Fithian et al.15 investigated acute, first-time PFI. However, his patient population included both pediatric and adult patients. He also found that younger patients, age 10 to 17 years, were more likely to develop recurrent PFI than older adult patients.15
Interestingly, Lewallen et al.16 demonstrated that patients older than the age of 40 years presenting with an acute, first-time patellofemoral dislocation had a PFI recurrence rate of 0%.16 A positive family history for PFI was a risk factor for recurrent PFI after first-time patellofemoral dislocation in a study by Palmu et al.17 It was also a risk factor for the development of contralateral knee PFI in studies by Fithian et al.15 and Palmu et al.17
Female sex is not a risk factor for developing recurrent PFI after an acute first-time patellofemoral dislocation.1,13,15,17
Fithian et al.15 demonstrated that patients presenting with a previous history of PFI (chronic nontraumatic PFI) are more likely to be older (median age of 21 years) and female (70%). They are also 6.6 times more likely to have recurrent PFI compared to patients presenting with an acute first-time patellofemoral dislocation.
A detailed clinical evaluation and the supplemental use of radiographic tests are crucial to determine the appropriate diagnosis, risks for recurrent instability episodes, and treatment for patients presenting with PFI. This assessment should also be divided into those patients presenting with an acute, first-time patellofemoral dislocation and those presenting with a previous history of PFI.
FIRST-TIME PATELLOFEMORAL DISLOCATION
This is usually a traumatic and painful injury. Occasionally, the reduction of the patella requires anesthesia or sedation. To avoid damage to the patellar and trochlear cartilage, the reduction should be performed by extending the knee while holding the patella in the lateral dislocation position. Reduction attempts with the knee in higher degrees of flexion should be avoided.4
The physical exam can be difficult in these patients due to pain from the recent trauma. It is important to assess the medial soft tissue complex of the knee. The MPFL and VMO are often torn. Special attention should be paid to any swelling or ecchymosis in this area. A large hemarthrosis can develop if an osteochondral fracture of the patella or trochlea occurred during the dislocation or reduction events. A recent study demonstrated that 38% (46/122) of adolescent patients with an acute patellofemoral dislocation had a displaced osteochondral fracture.18
Radiographs of the knee (anteroposterior [AP], lateral, and Merchant views) should be obtained to assess for osteochondral fractures and the status of the physis. The distal femoral and proximal tibial physes should be graded as open, closing, or closed. The radiographs can also be assessed for patellar height and trochlear dysplasia. For both to be assessed accurately, a perfect lateral radiograph (medial and lateral posterior condyles overlapping) of the femur should be obtained with the knee in 30 degrees of flexion.
The Caton-Deschamps (C-D) index has been validated to assess patellar height in children and adolescents.19 The mean C-D index in normal children and adolescents was 1.06 ± 0.21. Intraobserver and interobserver reliability studies showed excellent reliabilities with an intraclass correlation coefficient that was between 0.930 and 0.944 (95% confidence interval). A C-D index greater than 1.2 is considered to be diagnostic for patella alta. The Insall-Salvati index can also be used, but it is not validated in children and adolescents (Fig. 15.1).

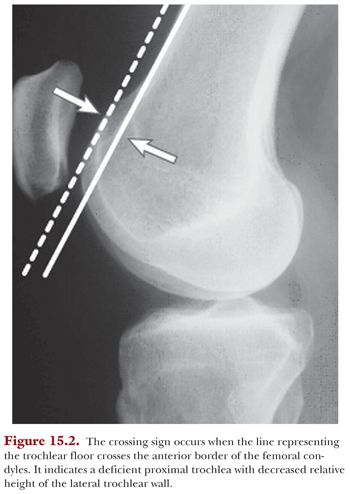
The Dejour classification is used to determine if a patient has trochlear dysplasia.20 Type A dysplasia is characterized by a shallow trochlea. On the Merchant (axial) view, the shallow trochlea will have a sulcus angle that measures greater than 145 degrees. The lateral x-ray will demonstrate a crossing sign. The crossing sign occurs when the line representing the trochlear floor crosses the anterior border of the femoral condyles. It indicates a deficient proximal trochlea with decreased relative height of the lateral trochlear wall21 (Fig. 15.2).
Type B dysplasia is characterized by a flat trochlea on the axial radiographs and a supratrochlear spur on lateral x-rays. The supratrochlear spur is an extension of the trochlear groove above the anterior cortex of the femur (Fig. 15.3).

Type C dysplasia is characterized by the presence of a crossing sign and a double contour on the lateral x-ray as well as medial hypoplasia and lateral convexity on the axial x-ray. A double contour is seen on the lateral x-rays as a double line at anterior aspect of condyles. This occurs because the medial trochlea is hypoplastic.
Type D dysplasia is a severe form of trochlear dysplasia. There is significant asymmetry between the large lateral trochlea and hypoplastic medial trochlea as well as a cliff between the trochlear facets. This leads to a double contour and supratrochlear spur on the lateral x-ray. The Dejour classification has not been validated in patients with skeletally immature physes.
Should an MRI be obtained to evaluate a patient with a first-time patellofemoral dislocation? In my practice, I obtain an MRI if the patient has osteochondral fracture on x-rays, a noticeable joint effusion/hemarthrosis, or if the history and physical exam are unclear.
Seeley et al.18 demonstrated that 44% of the patients with osteochondral fractures had plain radiographs that were negative.18 The osteochondral fracture was only diagnosed after the MRI was obtained. If the osteochondral fracture is large enough to treat operatively, then the location of the MPFL rupture is important to determine preoperatively. Kepler et al.10 demonstrated that 61% of pediatric and adolescent patients with PFI had MRI evidence of injury to the patellar attachment of the MPFL. Twelve percent injured the femoral attachment, 12% injured both the patellar and femoral attachments, 9% had midsubstance injuries, and 6% had no identifiable injury to the MPFL.10
The MRI can also be used to assess trochlear dysplasia and the tibial tubercle to trochlear groove (TT-TG) distance.
Lippacher et al.22 recently compared lateral x-rays with MRI for determining trochlear dysplasia in patients with PFI. A two-grade system divided into low-grade (type A) and high-grade (types B to D) trochlear dysplasia was compared to the traditional four-grade system. The four-grade analysis showed fair intraobserver and interobserver agreements (24% to 78%), whereas the two-grade analysis showed good to excellent agreement (56% to 96%). The best overall agreement was found for the two-grade analysis on MRI scans (62% to 96%). The lateral radiographs tended to underestimate the severity of trochlear dysplasia compared with axial MRI.22
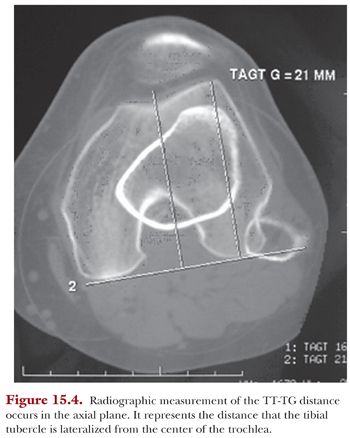
The TT-TG distance is a useful tool in guiding management for patients with recurrent lateral patellar instability (Fig. 15.4). Current recommendations for tibial tubercle transfer are based on TT-TG distance thresholds derived from adult populations. Recurrent patellar instability, however, frequently affects children, but normal and pathologic TT-TG values have not been established for pediatric patients. Recently published work by Dickens et al.23 sought to (1) confirm that MRI measurements for TT-TG distance in a pediatric population are reliable and reproducible, (2) determine whether the TT-TG distance changes with age, (3) define normal TT-TG distances in a pediatric population, and (4) confirm that a subgroup of pediatric patients with patellar instability have higher TT-TG distances.23 There were 618 MRIs retrospectively collected for patients who were 9 months to 16 years old. TT-TG distance changed with chronologic age in the pediatric population. Therefore, a percentile-based growth chart was developed in order to better depict normal TT-TG distances in the pediatric population. The median TT-TG distance for patients without patellar instability in this pediatric population was 8.5 mm (mean and 95% confidence interval, 8.6 ± 0.3 mm). Patients with patellar instability had higher TT-TG distances (median, 12.1 mm; P <.001).23 This percentile-based growth chart should be used to help direct surgical decision making regarding tibial tubercle transfer in pediatric and adolescent patients.