Persistent Hypoglycemia and Hyperinsulinemia
INTRODUCTION
Neonatal hypoglycemia can be transient (see chapter 75 on transient hypoglycemia) or persistent (hyperinsulinism, hypopituitaryism, disorders of gluconeogenesis, glycogenolysis, fatty acid oxidation, or inborn errors of metabolism). Hypoglycemia can be detrimental to the developing central nervous system, resulting in long-term effects. Neonatal hypoglycemia demands urgent diagnosis and treatment.
DIAGNOSIS/INDICATIONS
Definition of Hypoglycemia
Although the definition of persistent hypoglycemia continues to be debated and no consensus or research-based definition is available,1 many physicians use “operational threshold” levels of less than 45 mg/dL for diagnostic and 70 mg/dL for therapeutic purposes without scientific validation.2
Clinical Findings
History
Infants at higher risk of hypoglycemia should have their glucose checked soon postpartum, especially for infants who are small for gestational age (SGA), premature, or large for gestational age (LGA). Additional factors are a maternal history of diabetes during pregnancy (transient hyperinsulinism), history of consanguinity, or history of other children with unexplained deaths or glucose issues. The last 2 may suggest defects in glycogenolysis, gluconeogenesis, or ketogenesis. Timing of hypoglycemia may help differentiate etiology. Symptoms of hypoglycemia in the neonate may include seizures, cyanotic episode, apnea, “respiratory distress,” refusal to feed, brief myoclonic jerks, vomiting, somnolence, or subnormal temperature or there may be no overt symptoms. Intravenous glucose infusion rates (GIRs) in excess of 8 mg/kg/min suggest hypoglycemia secondary to hyperinsulinism.
Physical
Large for gestational age; SGA; prematurity; massive hepatomegaly; midline defects (cleft lip/palate, central incisor, holoprosencephaly, or in a male infant, small phallus); macroglossia; hemihypertrophy; or nystagmus should alert the clinician for possible hypoglycemia and its etiology.
Confirmatory/Baseline Labs
If the hypoglycemia is not readily responsive to initial measures (see chapter 75 on transient hypoglycemia), obtain “critical” labs listed in Table 105-1. The blood glucose concentration must be determined immediately using a laboratory enzymatic reaction. Falsely low glucose levels will be reported if there is a delay in processing secondary to metabolism of glucose in the specimen by erythrocytes. A special procedure may be needed for collection of lactic acid or ammonia.
Table 105-1 Critical Laboratory Values to Obtain at Time of Hypoglycemia
Serum glucose
Insulin
Ketones (serum or urine)
Cortisol
Growth hormone
Ammonia
Lactate
Free fatty acids
Urine organic acids
Plasma amino acids
Acylcarnitine profile
IGFBP3
DIFFERENTIAL DIAGNOSIS
Congenital Hyperinsulinism
Congenital hyperinsulinism is the most common cause of persistent hypoglycemia of infancy.3 For laboratory features consistent with hyperinsulinemic hypoglycemia, see Table 105-2. Genetic etiologies are summarized in Table 105-3.
Table 105-2 Laboratory Features of Hyperinsulinemic Hypoglycemia
Persistent hypoglycemia (<50 mg/dL)
Insulin (>2 μU/mL)
Serum ketones: β-hydroxybutyrate (<2 mmol/L)
Urine ketones: absent
Low serum free fatty acid (<1.5 mmol/L)
Normal cortisol and growth hormone
Glucagon stimulation test: positive (>30 mg/dL response to 1 mg glucagon)
Table 105-3 Genetic Forms of Hyperinsulinism a
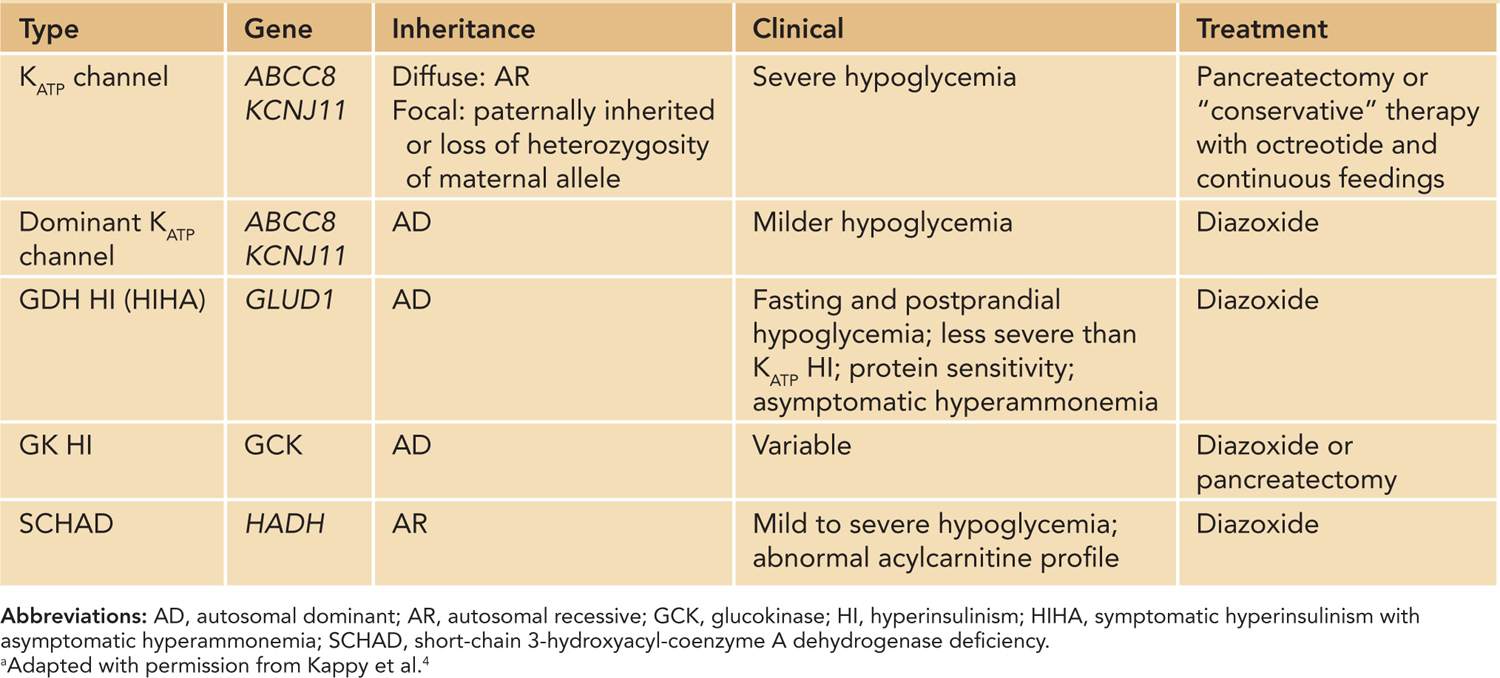
Mutations of the KATP Channel
The most common cause of hyperinsulinism is ABCC8 (SUR-1) or KCNJ11 (Kir6.2). Autosomal recessive (AR) mutations in these genes cause focal (AR in paternal allele or loss of heterozygosity of maternal allele) or diffuse islet cell hyperplasia. Usually, neonates are LGA with severe hypoglycemia after delivery. Frequently, this is diazoxide unresponsive. Autosomal dominant mutations of these genes cause less-severe hypoglycemia that usually is diazoxide responsive.
Glutamate Dehydrogenase
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


