growth phase, this length will have increased to 70 cm. During the first year of life, the spine will increase in length by 12 cm, and another 15 cm will occur between the ages of 1 and 5 years. The first 5 years is the time of greatest spinal growth, even greater than that of the adolescent growth period.
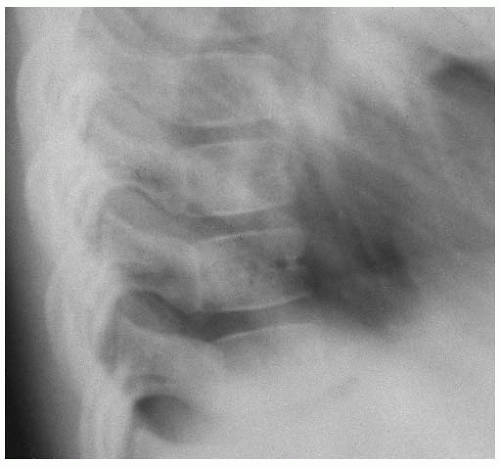 FIGURE 13-1 Normal lateral radiograph of the thoracic spine demonstrating the radiolucency of the intersegmental artery. |
seem to derive much of its strength from the attachment of the transverse ligament to the odontoid process and from the odontoid process attaching to the anterior arch by ligamentous structures.
above, one 1991 study that compared the performance of crawlers and non-crawlers on the Miller Assessment for Preschoolers showed that non-crawlers had lower average scores (23). It seems that the longer an infant crawls (to a point, of course), the better it is for the development of the nervous system.
growth wherein height might increase by 6 in. in as many months. This rapid growth phase, known as the “adolescent growth spurt,” is associated more with growth of the lower extremities than it is with growth of the spine, as noted above. Growth of the spine remains fairly constant throughout the adolescent period, growing at about the same rate from the age of 5 years onward. The adolescent phase is also a time when body structures are subjected to increasing trauma through sporting activities, increasing body weight, and increased velocity of movement. The effect of these changes can amplify any existing congenital or acquired spinal weaknesses, such as facet tropism, spondylolysis, spondylolisthesis, or the results of previous spinal trauma. Spinal problems in children can be due to many causes and can be categorized by age group (Table 13.1). Efficient proprioception from all joints is needed to reduce the risk of injury.
TABLE 13.1 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
clinical evaluation. Because of the increased flexibility of an infant’s spinal column, spinal trauma such as that which might be encountered during a motor vehicle accident is more likely to result in spinal cord injury with associated neurological symptoms rather than result in severe damage to the motion segment soft tissues, although this is extremely variable. It is important that every occupant involved in a motor vehicle accident, whether old or young, have a physical examination to check for the presence of such potential injuries. The potential for a relatively minor stiff neck after an auto accident to be the precursor to long-term spinal degeneration, which may eventually destroy the alignment, biomechanics, and integrity of joint structures, particularly in the cervical spine, must be recognized.
increasingly violent trauma inflicted upon a child by a parent or guardian. Fractures are the most common result of child abuse in the toddler, and skeletal x-rays are indicated in any case where suspicion of child abuse is present (32). Occasionally, an x-ray finding of an old, healed fracture site that does not correlate with the history and for which detailed questioning cannot uncover the cause may be evidence of previous or ongoing child abuse. Skeletal injuries can be dated so that the date of injury can be accurately estimated. The radiographic appearance of a healing bone after acute trauma follows a predictable pattern: 0 to 5 days, radiolucent fracture line is apparent but there is no evidence of healing; 5 to 10 days, periosteal new bone formation is evident; 10 to 14 days, soft callous formation; 14 to 21 days, hard callous formation (33).
spinal regions and/or restricted movements of the head and neck. The atlas vertebra fixed on the right side relative to the occiput has been reported in several studies to be the more frequent finding (35,38). Suboccipital strain can be managed effectively with specific adjustments of the cervical spine, usually only with a few treatments (35).
slightly. Adjustments began in the pelvis, which seemed to aggravate the torticollis. TMJ and cranial adjustments improved it. Cervico-thoracic adjustment allowed him to sit and the torticollis to improve. Over a period of 6 weeks, with periods of slight regression, he improved: his head was more centered, he was able to sit, although he was somewhat unstable, and he began to roll over and pull himself up (40).
and many cases of scoliosis are found during routine chiropractic physical examinations. Scoliosis screening is such an effective process for locating previously unidentified cases of scoliosis that screenings have become a regular occurrence in most schools.
exercises have been shown to reduce the rate at which the loss of joint mobility occurs (55). Spinal exercises and adjustments should be instituted for the purpose of increasing joint range of motion, or at least to preserve what movement remains. The patient should be advised to sleep flat on the back, on a firm mattress, with a low pillow under the head and neck to prevent exacerbating the flexion deformity of the spine. The following five assessment criteria for accurately measuring progress in the treatment of AS have been identified: cervical rotation, tragus to wall distance, lateral flexion, modified Schober’s test, and intermalleolar distance (56). These dimensions should be regularly monitored as a measure of the patient’s progress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree