″ (33 to 35.5 cm)
chest circumference—12″ to 13″ (30.5 to 33 cm)
head to heel—18″ to 21″ (46 to 53 cm)
weight—2,500 to 4,000 g (5 lb, 8 oz to 8 lb, 13 oz).
Birth weight
Normal birth weight: 2,500 g (5 lb, 8 oz) or greater
Low birth weight: Between 1,500 g (3 lb, 5 oz) and 2,499 g
Very low birth weight: Between 1,000 g (2 lb, 3 oz) and 1,499 g
Extremely low birth weight: Less than 1,000 g
Preventing heat loss
Follow these steps to prevent heat loss in the neonate.
Conduction
Preheat the radiant warmer bed and linen.
Warm stethoscopes and other instruments before use.
Before weighing the neonate, pad the scale with a paper towel or a preweighed, warmed sheet.
Convection
Place the neonate’s bed out of a direct line with an open window, fan, or air-conditioning vent.
Evaporation
Dry the neonate immediately after delivery.
When bathing, expose only one body part at a time; wash each part thoroughly, and then dry it immediately.
Radiation
Keep the neonate and examining tables away from outside windows and air conditioners.
Neurologic assessment
Normal neonates display various reflexes. Abnormalities are indicated by absence, asymmetry, persistence, or weakness in these reflexes:
sucking—begins when a nipple is placed in the neonate’s mouth
Moro’s reflex—when the neo-nate is lifted above the bassinet and suddenly lowered, his arms and legs symmetrically extend and then abduct while his thumb and forefinger spread to form a “C”
rooting—when the neonate’s cheek is stroked, he turns his head in the direction of the stroke
tonic neck (fencing position)— when the neonate’s head is turned while he’s lying in a su-pine position, his extremities on the same side straighten and those on the opposite side flex
Babinski’s reflex—when the sole on the side of the neonate’s small toe is stroked, toes fan upward
grasping—when a finger is placed in each of the neonate’s hands, his fingers grasp tightly enough that he can be pulled to a sitting position
stepping—when the neonate is held upright with his feet touching a flat surface, he responds with dancing or stepping movements.
Common skin findings
The term neonate has beefy red skin for a few hours after birth before it turns its normal color. Other findings include:
acrocyanosis (caused by vasomotor instability, capillary stasis, and high hemoglobin level) for the first 24 hours
milia (clogged sebaceous glands) on the nose or chin
lanugo (fine, downy hair) after 20 weeks’ gestation on the entire body (except on palms and soles)
vernix caseosa (a white, cheesy protective coating of desquamated epithelial cells and sebum)
erythema toxicum neonatorum (a transient, maculopapular rash)
telangiectasia (flat, reddened vascular areas) on neck, eyelid, or lip
sudamina or miliaria (distended sweat glands) that cause minute vesicles on the skin surface, especially on the face
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree