Pleural Effusions
Angela Lorts
INTRODUCTION
A pleural effusion is an accumulation of fluid between the parietal and visceral pleura. Normally, fluid is produced by the capillaries of the parietal pleura and absorbed by the capillaries of the visceral pleura; only a trivial amount of fluid is left within the pleural space. The Starling relationship governs the net flow of fluid at each capillary bed:
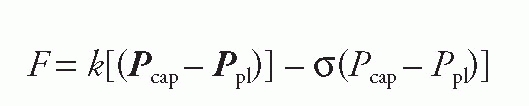
A larger difference between capillary and pleural hydrostatic pressure, or a smaller difference between capillary and pleural oncotic pressure, results in a larger amount of fluid left in the pleural space. Lymphatic drainage normally removes excess fluid from the pleural space. Accumulation of a pleural effusion may result from increased capillary hydrostatic pressure, decreased hydrostatic pressure in the pleural space, decreased capillary oncotic pressure, capillary leak, lymphatic obstruction, movement of fluid from the peritoneal space, or a combination of these factors.
Pleural effusions are classified according to their etiology as transudative or exudative. Pleural fluid analysis can often distinguish a transudate from an exudate and serves as the first step in the differential diagnosis.
Transudative effusions are usually secondary to increased capillary hydrostatic pressure or decreased capillary oncotic pressure. The most common etiology of a transudative effusion is congestive heart failure.
Exudative effusions are typically seen in diseases that injure the capillary membrane, result in increased capillary permeability, or impair lymphatic drainage. A broad differential diagnosis is implied by an exudative effusion and may require more extensive workup.
Transudative Effusion
Cardiac
Congestive heart failure
Increased pulmonary arterial pressure
Superior vena caval obstruction
Constrictive pericarditis
Pulmonary
Acute atelectasis
Hepatic
Cirrhosis
Hypoalbuminemia
Renal
Peritoneal dialysis
Nephrotic syndrome
Iatrogenic
Extravasation from subclavian or jugular central venous lines into the pleural space
Endocrine
Hypothyroidism
Exudative Effusions
Infectious
Bacterial infection (Most common—Streptococcus pneumoniae, Staphylococcus aureus)
Viral infection (Most common—Adenovirus)
Mycoplasma infection
Fungal infection
Parasitic infection
Neoplastic
Hematologic neoplasm
Cervical teratoma
Pleural mesothelioma
Pheochromocytoma
Wilms tumor
Metastatic sarcoma—Ewing sarcoma, rhabdomyosarcoma, and clear cell sarcoma
Squamous cell carcinoma
Bronchogenic carcinoma
Gastrointestinal Disease
Esophageal rupture
Sub-diaphragmatic abscess
Pancreatic pseudocyst
Acute pancreatitis
Intrahepatic abscess
Pulmonary Disease
Pulmonary embolism
Acute respiratory distress syndrome
Chronic atelectasis
Hemothorax
Collagen Vascular Disease
Rheumatologic—rheumatoid arthritis, systemic lupus erythematosus, sarcoidosis, and Wegener granulomatosis
Sjögren syndrome
Lymphatic
Traumatic chylothorax
Obstruction of lymphatic drainage
Congenital lymphangiectasis
Noonan syndrome
Lymphedema
Iatrogenic
Radiation therapy
Surgery
Esophageal sclerotherapy
Extravasation from subclavian or jugular central venous lines
DIFFERENTIAL DIAGNOSIS DISCUSSION
If the etiology of the effusion is unclear, the distinction should be made between a transudate and an exudate by thoracentesis and pleural fluid analysis.
Transudative Effusions
Transudative effusions usually resolve with treatment of the underlying disease process.
Exudative Effusions: Infectious Causes
Parapneumonic Effusions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


