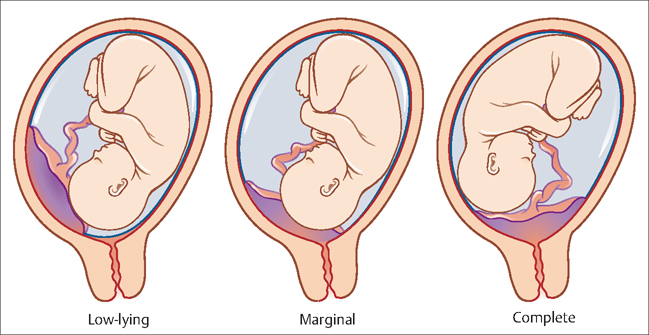
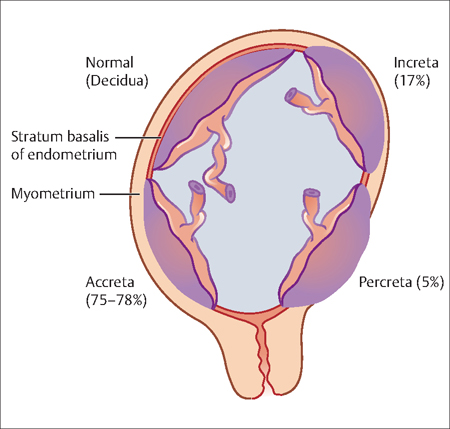
22 Postpartum Hemorrhage and Infection Gustavo Leguizamòn and Alberto Fernández Postpartum hemorrhage is excessive bleeding following the birth of a baby. It is one of the most life-threatening complications following birth. There are many types and causes of abnormal bleeding in a pregnant woman. This chapter discusses the many types of bleeding events that can occur in pregnancy, their frequency, their common symptoms, and the most effective approaches to management. Also briefy discussed in this chapter are measures needed to prevent the introduction of naturally occuring bacteria into the hemorrhage site and further complicating management of these serious conditions. Chapter 28 contains a more extensive discussion of the prevention and management of a wide vaiety of infections that can occur in pregnancy. Placental abruption (abruptio placentae): This term is used to describe the premature separation, either partial or total, of the placenta from the uterus during pregnancy or in labor. Placental abruption can be classifed as: Fig. 22.1 Classification scheme for placenta previa Placenta acreta: This refers to an abnormal attachment of the placenta to the uterine wall, secondary to the absence of the decidua basalis. When this abnormal attachment extends to or through the myometrium it is called placenta increta or placenta percreta, respectively. Placenta previa: This condition occurs when the placenta locates either over, or in close proximity to, the internal os. Three types have been traditionally recognized (Fig. 22.1). Puerperal endometritis: This term describes a polymicrobial infection caused by bacteria from the genital tract. Uterine atony: The lack of an effective contraction after the delivery of the placenta. It is the most common etiology of postpartum hemorrhage. Vasa previa: This term refers to the velamentous insertion of fetal vessels over the cervical os. The condition is a grave one, since vessel rupture is a frequent event with subsequent fetal exanguination. Identifying risk factors is of the outmost importance to enable prompt diagnosis of this condition. Few situations are as dangerous for the patient and stressful for the health care team as diagnosing an unsuspected placenta acreta during a cesarean section. The best approach to early detection of placenta acreta is to identify risk factors (see Etiology and Risk Factors below) and, if present, conduct an ultrasonographic evaluation of placental insertion. The loss of the normal hypoechoic limit between placenta and myometrium is indicative of a possible acreta. This condition is usually asymptomatic until membranes are ruptured and vessels start bleeding. Occasionally, it is diagnosed antenatally with Doppler ultrasonography. Intensive fetal monitoring and early admission as well as delivery should be considered. Symptoms usually manifest during the first 48 hours after delivery. The most frequent findings are: If diagnosis is not clear, conduct a vaginal exam to confirming pain on uterine palpation and an increase in temperature of the vaginal mucosa. Uterine atony is typically diagnosed after delivery when there is excessive bleeding and a large, relaxed uterus. The doctor may perform an examination to be certain that there are no tears of the cervix or the vagina, and that all fragments of placenta have been removed from the uterus. The diagnosis often is not made antepartum. Patients usually present with bleeding at the time of spontaneous or artificial rupture of membranes. However, bleeding can occur before the rupture of membranes. Vasa previa can also present with fetal bradycardia when the velamentous vessels are compressed by the presenting part. Most often, the fetus is already dead when the diagnosis is made due to massive blood loss. The prevalence of placental abruption depends on the population studied. It has been reported as ranging from 1 in 75 to 1 in 226 deliveries. Risk of recurrence is between 5% and 17% after one placental abruption. After two consecutive episodes, the recurrence risk is approximately 25%. Although a significant decrease in perinatal mortality has been observed in many populations, placental abruption is still of significant concern. There is a ninefold increase in intrauterine demise and fourfold increase in preterm delivery associated with this condition. This condition occurs with a frequency of approximately 1 in 500 deliveries. The overall incidence has been reported to be 0.4%. It is more frequent in the second trimester, with an incidence of 4–6%. The lowest risk corresponds to normal vaginal delivery (3%), followed by planned cesarean section (10–15%), and intrapartum cesarean section (between 20% and 35%, depending on the use of prophylactic antibiotics). Overall, this condition occurs in 5% of deliveries. The prevalence of vasa previa ranges from 1 in 2761 pregnancies to 1 in 5000 pregnancies. Although the etiology of this condition is unknown there are identifable risk factors: Fig. 22.2 Placenta acreta is thought to be caused by damage to, or the absence of, the decidua basalis. Placenta increta and percreta also may occur. However, acreta is the predominant location.
Definitions
Diagnosis
Placenta Acreta
Placenta Previa
Puerperal Endometritis
Uterine Atony
Vasa Previa
Prevalence and Epidemiology
Placental Abruption
Placenta Acreta
Placenta Previa
Puerperal Endometritis
Uterine Atony
Vasa Previa
Etiology and Risk Factors
Placental Abruption
Placenta Acreta
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


