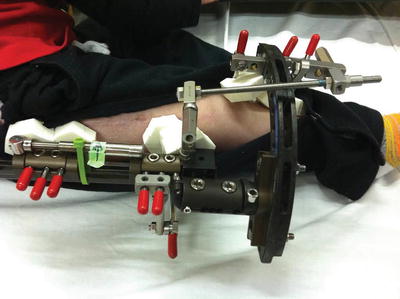
Fig. 12.1
Orthoplast custom foot splints are fabricated prior to discharge from the hospital. In case of monolateral fixators a ring is attached to the fixator for easy application of the foot splint using Velcro straps
Lengthening or Correction Phase
Based on variables such as the underlying diagnosis, need for multi-segment lengthening, amount of deformity and social considerations, there are three different rehabilitation pathways that most patients take after surgery: outpatient physical therapy with one to two sessions per day for 3–5 days per week, a day program with two to three sessions of therapy a day for 3–5 days a week, and inpatient rehabilitation with extensive physical therapy in a rehabilitation hospital [4]. The goals of physical therapy during the lengthening/correction phase are to maximize joint range of motion and maintain muscle tone and flexibility. Early joint mobilization is imperative to prevent contractures. Barker et al. [5] found that greatest loss of motion across joints occurred between surgery and commencement of distraction indicating pain as the primary cause. Aquatic therapy is a good adjunct to land therapy for patients with multi-segment lengthening and those undergoing bilateral lower extremity lengthening when full weight bearing is not allowed (Fig. 12.2).


Fig. 12.2
Chlorinated, heated, hydrotherapy pool for promoting increased range of motion and muscle strength
Consolidation Phase
In this phase, the goal of therapy is to maximize range of motion and continue to improve strength. Weight bearing and exercises that promote axial loading of the bone are encouraged. If patients have lost substantial knee range of motion, such as development of flexion contracture after tibial or femoral lengthening, then aggressive splinting across the knee joint with customized bracing or casting is done (Fig. 12.3). It is best to treat these contractures before the removal of external fixator since treatment of contracture after removal of fixator may lead to insufficiency fractures due to excessive stress and unresolved soft tissue tension.
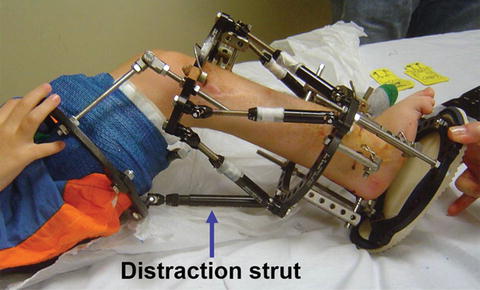
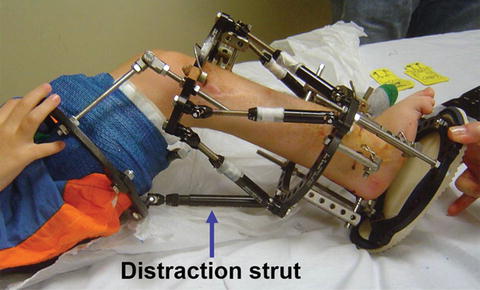
Fig. 12.3
Use of a Taylor Spatial Frame™ strut to apply an extension force in a patient who developed severe knee flexion contracture during tibial lengthening for fibular hemimelia limb deficiency. Thigh cuff using fiberglass casting is linked to the external fixator with hinges
Post Frame Removal
Gradual recovery of range of motion and functional strength through progressive exercises is the focus of physical therapy after removal of the fixator [4]. At this stage, there is a concern for fracture through the pin sites and at the newly formed bone of the lengthening regenerate [6]. It is recommended to be cautious in the first 4–6 weeks after fixator removal to allow for bone healing at these areas and therapy may be delayed for a month [7]. Casts and braces may be utilized during this phase for providing additional stability to the lengthened bone [4]. Once physical therapy is resumed, it is recommended that closed chain exercises be started before open chain exercises. Closed chain exercises are weight-bearing exercises, providing axial loading to further strengthen the lengthened bone segment. Open chain exercises are exercises where the distal limb segment moves around the proximal axis, this leads to increase torque and stress on the weaker newly lengthened bone segment. Careful stabilization of the bone segment as close to the joint line as possible is necessary to avoid bending stress on the bone during mobilization with physical therapy (Fig. 12.4). Manual mobilization with adequate stabilization of the lengthened bone is a safe and effective way to regain motion. Gait training and return to normative function are other additional goals during this phase. Recovery is slowest immediately following fixator removal and speeds up between 6 months to 1 year postoperatively. No further recovery is typically seen after 2 years following fixator removal [2]. During this period, home exercise program and participation in activities play a big part in the final journey of return to full functionality.


Fig. 12.4
Careful stabilization of the femur and tibia are critical during therapy after fixator removal. Patient receiving hamstring stretch with posteroanterior mobilization. Therapist hands are placed as close to the joint line as possible
Box 12.1. Complications During Limb Lengthening
Muscle contractures
Muscle weakness
Joint stiffness
Nerve injury
Joint subluxation
Role of Physical Therapy in Management of Complications
After the index surgery, patients can experience bone and/or soft tissue complications, which can compromise functional outcomes. Temporary soft tissue dysfunction occurs in the majority of patients who undergo limb lengthening and deformity correction procedures. The severity of these complications and obstacles to lengthening are dependent upon the diagnosis, amount of lengthening or correction, soft tissue quality, level of osteotomy, technique and device used for surgical correction, and nerve complications [1]. In addition to physical causes of complications there are social reasons such as poor pain tolerance and inadequate family support that can lead to suboptimal results.
Examples of soft tissue dysfunctions include muscle and tendon contractures, muscle weakness, joint stiffness, nerve injury, and joint subluxation. Bone complications include poor bone formation, angulations of the regenerate bone, and insufficiency fractures. Therapeutic intervention is crucial to avoid permanent dysfunctions. The physical therapist needs to have adequate handling techniques and the skill to apply appropriate forces and stabilization in order to focus treatment targeted at the appropriate tissues (Fig. 12.5). It is a fine balancing act since excessive forces can cause bone to bend or fracture. The therapist must keep in mind that the stress strain curve for tissues in the human body alters with age [8]. Pediatric patients deform their soft tissue with much less force than adults. Bone and soft tissue complications can occur during lengthening and consolidation phases, as well as after the removal of the external fixator.
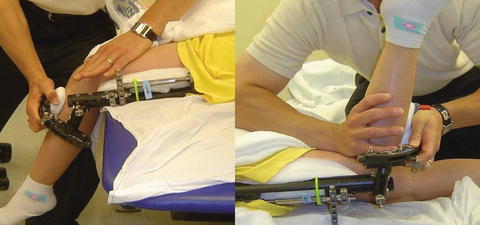
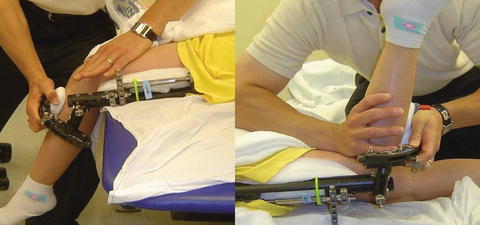
Fig. 12.5
Hand placement is critical for joint mobilization. Interior mobilization of the patella during knee flexion mobilization and correct posterior stabilization of the proximal tibia are important
Muscle Contractures
Contractures occur when elastic tissues and contractile elements are unable to accommodate change in their length following limb lengthening and deformity correction. Myofascial tissues resist such elongation more than most other tissues and are therefore more prone to contractures. A relative shortening of diarthrodial or biarticular muscles (crossing two joints) and the fascial component is often the cause of such contractures [1]. For example, the gastrocnemius develops passive tension much more rapidly in response to bony lengthening than does the soleus.
When muscles are kept in a shortened position, often due to postoperative pain early in the lengthening process the muscle adaptively shortens by absorbing sarcomeres to maintain efficiency. Prolonged stretch through a muscle has been proven to add sarcomeres. The therapist must devise a way to provide prolonged stretch of such muscles across adjacent joints. For such stretch to be effective it must have four critical components: (1) adequate intensity, (2) long duration, (3) adequate frequency with multiple repetitions, and (4) an active stretch component [8].
Problematic muscles should be identified early in order to treat contractures effectively. In tibial lengthening, for example, problem muscles are the gastrocnemius and toe flexors. As a result, patients are prone to develop knee flexion, ankle plantarflexion, and toe flexion contractures. Likewise, during femoral lengthening, the quadriceps (especially the rectus femoris) and hamstring muscles are predisposed to develop contractures resulting in deficits of flexion and potential for fixed flexion deformity across the knee joint, respectively.
Soft tissue restriction can be further complicated by the presence of scars from previous surgery, as is often seen in patients with long-standing limb deformities. Scar tissue lacks the elasticity of the native tissue and scar fibers are often laid down in a much more disorganized, rigid pattern, especially when the tissue is immobilized due to pain or lack of motion. Utilizing soft tissue mobilization with implementation, such as ASTYM™ (Fig. 12.6) and Graston™, can break down deficient, mature scar tissue and establish a more organized, pliable scar [8].
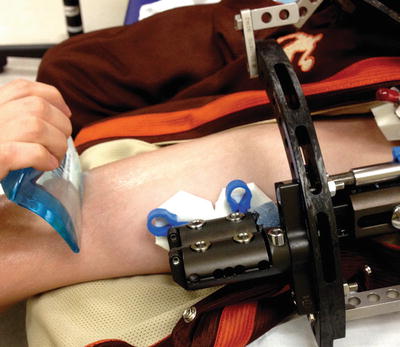
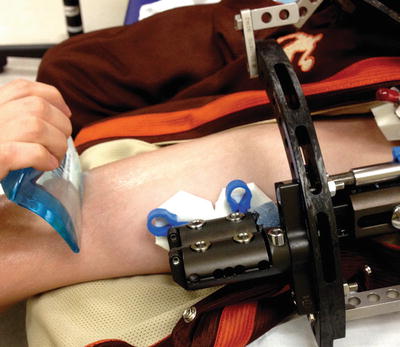
Fig. 12.6
ASTYM™ treatment for improving muscle flexibility and to promote remodeling of the fibrous tissue
Managing muscle contractures effectively is vital for a satisfactory clinical outcome following limb lengthening and deformity correction [1]. Passive stretching is an effective way to manage soft tissue contractures. Per our protocol, moist heat is applied prior to stretching to aid in collagen breakdown and improve stretch of connective tissue [8]. Analgesic medications administered 30 min prior to therapy help patients tolerate the stretch better. Reciprocal inhibition, activating the antagonist muscle before stretching the agonist, relaxes the muscle being stretched. Pin sites near the fascial and muscle planes are susceptible to inflammation. Thus gentle soft tissue mobilization and massage helps to manage tightness caused by adherent soft tissues around the pin. Another strategy to reduce pain around the pins during joint mobilization and stretching is to use tight pin wraps especially at sites near the knee or hip joint (Fig. 12.7). The tight pin wraps reduce skin motion during therapy and significantly reduce pain (Fig. 12.8). Stretching of biarticular muscles 10 times per session and uniarticular muscles five times a session with 20–30-s holds for each stretch is recommended. When stretching a biarticular muscle, stabilization at one joint is necessary during mobilization at the other joint to obtain maximum stretch. Ideally, a patient should have such treatments twice a day.

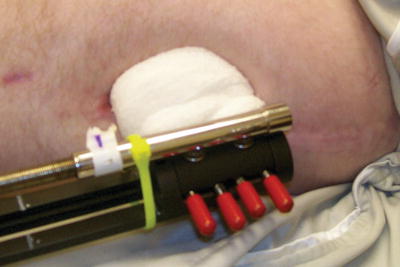

Fig. 12.7
Pin site around the hip joint can be painful due to movement of excess tissue during therapy. Massage around the pin site and use of tight wraps help reduce pain during therapy
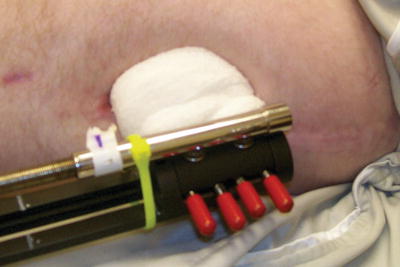
Fig. 12.8
A compression wrap around proximal femoral pins to avoid tissue motion during therapy. This technique reduces pain as well as risk of infection
Positioning and splinting strategies should also be used to manage soft tissue contractures. Optimal positions vary by affected body part. For example, patients who have undergone tibial lengthening should be positioned in knee extension and ankle dorsiflexion (Fig. 12.9). Knee extension, along with hip abduction, is a desirable position for patients undergoing femoral lengthening. Commercially made static splints (Fig. 12.10) augment therapeutic passive stretching by counteracting the connective tissues’ elastic response to passive stretching. Using a splint to place the muscle under tension for as many hours as possible, helps prevent contractures by obtaining plastic response in the connective tissue. Dynamic splints produce optimal plastic elongation (permanent elongation) of the connective tissue through a low load prolonged duration stretch (Fig. 12.11). Such a stretch also causes physiological remodeling of connective tissue through biochemical response. Dynamic splints work most effectively in treating knee contractures as they are a hinge joint. Be aware that splints work only in optimal positions and tension should always be increased gradually.


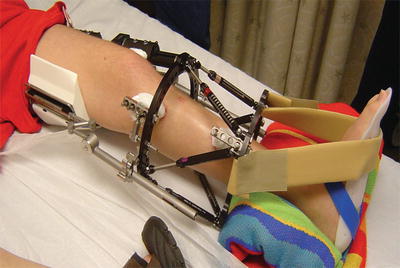

Fig. 12.9
Patient undergoing tibial lengthening and procurvatum deformity correction. Gastrocnemius and soleus contracture with lack of ankle dorsiflexion occurs commonly in these patients

Fig. 12.10
Commercially available walking shoe modification with Velcro straps to keep ankle in neutral dorsiflexion position
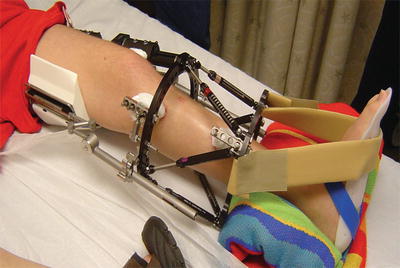
Fig. 12.11
Use of commercially available dynamic brace (Dynasplint™) attached to the proximal tibial ring to improve knee extension
Commercially made dynamic splints do not always provide the customization needed for an effective stretch. Therefore, the authors developed and utilize a custom knee device (CKD) for contracture management during or after external fixation (Fig. 12.12). This is a semirigid device made of a polyester and fiberglass cast of the thigh and lower leg with an aluminum hinge across the knee to allow for progressive stretching into the restricted range of motion. Elastic bands are utilized to provide the needed tension and the rigidity of the casting materials allows for minimal loss of the stretch energy to the desired tissues. Knee joint subluxation can also be managed utilizing the CKD with added straps at the knee joint to help approximate the joint and reduce the subluxation. The more the patient wears this device, the sooner the muscle truly lengthens and range of motion is restored. This concept can be utilized with tibial frames, as a thigh cast can be made with a half ring casted in and then attached to the tibial frame with a hinged joint. A telescoping strut can be added and the knee can be progressively straightened if a flexion contracture develops (Fig. 12.13). It is recommended to use these splints all night or at least 3–4 h per day.

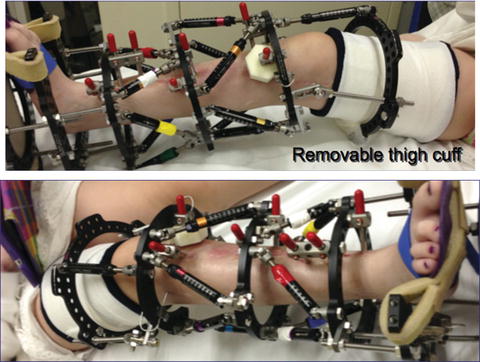

Fig. 12.12
Use of custom knee device (CKD) in a child with congenital femoral deficiency (CFD) undergoing femoral lengthening using monolateral fixator. Elastic bands offer continuous dynamic stretch in to extension. Patients are encouraged to use the device 8–14 h per 24-h period daily
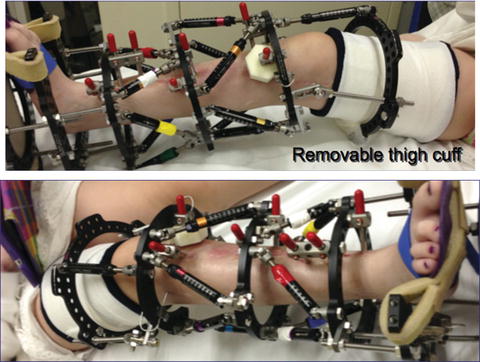
Fig. 12.13
Use of removable thigh cuff attached to tibial frame with hinges in a patient undergoing tibial lengthening. Taylor Spatial strut between ring incorporated in thigh cuff and proximal tibia ring allows for applying an extension stretch
Joint Stiffness
Muscle contractures, if not treated aggressively, lead to capsular and intra-articular adhesions. Contracture of biarticular muscles also introduces compressive force on the articular cartilage, which leads to a stiffness across adjacent joints [9]. Characteristics of a stiff joint include loss of motion and ease of movement within the joint’s available excursion. Joint stiffness is best prevented with active and passive motion. Manual traction with joint mobilization is beneficial and recommended when feasible. However, such mobilization can only be performed on joints that are not included in the external fixation construct.
Muscle Weakness
Patients may experience muscle weakness due to disuse atrophy and neurogenic inhibition with associated pain. Electrical stimulation and hydrotherapy are two modalities that can be used to manage muscle weakness. Electrical stimulation is used as an adjunct to a strengthening program and to augment voluntary muscle contraction. The most common area for electrical stimulation is the quadriceps muscle (Fig. 12.14). In our experience, as long as there is no direct contact of electrodes to the half-pins, it has been safely tolerated by children undergoing conventional distraction osteogenesis treatment with external fixation.
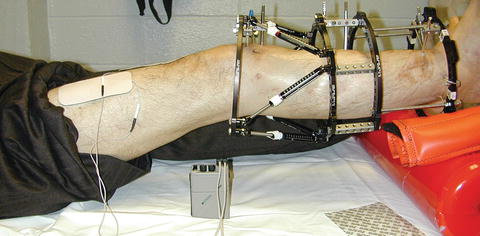
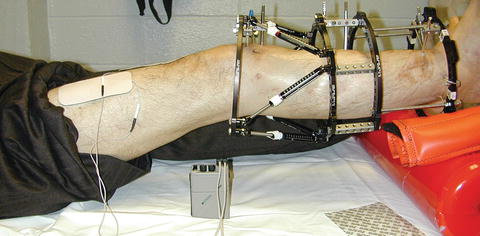
Fig. 12.14
Neuromuscular electrical stimulation of the quadriceps muscle with heel propped position. This position allows for active stretch as well as augmented strengthening of the quadriceps
At our center, typical electrical stimulation parameters are a biphasic pulse at a frequency of 35–70 Hz and pulse duration of 300–400 μs. In addition, an on-to-off ratio of 1:3 is recommended. Stimulation intensity should be adequate to cause strong contraction of the muscle. Patients tolerate newer electrical stimulation devices better using advanced frequency modulation software. Children tolerate higher intensity settings with these devices as compared to older devices. Family education for setup is recommended for incorporation of electrical stimulation into a home program.
Hydrotherapy helps avoid significant muscle weakness, especially in patients with bilateral external fixators or unilateral femur plus tibial fixators. Hydrotherapy also promotes increased active ROM (see Fig. 12.2). Buoyancy offsets fixator weight and facilitates muscle strengthening. Limb lengthening patients experience aquatic therapy in a heated, clinically chlorinated pool. Hydrotherapy allows for weight bearing early in the lengthening process, even if there are weight-bearing restrictions on land. With the water up to the nipple line, patients can utilize the buoyancy of the water to provide their bones with protection from gravity’s compressive forces to walk for continued cardiovascular health and muscle memory. The heated water brings muscle relaxation and freedom of motion, which allows for exercise and standing mobility. The chlorine levels at our center are kept at level 5 since patients get in with open pin sites. Purulent drainage from a pin site is a contraindication for getting into the pool. Daily assessment of pin sites are done by the treating land therapist as well as the aquatics therapist.
Joint Subluxation
Joint subluxation is a dreaded complication of limb lengthening surgery. Subluxations are caused by lack of opposition of the joint surfaces, muscle and tendon contracture, and ligamentous laxity. If a subluxation is not recognized and treated early, it can result in permanent sequelae. This can lead to significant reduction in range of motion, pain, and early onset of arthritis due to articular cartilage erosion. Knee subluxation in patients who have undergone femur lengthening for congenital femoral deficiency usually involves posterolateral translation of the proximal tibia. Such patients may have cruciate deficient knee joints, hamstring contracture, quadriceps inhibition, tight iliotibial bands, and flexed knee posturing. The combined effect of these conditions leads to unopposed posterolateral pull on the proximal tibia and in some cases also lateral subluxation of the patella [1]. Knee joint subluxation can occur during femoral lengthening if the joint is not protected in the frame or during lengthening with an intramedullary lengthening device. It can also occur due to unresolved residual tension in the soft tissues post fixator removal. Due to the high frequency of subluxations in the congenital femoral lengthening most surgeons prefer to extend the frame to the tibia with a hinge at the knee joint (Fig. 12.15) [1].