Nonsurgical Treatment of Pelvic Organ Prolapse
Ingrid E. Nygaard
While surgery is considered the primary treatment for pelvic organ prolapse (POP), pessaries have been used to reduce prolapse for centuries and continue to fill an important niche in treating this disorder. Additionally, there is some, albeit scant, evidence that pelvic muscle exercises may hinder prolapse regression.
In 2001, 86% of American gynecologists queried prescribed pessaries, though most received minimal training in this area in their residencies. Further, 77% of American Urogynecologic Society members responding to a questionnaire about pessary use reported using them as first-line therapy for prolapse; 12% used pessaries only when surgery was contraindicated.
Some patients choose to wear a pessary as primary therapy for POP, while others use one temporarily when awaiting surgery. For some women, the option of a pessary allows flexibility in scheduling surgery. Others may wear a pessary only when doing an activity that exacerbates symptoms such as exercise.
A pessary may useful diagnostically. Patients generally have a variety of symptoms that may or may not be related to POP. By reducing the bulge for several days with a pessary, the patient and clinician get clues about whether reducing the prolapse surgically is likely to resolve symptoms that the patient may have, such as pelvic and back pain, urinary urgency and frequency, or voiding dysfunction. This may improve the chance that the patient has reasonable expectations of what surgery can and cannot “fix.”
Limited data from a small study by Handa suggest that wearing a pessary may have a therapeutic effect in women with POP: 19 of 56 women fitted with a pessary continued its use for at least 1 year. Four women had an improvement in stage of prolapse, and no women had worsening.
Choosing a Pessary
Today’s pessaries are made from medical-grade silicone, which is not allergenic or toxic, does not absorb odors, can be sterilized, and lasts for several years.
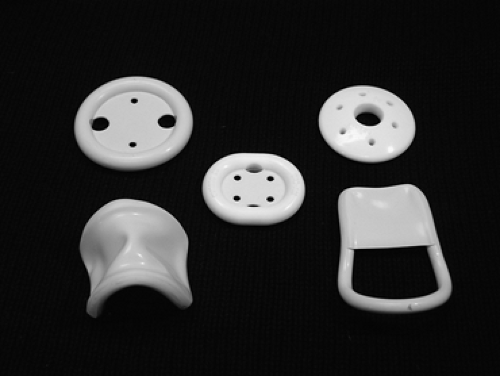
Some pessaries are easier for a woman to manage herself than are others. Pessaries can be loosely grouped into supportive pessaries, in which levator muscle tone is needed to keep the pessary in place (Fig. 50.1), or space occupying pessaries (Fig. 50.2), which, as their name implies, keep prolapse reduced by filling the vagina. Space-occupying pessaries are particularly useful for women with advanced POP who have minimal levator muscle tone and wide genital hiatuses.
Wu found that 70% of women with POP were successfully fitted with a size 3, 4, or 5 ring pessary. Pott-Grinstein also reported that the ring and donut pessaries were the most common pessaries used. In contrast, Sulak fitted 96 of 107 women with symptomatic POP with a Gellhorn pessary and gave the following reasons why they chose this pessary: the design makes it easy to insert and remove, the base of the pessary is large enough to support the proximal prolapse without exerting excessive pressure in any particular area, the concave base provides suction, and this pessary can be removed by the patient “with minimal discomfort.”
Most women can be fit successfully. In a prospective cohort study by Clemons and associates, 94 of 100 women with POP were fitted successfully in the office, while two women had pain and four expelled all pessaries tried. Clinicians tried an average of 2.2 pessaries per patient to achieve the best fit. The strategy of the clinic was to try a ring pessary with support first, followed by a Gellhorn if the ring was expelled. One week later, 54% of women were satisfied with the pessary, but it was expelled in 29% and caused pain or discomfort in 17%. Of the dissatisfied women, 29 were refit, 76% successfully. Overall, 73% of women had a successful 2-week pessary fitting trial. Women with a vaginal length of ≤6 cm and those with a wide introitus (four fingerbreadths wide or greater) had a lower chance of being successfully fitted. Ring pessaries with support were used in 100% of women with stage II prolapse and 71% of women with stage III prolapse. Gellhorn pessaries were used in 64% of women with stage IV prolapse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree