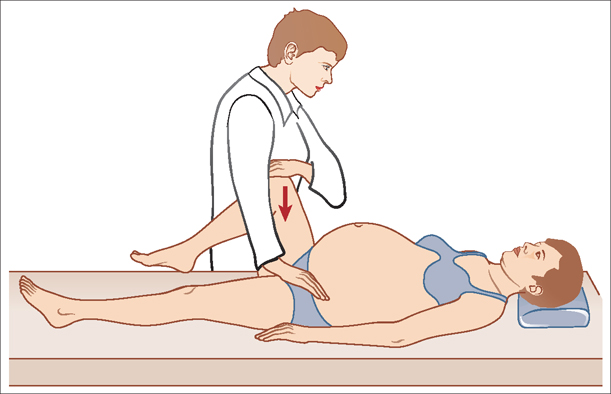
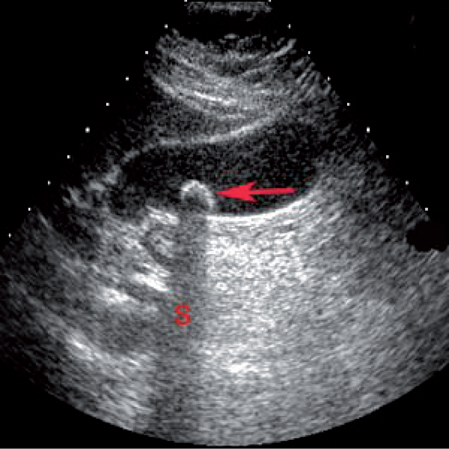
26 Other Medical Complications in Pregnancy E. Albert Reece This chapter discusses medical complications that commonly arise in pregnancy but are not covered elsewhere in this book. It includes a discussion of asthma, back pain, cholestasis and cholesytitis (two common, pregnancy-related liver disorders), diabetes, gastric motility disorders, and thyroid problems. Asthma: This is a chronic respiratory disease, in which the airways unexpectedly and suddenly narrow, often in response to an allergen, cold air, exercise, or emotional stress. Symptoms include wheezing, shortness of breath, chest tightness, and coughing. Back pain: This term refers to a pain felt in the back that usually originates from the muscles, nerves, bones, joints or other structures in the spine. Cholestasis: This is a condition in which the normal flow of bile in the gallbladder is affected by the high amounts of pregnancy hormones. It is more common in the last trimester of pregnancy when hormones are at their peak, but it usually goes away within a few days after delivery. Cholestasis is sometimes referred to as extrahepatic cholestasis, which occurs outside the liver, intrahepatic cholestasis, which occurs inside the liver, or obstetric cholestasis. Cholecystitis: This is an acute or chronic inflammation of the gallbladder and the second most common nonobstetric surgical condition in pregnancy (after appendicitis). Acute cholecystitis is usually the result of a gallstone impacted in the cystic duct. Diabetes: This is a disease in which the body doesn’t produce or properly use insulin. There are three major kinds of diabetes: type 1, type 2, and gestational diabetes. Type 1 diabetes is attributed to about 5 to 10 percent of all diabetetic patients in the United States and results from the body’s failure to produce insulin. Type 2 diabetes accounts for about 90 to 95 percent of the all diabetic patients in the United States and results from the body’s inability to produce sufficient amounts of insulin as well as the body’s resistance to insulin, which means that the body doesn’t use insulin effectively. Gestational diabetes is diabetes that arises or is diagnosed in pregnancy. It accounts for about 135 000 diabetic patients annually in the United States and occurs in approximately four percent of pregnant women. While most women recover from gestational diabetes after they give birth, they have an increased risk of developing type 2 diabetes in the future. Gastrointestinal motility disorders: This phrase is used to describe a variety of disorders in which the gut loses its ability to coordinate muscular activity, owing to aberrant endogenous or exogenous causes. Intestinal motility disorders may be primitive or secondary and may manifest in a variety of ways including: abdominal distension and recurrent obstruction; severe abdominal colicky pain; severe constipation; and gastroesophageal reflux disease or intractable, recurrent vomiting. Thyroid disorder: This disorder occurs when the thyroid gland is unable to supply the appropriate amounts of hormone to the body. As a result, the body’s metabolism and growth functions may not operate properly. The most common types of thyroid disease include: 1) hypothyroidism, in which the thyroid gland does not release enough hormones, and 2) hyperthyroidism, in which the thyroid gland produces too much hormones. Although the woman’s symptoms, medical history, and physical examination may suggest that she has asthma, it may be necessary to perform lung function tests to confirm an asthma diagnosis. Lung function tests may include: Spirometry. This is a noninvasive technique that measures how well a person breathes. During spirometry, the patient takes deep breaths and forcefully exhales into a hose connected to a machine called a spirometer (Fig. 26.1). Spirometry testing reveals two measurements that are important in diagnosing asthma: 1) forced vital capacity (FVC), which is the maximum amount of air someone can inhale and exhale, and 2) forced expiratory volume (FEV1), which is the maximum amount of air a person can exhale in 1 second. If certain key measurements are below normal for a person’s age, it may be a sign that that their airway is obstructed. Challenge test. This test involves deliberately trying to trigger airway obstruction and asthma symptoms by having the patient inhale an airway-constricting substance or take several breaths of cold air. If the patient appears to have exercise-induced asthma, you may want to ask her to do vigorous physical activity to trigger symptoms. After triggering the symptoms, readminister the spirometry test. If the patient’s spirometry measurements are still normal, it is likely that she does not have asthma. On the other hand, if her measurements have fallen significantly, it may mean she has asthma. Fig. 26.1 A digital spirometer used for measuring lung function. The most common, noninvasive diagnostic test performed in pregnant women with sacroiliac pain is the posterior pelvic provocation test (Fig. 26.2). The test is considered positive if it reproduces the woman’s back pain; it has been shown to be 81% sensitive and 80% specific for sacroiliac pain. Other physical exams and findings used to localize pain to the sacroiliac joint include the following: In some cases, however, a computed tomography scan or magnetic resonance imaging scan is needed to get a better look at the underlying cause of back pain. Cholestasis is diagnosed by a complete medical history, physical examination, and blood tests that evaluate liver function, bile acids, and bilirubin. Accurately diagnosing cholecystitis requires verification that the woman’s abdominal pain is caused by gallstones and not by some other condition that can mimic a gallbladder attack, such as acute appendicitis, inflammatory bowel disease (Crohn disease or ulcerative colitis), pneumonia, stomach ulcers, gastroesophageal reflux and hiatal hernia, viral hepatitis, kidney stones, urinary tract infections, diverticulosis or diverticulitis, pregnancy complications, and even heart attack. Fig. 26.2 The posterior pelvic provocation test is commonly used to help diagnose sacroiliac back pain in pregnancy. Fig. 26.3 A gallstone (red arrow) within the gallbladder produces a bright surface echo and causes a dark acoustic shadow (S). Ultrasound or other imaging techniques can usually detect gallstones (Fig. 26.3). Nevertheless, because gallstones are common and most cause no symptoms, simply finding stones does not necessarily explain a patient’s pain. In patients with known gallstones, the doctor can often diagnose acute cholecystitis (gallbladder inflammation) based on classic symptoms (constant and severe pain in the upper right quadrant of the abdomen). Imaging techniques are necessary to confirm the diagnosis. There is usually no tenderness in chronic cholecystitis. The following tests are used to diagnose diabetes: Test results indicating that a person has diabetes should be confirmed with a second test on a different day. Gestational diabetes is also diagnosed based on plasma glucose values measured during the OGTT, preferably by using 100 g of glucose in the liquid for the test. Blood glucose levels are checked four times during the test. If blood glucose levels are above normal at least twice during the test, the woman has gestational diabetes. Table 26.1 shows the above-normal results for the OGTT for gestational diabetes. The modes of diagnosing motility disorders are as diverse as the disorders themselves and are beyond the scope of this chapter. However, the methods used to diagnose functional gastrointestinal disorders (including motility disorders) are chosen based on a patient’s symptoms. To make the diagnosis as consistent as possible, a group of more than 100 international experts created the Rome criteria. Rome III, published in 2006, provides the most current diagnostic criteria for all of the functional gastrointestinal disorders (see Further Reading).
Definitions
Diagnosis
Asthma

Back Pain
Cholestasis
Cholecystitis
Diabetes
Gastrointestinal Motility Disorders
| When | Plasma glucose result (mg/dL) |
| Fasting | 95 or higher |
| At 1 hour | 180 or higher |
| At 2 hours | 155 or higher |
| At 3 hours | 140 or higher |
Thyroid Disorder
If hypothyroidism is suspected in a pregnant patient, the physician can perform a thyroid stimulating hormone (TSH) blood test. Just as in nonpregnant women, the TSH level will be increased if hypothyroidism is present.
The diagnosis of hyperthyroidism in pregnancy can be complicated, however, since some of the blood tests used for the diagnosis are altered because of the pregnancy. The diagnosis is based on high levels of thyroid hormones, T3 and T4, and a low level of TSH.
Prevalence and Epidemiology
Asthma
Asthma is the most common lung disorder during pregnancy. At any given time, up to 8% of pregnant women have asthma. The factors that increase or decrease the risk of developing asthma during pregnancy are not entirely clear. The likelihood of these attacks is not constant throughout pregnancy. It is at its highest during weeks 17 through 24 of pregnancy.
Although the vast majority of pregnant women with asthma and their babies have no complications, pregnant women with asthma do have a small increase in the risk for certain complications of pregnancy. Compared to women who do not have asthma, women with asthma are slightly more likely to have high blood pressure or pre-eclampsia, a premature delivery, a cesarean delivery, or a baby that is small for its age.
Back Pain
Reports suggest that between 50% and 80% of all pregnant women have back pain sometime during their pregnancy. It occurs more frequently later in the pregnancy as the weight of the baby increases. Although long-term pain is very rare, short-term pain tends to be dominant. Usually during the third trimester, 50% of pregnant patients will experience back pain. In contrast, by the postpartum period only about 9% of women experience back pain.
Cholestasis
Cholestasis occurs in about 1 of 1000 pregnancies but is more common in Swedish and Chilean ethnic groups.
Cholecystitis
The incidence of symptomatic biliary tract disease is 0.16% in pregnancy. However, approximately 80% of women with symptoms of gallbladder disease experience their first attack within one year of pregnancy, which seems to predispose women to developing biliary tract disease (see Etiology and Pathophysiology below).
Diabetes
Abnormal maternal glucose regulation occurs in 3–10% of pregnancies. Gestational diabetes mellitus accounts for 90% of cases of diabetes mellitus in pregnancy. Type 2 diabetes mellitus accounts for 8% of cases of diabetes mellitus in pregnancy. Given its increasing incidence, pre-existing diabetes mellitus now afects 1% of pregnancies. Studies suggest that the prevalence of diabetes among women of childbearing age is increasing in the United States. This increase is believed to be attributable to more sedentary life styles, changes in diet, continued immigration from high-risk populations, and the virtual epidemic of childhood and adolescent obesity that is presently evolving in United States (see Etiology and Pathophysiology below).
Gastrointestinal Motility Disorders
The average incidence is 3.5 per 1000 deliveries.
Thyroid Disorder
Thyroid disease is present in 2–5% of all women and 1–2% of women in the reproductive age group. Thus, thyroid problems are common in women who are pregnant.
Etiology and Pathophysiology
Asthma
Being pregnant has a significant impact on a woman’s respiratory physiology. Although the respiratory rate and vital capacity do not change in pregnancy, there is an increase in tidal volume, minute ventilation, and minute oxygen uptake, which lead to a decrease in functional residual capacity and residual volume of air as a consequence of the elevated diaphragm. There is also an increase in airway conductance, while total pulmonary resistance is reduced, possibly as a result of progesterone.
Due to all of these physiological changes, pregnant women often have episodes of hyperventilation in the latter half of pregnancy. This may lead to a chronic respiratory alkalosis during pregnancy with a decreased Pco2, decreased bicarbonate, and increased pH. The increases in minute ventilation and improved pulmonary function in pregnancy promote more efficient gas exchange from the maternal lungs to the blood. Therefore, changes in respiratory status occur more rapidly in pregnancy than in the nonpregnant patient.
Back Pain
The etiology of low back pain during pregnancy remains speculative. However, the scientific literature mentions as least three potential, pregnancy-related mechanisms: 1) biomechanical/musculoskeletal, 2) hormonal, and 3) vascular. In light of the variable clinical presentation of low back pain during pregnancy, a multifaceted etiology is an appropriate assumption.
Cholestasis
The etiology of choleostasis is not completely understood. Genetic, hormonal, and environmental factors may contribute to its pathogenesis. Clinical evidence suggests that estrogens play a role in the initiation of cholestasis. Indeed, cholestasis most commonly occurs in the last trimester, when estrogen levels reach their maximum. Also, the use of estrogen-containing oral contraceptives among women with a personal or family history of cholestasis could result in clinical features of cholestasis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


