has one of the highest autism rates: 1 out of every 133 children and 1 out of every 79 boys. They also have a higher ratio of breech births, cesarean sections, and newborns who required more than 30 minutes of assisted ventilation among children with autism (6). Glasson et al. (7), from the University of Western Australia School of Psychiatric and Clinical Neuroscience, compared the birth records of the 465 children diagnosed with autism between 1980 and 1995 with the records of 1,313 randomly selected nonautistic children. They found that, when compared to the non-autistic group, the autism patients experienced more difficulties during pregnancy, labor, delivery, and during the neonatal period. They stated that the autism group was characterized by increased maternal age, being first born, a threatened abortion before 20 weeks’ gestation, fetal distress, and an elective caesarean (7). In a study published in Pediatrics, Juul-Dam et al. (8) looked at perinatal factors of 74 participants, 61 of whom were autistic and 13 of whom had PDDs-not otherwise specified (PDD-NOS). The study showed that some of the perinatal factors that had significantly higher incidences in the autistic group were found with the induction of labor and prolonged and precipitous labor. The PDD-NOS group showed results similar to those of the autism group. The specific reason for the induction of labor was not specified; therefore, it is difficult to assess the relevance, if any, to the later diagnosis of autism or PDD-NOS (8). Prolonged labor may be caused by fetal malposition, fetopelvic disproportion, excess sedation, inadequate contractions, and rupture of the fetal membranes before the onset of active labor. Risks associated with this include increased rates of operative vaginal deliveries or emergent cesarean section, an increased risk of intrauterine infection, and an associated increased risk of fetal compromise. Fetal compromise may take the form of asphyxia, infection, or head trauma from prolonged pressure, all of which may have lasting neurologic consequences. Some researchers also hypothesize that in children with childhood disintegrative disorder (CDD) predisposing genetic factors combined with environmental stressors such as prenatal or postnatal virus exposure or birth trauma have resulting brain deposition of amyloid and disruption of synaptic transmissions (9).
a tremendous amount of research demonstrating the neurotoxic affects from many environmental chemicals. There is ongoing study of the exposure affects from chemicals in the environment such as lead, mercury, polychlorinated biphenyls (PCBs), and pesticides. In 2004, researchers analyzed umbilical cord blood samples from 10 neonates, all born in US hospitals in August and September of that year. The 10 samples were from blood donated to the American Red Cross and were chosen randomly and came with no identification. The researchers had no geographical information about where the infants were born and only knew that the samples came from around the country. Of the more than 400 chemicals for which the researchers tested, 287 were detected in umbilical cord blood. Of these, 180 are known to cause cancer in humans or animals, 217 are toxic to the brain or nervous system, and 208 cause birth defects or abnormal development among animals. Scientists now refer to the presence of such toxins in the newborn as “body burden.” According to the study’s authors, the scope of testing was limited because chemical companies are not required to divulge methods for detecting the presence of their chemicals in the human body. They believed that had they been able to test for a broader array of chemicals, they would almost certainly have detected far more than 287. Of the toxins, mercury was found in samples from all 10 newborns, with the average concentration being 0.947 parts per billion. Additional toxins found during this study are listed in Table 25.1. The findings of this study are extremely alarming when considering the developing fetus and the possible long-term developmental implications these toxins may bring. An immature and porous blood-brain barrier, which does not fully form until 6 months of age, allows for greater chemical exposures to the developing brain. Also, children have lower levels of some chemical-binding proteins, which allow for more of any particular chemical to reach “target organs,” and systems that detoxify and excrete industrial chemicals are not fully yet developed.
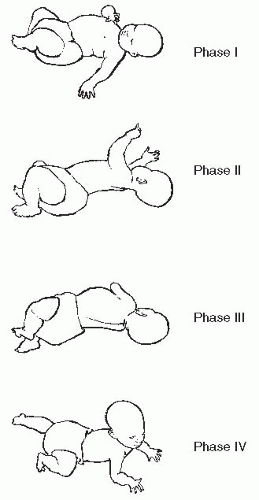
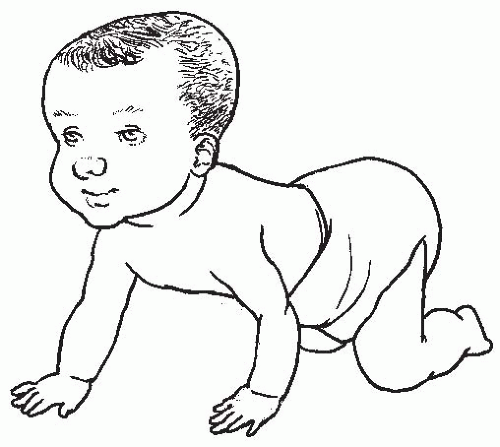
developmental screening procedures to determine if a child may be at risk for developmental delay and/or NDs. Many within the medical community who are involved in the research and treatment of children with NDs suggest that screening for specific developmental milestones as well as for retained primitive reflexes should become a regular practice for the pediatrician. Many pediatricians screen for various developmental milestones only within the first year of life. Few test for retained primitive reflexes beyond the first year. It is important to understand that developmental milestones continue to be significant beyond the first year of life, and primitive reflexes, if retained beyond the first year, have a significant impact on proper neurological development. For the doctor of chiropractic caring for the pediatric patient, it is crucial that he or she knows and understands specific developmental milestones and their significance should the child be delayed in reaching them (refer to Chapter 6 for specific milestones). Doctors of chiropractic caring for the pediatric population should also know how to examine for retained primitive reflexes beyond the first year of life and understand their neurological implications. The testing for retained primitive reflexes, as well as their significance, is discussed in detail in Chapter 24. Some of the latest research for early detection of autism will be presented later in this chapter. This type of information is important for the doctor of chiropractic to be aware of because many children are treated by their chiropractor on a regular basis from birth. Consequently, it is important that the doctor of chiropractic be skilled in early detection of any developmental delay.
TABLE 25.1 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Avoiding eye contact; not looking people in the face
Not pointing to objects
Trouble interacting, playing with, or relating to others
Unusual movements such as hand flapping, spinning, or tapping
Not using or seeming not to understand language
Delays in developmental milestones or loss of milestones already achieved
Playing with the same toy in a way that seems odd or repetitive
Not exploring the environment with curiosity or interest
4 or 5 out of every 10,000 live births, and it is estimated that 90% are boys and 10% are girls. Classic autism is not noted to be sharply on the rise, but it is with autism spectrum disorder (ASD) and regressive autism in which the dramatic increase in numbers is being seen. Kanner’s original description of autism noted that many of the patients had unusually enlarged heads. However, this observation did not receive much attention until recently, when postmortem and magnetic resonance imaging (MRI) studies began to confirm that in children with autism the brain is enlarged, although it still has not been confirmed whether all the brain regions and/or systems are enlarged equally.
TABLE 25.2 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the process of early diagnosis. Table 25.3 is referred to as the Checklist for Autism in Toddlers (CHAT) and is a standard recommendation to be performed during a child’s 18-month developmental checkup.
most important for executive function. It is involved in regulation necessary for working memory, organization, planning, problem solving, environmental monitoring, self-awareness, attention, mental flexibility, and abstract reasoning. It specifically controls initiative and initiation, disinhibition, and shifting of cognitive ability. The orbitofrontal cortex has deep connections to the basal ganglia complex and is responsible for behavioral regulation. Lastly, the medial cortex via the anterior cingulate circuit, with links to the limbic system, is responsible for emotional regulation. It modulates emotional arousal, expression of mood, and self-soothing strategies. Behavior may be repetitive and obsessive because of an inability to modify ones behavior to fit various social contexts. Therefore, the concept of “developmental disconnect” fits cohesively with the neurobehavioral features that are observed among autistic children, their emergence during development, and the heterogeneity of autism etiology, behaviors, and cognition. Executive function deficit is also associated with other NDs such as obsessive-compulsive disorder, Tourette’s syndrome, depression, schizophrenia, LDs, and ADHD. Because of its complexity, the frontal lobe develops slower than other parts of the brain, so executive functions do not fully mature until adolescence.
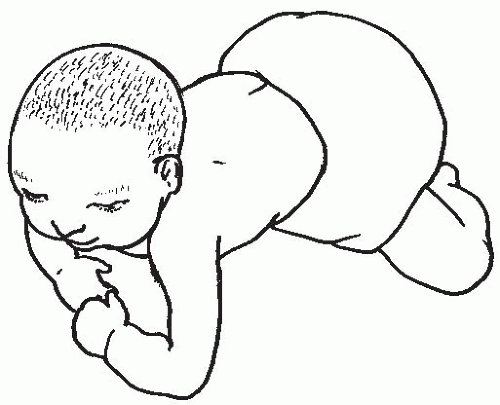
 FIGURE 25-5 “Army” crawl posture in an infant diagnosed with autism later. The infant may “drag” one of their arms or legs as they attempt to crawl. |
TABLE 25.3 | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
termed the “ascending reticular activating system,” which is a critical area involved in arousal and wakefulness (refer to Chapter 24 for more information on the role of the reticular activating system [RAS]). This particular system is thought to be critically involved in a number of functions, including stress, emotion, attention, motivation, decision making, learning, and memory. The connection between the LC and autism comes from decades of anecdotal observations that some autistic children seem to improve during times of fever and regress when the fever ends. The working theory is that the LC system is a neuronal network that is involved in mediating the cognitive and behavioral properties compromised in ASD; it also has regulatory control over fever. Fever-induced reversibility of autism suggests that there is temporary restoration of the neurological function of the networks subserving the LC-NA system (23). The role of epigenetics and NDs was discussed at the beginning of this chapter. Interestingly, the LC-NA system can undergo alterations of complex gene-environmental interactions, leading to dysregulation caused by epigenetic mechanisms during decisive developmentally critical periods (24). A prospective study of 30 children aged to 18 years with ASD during and after an episode of fever was published in 2007 in Pediatrics (25). The researchers found that fewer aberrant behaviors were recorded for febrile patients on the Aberrant Behavior Checklist subscales of irritability, hyperactivity, stereotypy, and inappropriate speech compared with control subjects, and all improvements were temporary. The researchers did suggest that more research is needed to prove conclusively fever-specific effects on ASD and to be able to explain the underlying neurological mechanisms, possibly involving immunological and neurobiological pathways, intracellular signaling, and synaptic plasticity. The LC is an area of the brain that is not irreversibly altered; therefore, if it is responsible for ASD, this gives hope that there are remedies for those with ASD. Because the LC is responsible for the processing of all sensory information from the body, the role of sensory processing therapy for children with ASD must be explored as one of the foundations of treatment.
subjects during four motor imitation tasks. Autistic subjects showed significantly greater right hemisphere activation during the imitation tasks than the normal subjects. This pattern was particularly evident among younger autistic subjects and during oral rather than manual imitation tasks (30). In another study, brain functional imaging using single photon emission computed tomography was used to measure left/right asymmetry and absolute values of regional cerebral blood flow in 18 autistic children ages 4 to 17 years and 10 agematched controls. The results confirmed the existence of left-hemispheric dysfunction in childhood autism, especially in the cortical areas devoted to language and handedness, leading to anomalous hemispheric specialization (31). In yet another study that looked at regional cerebral blood flow in children with autism, a statistically significant global reduction of cerebral blood flow was found in the group of autistic children compared with their normal counterparts. There was existence of left-hemisphere dysfunction, especially in the temporoparietal areas devoted to language and the comprehension of music and sounds. The researchers suggested that these abnormal areas are related to the cognitive impairment observed in autistic children, such as language deficits, impairment of cognitive development and object representation, and abnormal perception and responses to sensory stimuli (32). A device for measuring signal transfer within and between hemispheres has been developed at the Center for Neuropsychological Research at the University of Trier in Germany. The device was used for measuring brain asymmetry in tactile processing of autistic children. Results indicated that brains were more asymmetrical in autistic children than in controls, with the right hemisphere functioning quicker than the left (33). Melillo and Leisman (34) propose that there is a functional disconnect with reduced activity and coherence in the right hemisphere that would explain all the symptoms of ASD. If this is the case, they suggest that the best way to address the symptoms of ASD is via multimodal therapies that would include somatosensory, cognitive, behavioral, and biochemical interventions, all directed at increasing right hemisphere activity to the level that it would become temporally coherent with the left hemisphere. In one particular study of 14 autistic boys ages 6 to 14 years with relatively intact verbal functions and without severe or moderate MR, the autistic boys showed significantly lower driving characteristics of electroencephalographic photic driving. The findings were only in the right hemisphere and were compared with those of 21 normally developing boys (35). In one other study, the researchers examined regional grey matter differences and similarities in children and adolescents with ASD and ADHD in comparison with healthy controls using structural MRI and voxelbased morphometry. With regard to clinical criteria, the clinical groups did not differ with respect to ADHD symptoms; however, only patients with ASD showed deficits in social communication and interaction according to parental ratings. Structural abnormalities across both clinical groups compared with controls became evident as grey matter reductions in the left medial temporal lobe and as higher grey matter volumes in the left inferior parietal cortex. In addition, autism-specific brain abnormalities were found as increased grey matter volume in the right supramarginal gyrus. The researchers concluded that, although the shared structural deviations in the medial temporal lobe might be attributed to an unspecific delay in brain development and might be associated with memory deficits, the structural abnormalities in the inferior parietal lobe may correspond to attentional deficits observed among children with ASD and ADHD. By contrast, the autism-specific grey matter abnormalities near the right temporoparietal junction may be associated with impaired “theory of mind” abilities. These findings shed some light on both similarities and differences in the neurocognitive profiles of patients with ADHD and ASD (36).
detected a significant reduction in the total callosal areas and in the anterior one-third of the corpus callosum among patients with autism. However, 3D maps revealed significant reductions in both the splenium and genu of the corpus callosum. These abnormalities suggest aberrant connections between cortical regions, which is consistent with the hypothesis of abnormal cortical connectivity in autism (39).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree