Neonatal Resuscitation Procedures
Alan Fujii
Robert J. Vinci
Introduction
Neonates require cardiopulmonary resuscitation more commonly than any other age group. It is estimated that 10% of newborn deliveries will require some degree of resuscitation by a skilled clinical team (1). While newborn deliveries are an uncommon event in the emergency department (ED), those that occur in the prehospital setting or in the ED are frequently from high-risk groups (i.e., lack of prenatal care, trauma-induced labor, drug abuse) and may be more prone to complications. Newborn deliveries that occur outside of a hospital obstetrical unit place the neonate at risk for complications such as hypothermia, acute blood loss, hypoglycemia, and asphyxia. Therefore, it is imperative for the ED physician to be skilled in resuscitation techniques in order to minimize these complications. Neonatal asphyxia, the most serious of all neonatal complications, must be treated efficiently and aggressively to avoid devastating neurological injury to the newborn infant. For this reason, current recommendations state that “every birth should be attended by at least one person skilled in neonatal resuscitation whose sole responsibility is management of the newborn” (2). Standardized courses such as the Neonatal Resuscitation Program (NRP) provide a teaching format and curriculum for improving the resuscitation skills of all appropriate practitioners. Precipitous deliveries can occur anywhere in the prehospital setting, including in the home, in an office practice, or during a prehospital transport. Therefore, it is incumbent upon all practitioners, including nurses, physicians, midwives, and prehospital personnel, to be familiar with the techniques described in this chapter.
Anatomy and Physiology
Fetal Transition
Transition from fetal to neonatal life involves a series of rapid anatomic and physiologic adaptations. In fetal circulation, blood flow to the lungs is minimal as a result of high pulmonary vascular resistance, a patent ductus arteriosus, and low resistance of the systemic (placental) circulation. At birth, the fetus must establish the lungs as the site of gas exchange. Inherent in this process are the physiologic mechanisms that clear the airway of fetal lung fluid. Thoracic compression during labor, catecholamine stimulation of lymphatic drainage of alveolar fluid, and the newborn’s initial respiratory effort contribute to this process. The circulation, which previously shunted blood away from the lungs, must now fully perfuse the pulmonary vasculature, thus enabling adequate gas exchange at the alveoli-capillary unit.
Although surfactant production begins at approximately 24 weeks gestation, adequate amounts of surfactant to open alveoli may not be present until 36 weeks. A combination of events at birth act to initiate respiration. These events include the interruption of umbilical circulation, stimulation of peripheral and central chemoreceptors, and tactile and thermal
stimulation. The first few breaths must clear amniotic fluid from the lungs and establish a functional residual capacity. With the onset of respirations, the increase in oxygenation leads to the production of prostaglandins, which in turn reduces pulmonary vascular resistance. A fall in pulmonary vascular resistance decreases the right-to-left shunt through the ductus arteriosus, and the increase in left atrial pressure leads to subsequent closure of the foramen ovale. Fetal circulation now assumes the adult pattern (Fig. 36.1) (3).
stimulation. The first few breaths must clear amniotic fluid from the lungs and establish a functional residual capacity. With the onset of respirations, the increase in oxygenation leads to the production of prostaglandins, which in turn reduces pulmonary vascular resistance. A fall in pulmonary vascular resistance decreases the right-to-left shunt through the ductus arteriosus, and the increase in left atrial pressure leads to subsequent closure of the foramen ovale. Fetal circulation now assumes the adult pattern (Fig. 36.1) (3).
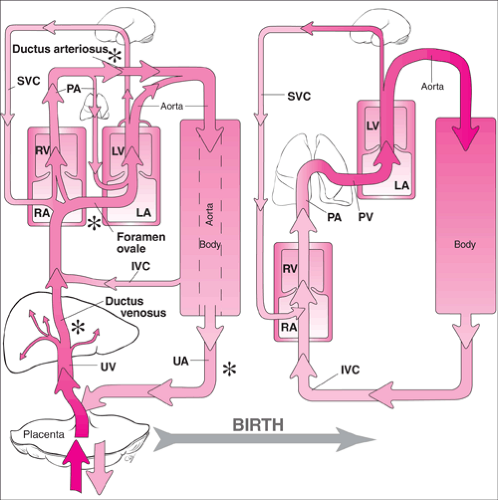 Figure 36.1 Schematic representation of transition from fetal to neonatal circulation. IVC, inferior vena cava; LA, left atrium; LV, left ventricle; PA, pulmonary arteries; PV, pulmonary veins; RA, right atrium; RV, right ventricle; SVC, superior vena cava; UA, umbilical arteries; UV, umbilical vein. Shading represents relative oxygen saturation. Structures marked with an asterisk (*) close soon after birth. See Figure 38.1 for a more detailed depiction of the umbilical vessels and their connections. |
Asphyxia
Birth asphyxia accounts for almost 20% of neonatal deaths (4). Neonatal asphyxia can result from multiple maternal and neonatal factors (Table 36.1). Asphyxia is the initial event that produces pulmonary vasoconstriction and delays closure of the ductus arteriosus. Fetal circulation is therefore maintained with a suboptimal increase in pulmonary blood flow. The goal with any asphyxiated newborn is to reverse the
asphyxia as soon as possible before permanent injury occurs. In an asystolic newborn, if adequate cardiac output is not established within the first 10 to 15 minutes of resuscitation, survival or survival without severe disability is unlikely (5,6).
asphyxia as soon as possible before permanent injury occurs. In an asystolic newborn, if adequate cardiac output is not established within the first 10 to 15 minutes of resuscitation, survival or survival without severe disability is unlikely (5,6).
When asphyxia occurs (either in utero or following delivery), an initial period of hyperpnea develops with sinus tachycardia. If hypoxia continues, respiratory effort ceases and bradycardia ensues (primary apnea). Providing oxygen and stimulation during this period in many cases will induce spontaneous respirations. If asphyxia continues, the newborn develops gasping respirations, the heart rate continues to decrease, and blood pressure falls. With the cessation of gasping respirations, secondary apnea develops, the newborn becomes unresponsive to stimulation, and neonatal asphyxial injury may develop. Positive pressure ventilation (PPV) must be initiated rapidly. The clinician must realize that when he or she evaluates a newborn in distress or full arrest, the asphyxiating event may have begun in utero; therefore, apnea at birth should be treated as secondary apnea, and resuscitation with positive pressure ventilation should begin immediately.
The Environment
Because of a large surface area to mass ratio, the neonate is susceptible to significant heat loss, and because many ED deliveries involve the birth of a premature newborn, heat loss may be a significant problem. Newborns, especially premature newborns, may be unable to effectively modulate their own temperature control and have limited capacity to generate heat. Without appropriate attention to thermal management, hypothermia may occur. Hypothermic stress in the newborn may contribute to acidosis, hypoglycemia, and respiratory depression (7). Hyperthermia should also be avoided, as it may lead to perinatal respiratory depression (8).
Indications
Basic techniques involved in neonatal resuscitation are applicable to the delivery of all newborns. While the delivery of a depressed or asphyxiated newborn can be anticipated in many cases based on antepartum or intrapartum history (Table 36.1), it may not always be possible to elicit these factors in the ED. Many asphyxiated newborns will have no risk factors and are only recognized at the time of birth. Resuscitation is required for about 80% of newborns with birthweights less than 1,500 g. Approximately 5% to 10% of term newborns require resuscitation beyond suctioning, drying, and stimulation. Preparation for high-risk situations in the ED requires proper equipment and personnel trained in the techniques of neonatal resuscitation. Because of the difficulty in accurately assessing gestational age in unanticipated deliveries, initiation of resuscitation is indicated unless it can be reliably determined that the newborn is less than 23 weeks gestation or less (9). Neonatology consultation in questionable circumstances should be obtained when possible.
TABLE 36.1 Factors Associated With Neonatal Asphyxia | ||
|---|---|---|
|
Equipment
Equipment requirements for more extensive resuscitations can be found in the chapters noted.
Suction Equipment
Bulb syringe
Mechanical suction with regulator
Suction catheter (6, 8, and 10 French)
Meconium aspirator (Chapter 37)



