Postdischarge Nutritional Management of the Premature Infant
Utpala G. Das
Nutritional management of the premature infant following discharge from the hospital varies depending on the gestational age or weight at birth, occurrence of postnatal complications that affect nutrition (such as bowel resection for necrotizing enterocolitis), and the need for specialized nutritional supplementation due to an inability to take adequate calories orally or due to the risk of oral feeding. Feeding issues are discussed in Chapter 31, and specialized nutritional support is discussed in Chapter 33. Details of nutritional support prior to discharge from the nursery are discussed in Chapters 43 and 45. This chapter discusses the special nutritional needs of infants with a birth weight of less than 2.5 kg following discharge from the nursery.
THE PREMATURE INFANT IN THE NEONATAL INTENSIVE CARE UNIT
A widely accepted nutritional goal for the preterm infant is for growth and body composition of the premature infant to reflect that of a fetus of comparable postconceptional age. In practice, this is a difficult target to achieve because of problems encountered with the administration of adequate caloric feedings by either the intravenous or enteral route in the stressed premature infant. Despite efforts to promote growth during hospitalization, preterm infants usually accrue significant nutrient deficits during hospitalization, and at the time of discharge, most preterm infants born at weights less than 1500 g (very low birth weight) have moderate to severe growth failure. Infants with significant morbidities and infants born at less than 1000 g (extremely low birth weight) have more severe growth failure because they regain birth weight at a later age, and they gain weight more slowly.
Assessment of growth requires the use of specialized growth curves developed specifically to monitor the growth of premature infants.1,2 Term infants lose on average 5% to 7% of their birth weight during the first 3 to 4 days of life, regaining birth weight by days 7 to 10. In contrast, premature infants lose up to 15% of their birth weight over the first 10 days of life. In general, babies born between 24 and 29 weeks gestation do not regain birth weight until about 2.5 weeks after birth. When compared to expected in utero growth, these infants generally reach the 10th percentile by 32 weeks gestational age and continue to grow along or below the 10th percentile through discharge. Monitoring the adequacy of nutrition following discharge is important to assure optimal catch-up growth.
THE PREMATURE INFANT AFTER DISCHARGE
Cumulative energy and protein deficits accrue at 1 and 6 weeks age in infants born at 31 weeks’ gestation or earlier.3 These deficits tend to worsen when infants are fed a formula designed for healthy full-term infants or if they are fed with unsupplemented breast milk at discharge. Bone mineral content is usually decreased in premature infants after discharged from the hospital,4-6 so attention to calcium, phosphorus, and vitamin D intake is also critical to catch up bone mass accretion.7,8 The options, postdischarge, for feeding infants born at less than 2.5 kg include breast milk with or without human milk fortifier, preterm formula, postdischarge formula, and term infant formula. The selection depends on maternal preference, prenatal history, and careful monitoring of infant growth parameters.
 BREAST MILK FEEDING
BREAST MILK FEEDING
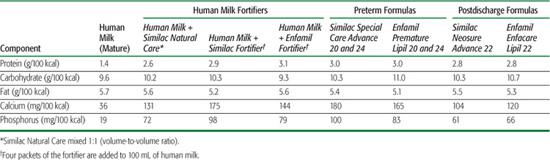
Breast milk is generally recognized as the best choice for enteral feeding. Aside from its nutritional value, it provides beneficial digestive enzymes and immunologic and antimicrobial factors. Hospitalized premature infants receive breast milk supplemented with a human milk fortifier to provide additional calories, protein, vitamins, calcium, and phosphorus (Table 26.1). Improved growth is reported when human milk fortification is adjusted by using blood urea nitrogen as an index of protein adequacy.9 It is uncertain if breast milk alone provides sufficient nutrients to a premature infant after discharge from the hospital.10 Premature infants fed breast milk postdischarge are shorter and weigh less than formulafed infants,11 suggesting that postdischarge breast-fed premature infants may benefit from fortification of breast milk. However, the available data do not provide strong evidence that formula supplementation ultimately affects growth rates or development,12 so the benefits of supplementation in breast-fed infants remains uncertain. However, inadequate intake of calories and/or protein, iron, zinc, calcium, phosphorus, and vitamins can result in nutrient deficiencies.
Former premature infants should be fed on demand every 1.5 to 3 hours to assure adequate intake. Fortification of some feedings with milk fortifier or an enriched infant follow-up formula may be useful until the infant has catch-up growth to achieve a weight at the 10th percentile or if the baby is not gaining weight at an acceptable rate (20–30 g/day). If growth is inadequate, supplemental feedings with fortified breast milk (24 or 27 cal/oz with term formula powder) may be helpful. If poor growth persists, a review of the efficiency of breast-feeding should ensue, and supplemental feedings may be required. Preterm infants fed unsupplemented breast milk should be provided with additional iron (2–4 mg/kg, maximum dose of 15 mg/day) and vitamins (0.5–1.0 mL of standard liquid pediatric multivitamin per day until weight is 5 kg). If exclusively breast-fed, supplementation with a total of 400 IU of vitamin D is recommended after 2 months of age. An iron-fortified formula or a preterm discharge formula should be used at weaning from breast-feeding depending on age, as detailed below.
 FORMULA FEEDING
FORMULA FEEDING
Specialized formulas are designed for the hospitalized premature infant to assure adequate protein and essential nutrient intake provided the infant receives full enteral feedings. In comparison to standard term infant formula, preterm formulas contain more protein, sodium, calcium, phosphorus, and vitamins per 100 mL of formula (Table 26.1). If the typical preterm infant consumes 150 mL/kg/day of formula, the preterm formula provides 3 gm/kg/day of protein and 6.5 gm/kg/day of fat, with 50% of the fat provided as medium-chain triglycerides. Two studies have shown that continuing this preterm formula for up to 6 months postterm leads to better growth parameters compared to the preterm infant fed term infant formula or breast milk.13-15
Despite data that infants fed preterm formulas have better growth, these formulas are not recommended following discharge because of concerns that when fed ad lib, infants may ingest a dangerous level of certain nutrients if they ingest a high volume of the preterm formula. This has led to the development and marketing of separate preterm, postdischarge formulas designed to promote catch-up growth while minimizing the possibility of nutritional toxicities. The nutrient levels of these formula are at the upper end of the nutrient level range for healthy term infants; they contain a higher protein and energy content than term formula (but not in sufficient amount to promote excess fat deposition); additional calcium and phosphorus to promote bone mineralization; and additional zinc, vitamins, and trace elements to support growth (Table 26.1).11
Some studies have shown that premature infants fed a postdischarge formula for up to 9 months postterm had better weight and length gain and increased bone mass than premature infants fed term infant formula for the same length of time.16-19 However, the available data do not provide strong evidence that this practice impacts growth rates or development at 18 months postterm.20
Table 26-1. Macronutrient and Mineral Composition of Human Milk, Fortified Human Milk, Preterm Formulas, and Postdischarge Formulas
Despite the lack of convincing data, the use of a 22 kcal/oz preterm discharge formula for infants weighing less than 3000 g, or until they have achieved catch-up growth so that they are at the 10th percentile for adjusted age, is generally recommended.21 A higher-calorie formula (24–27 kcal/oz) may be required in infants who are not gaining weight adequately (20–30 g/day) or who are fluid restricted. When an infant achieves adequate catch-up growth, it is unclear if there is benefit from continued use of a preterm discharge formula or if this may contribute to subsequent overweight. In all cases, an iron-fortified term infant formula should be used until the infant is 1 year adjusted age. Vitamin supplementation is generally not required in the formula-fed infant who is otherwise growing normally.
 MONITORING
MONITORING
Monitoring of growth parameters (weight, length, head circumference) is critical so that nutritional deficiencies are recognized. Growth charts based on a large cohort of premature infants have been developed by the Infant Health and Development program for 2 birth weight ranges: 1500 g or less and 1501 to 3500 g.22,23 Other charts may be found at http://www.biomedcentral.com/1471-2431/3/13/figure/F2?highres=y, and an interactive tool to correct for gestational age is available at http://www.medcalc.com/growth. These charts combined with those available from the Centers for Disease Control and Prevention and the World Health Organization provide a reasonable assessment of appropriate growth, and it is often useful to plot infants on both charts.24 Measurements should be plotted according to the corrected age, which is determined by subtracting the number of weeks of prematurity from the infant’s actual chronological age. Corrected age should also be applied when the standard growth charts are used until the child reaches age 2 years for infants born at birth weights greater than 1000 g. In those with birth weights less than 1000 g, the corrected age may be used until age 3 years.
Soy formulas are not recommended for feeding any preterm infants because of the decreased bioavailability of calcium and phosphorus in these products. Routine laboratory follow-up in the otherwise healthy premature infant who is receiving appropriate nutrient and supplement intake is not recommended. Exclusively breast-fed infants will need close follow-up of growth parameters, anemia, and bone disease (low serum phosphorus and an elevated alkaline phosphatase). Much of the data available on optimal postdischarge nutrition is based on growth data of former premature infants at 1 to 2 years of age. Long-term data on the impact of various nutritional management approaches on neurodevelopmental outcomes and on the risk for other disorders, such as obesity and metabolic syndrome, are lacking.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


