Fig. 13.1
Carotenemia. Yellow-orange discoloration on the palms as compared with that of a normal control
Pathogenesis
Humans do not synthesize carotene; carotene must be ingested. Fruit and vegetables are rich in carotene, even the green ones. Milk, egg, legumes, grains, etc., also contain significant levels of carotene.
One-third of ingested carotene is absorbed across the intestinal lumen. Some carotene is converted to vitamin A, but most is accumulated in the epidermis and in the subcutaneous fat. Excessive ingestion of carotene leads to carotenemia and it is the most common cause. However there are several diseases that have been associated with carotenemia such as hypothyroidism, diabetes mellitus, liver and kidney disease, anorexia nervosa, food faddism, and rare cases of inborn errors of carotene metabolism. Carotenemia occurs when carotene levels are greater than 250 mg/dL [2, 5].
Treatment
Reassure parents.
Decrease the amount of carotene-rich food ingestion.
Education about carotene-rich foods.
There is no medical reason to reverse the carotene deposition in the skin. Discontinuation of excessive carotene intake typically returns the skin color to normal after 2–6 weeks. If other causes are suspected appropriate examination should be made.
Prognosis
Carotenemia is a benign condition.
Ongoing Research
Research on the biochemical and enzymatic pathways must provide insight into carotenemia particularly as it concerns infants with associated diseases.
Conclusion
Carotenemia affects infants of all races. In pediatric skin of color, yellow-orange discoloration is most noticeable on the palms. It is a frequent condition in children otherwise healthy. It disappears when dietary habits are changed. Parents must be informed.
Pernicious Anemia
Introduction
Hyperpigmentation of the skin is a clinical manifestation of vitamin B12 deficiency.
Vitamin B12 plays an important role in DNA synthesis. Various clinical manifestations mainly neurological, hematologic, and cutaneous are found in patients with vitamin B12 deficiency [6].
Epidemiology
It is a major heath issue with prevalence around 20 % in industrialized nations.
Breast-fed infants of strict vegetarian mothers are a risk group.
All racial and ethnic populations are affected.
Clinical Presentation
Mucocutaneous lesions can be the clue for the early diagnosis.
Unexplained and nonresolving skin lesions can be a red flag.
Hyperpigmentation is more common in darker-skinned patients.
Dermatological manifestations in patients with vitamin B12 deficiency include hyperpigmentation especially over the dorsum of the hands and feet with accentuation over the interphalangeal joints and terminal phalanges. Palmar creases, flexural areas, and pressure points are the most common affected areas (Fig. 13.2). The nails may have hyperpigmented streaks with pale nail beds. The association with pigmentation of oral mucosa (Fig. 13.3) is characteristic of vitamin B12 deficiency [8, 9]. Glossitis is the most common mucocutaneous manifestation followed by angular cheilitis. Hair changes manifest, as localized or diffuse depigmentation and vitiligo have been reported [9, 10].

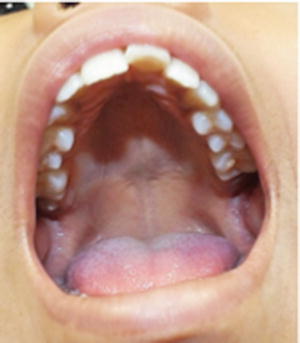

Fig. 13.2
Pernicious anemia. Palmar crease hyperpigmentation as compared with mother’s palm
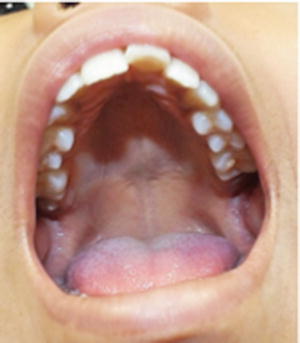
Fig. 13.3
Pernicious anemia. Pigmented lesions of oral mucosa
Pathogenesis
Vitamin B12 cannot be synthesized in the human body and must be supplied in the diet. Serum levels less than 200 pg/mL mean definite deficiency. The primary source of vitamin B12 is derived from animal products such as meat, eggs, fish, and milk. The body stores large amounts of vitamin B12 so it takes 2–6 years to develop symptoms of deficiency [6, 8, 9]. Causes of vitamin B12 deficiency are inadequate intake, malabsorption, and inborn errors of transport or metabolism. In children the must common cause is inadequate intake. The mechanism of hyperpigmentation is unknown; increased synthesis, defective transport, or a defect in distribution of melanin has been proposed [10].
Treatment
Initial replacement is through intramuscular injections.
Children with normal absorption can be maintained on oral replacement.
Treatment depends on treating the cause of deficiency besides supplementing with vitamin B12.
The treatment of vitamin B12 deficiency must be started immediately because diagnosis of vitamin B12 deficiency is often overlooked in its early stages. Supplementation must be continued every month if symptoms persist.
Prognosis
Affection of the hematologic, gastrointestinal, and nervous systems can be avoided with an early diagnosis and adequate treatment. Cutaneous hyperpigmentation is completely reversible with treatment.
Ongoing Research
Research on causes of vitamin B12 deficiency is necessary to prevent complications.
Conclusion
Vitamin B12 deficiency causes a range of disorders and affects all age groups. Diagnosis is difficult because its presentation varies from being asymptomatic to affecting multiple organ systems. Unexplained skin lesions that do not respond to therapy can be an indication of vitamin B12 deficiency.
Endocrinological Disorders
Acromegaly
Introduction
Oversecretion of growth hormone.
Overgrowth of acral bone and soft tissue.
Growth hormone excess causes gigantism in children and adolescence, and acromegaly in adults.
Epidemiology
3–4 per million per year.
Males and females are equally affected.
About 20 % begins during adolescence.
Acromegaly is a rare disorder. Virtually all patients have different tissue overgrowth with characteristic findings. Hyperpigmentation is more accentuated in patients with dark skin [11].
Clinical Presentation
Generalized increased pigmentation.
Macrognathia.
Enlargement of hands and feet.
The most obvious cutaneous changes related with excess secretion of growth hormone is the thickening of the skin, an increase in the size and function of sweat and sebaceous glands, and an increase in hair follicles. The generalized increased pigmentation in approximately half of the children generally is moderate along with changes of the skin. Hyperpigmentation is particularly noticeable in pediatric skin of color where the skin is more thickened resulting in coarsening of the facial features. The nails become thickened and hardened. Acanthosis nigricans can be seen in many patients. The metabolic effects include diabetes, hyperlipidemia, and hypertension [11–14].
Pathogenesis
Excessive production of growth hormone is usually due to a benign pituitary adenoma. Growth hormone stimulates production of somatomedin by the liver and it is the increase in somatomedin levels that accounts for most of the alterations presented in acromegaly. The cause of hyperpigmentation is not understood since growth hormone has not a known function in melanin production [11].
Treatment
Surgical removal of the pituitary tumor.
Residual disease requires somatostatin analogues.
Growth hormone replacement therapy is usually required.
Because clinical manifestations of acromegaly generally occur slowly, treatment is not corrective but rather preventive of further damage.
Prognosis
The skin changes can regress in days to weeks after lowering of growth hormone and somatomedin levels, although bony changes will persist.
Ongoing Research
Somatostatin analogues (e.g., octreotide) are increasingly being considered as potential primary therapy.
Conclusion
Acromegaly is a rare disorder secondary to growth hormone excess. The onset of symptoms is during adolescence in about 20 % of the cases. Approximately half of these children will develop diffuse hyperpigmentation.
Addison’s Disease
Introduction
Generalized hyperpigmentation precedes other manifestations.
Salt craving is characteristic.
Addison’s disease is an adrenal deficiency characterized by skin hyperpigmentation and salt wasting secondary to inadequate secretion of androgenic and corticosteroid hormones.
Epidemiology
Prevalence of 0.8–1.4 cases per 100,000 per year.
Congenital adrenal hyperplasia is the most common cause in children.
All races are affected.
Clinical Presentation
Diffuse bronze hyperpigmentation.
Oral mucosa may be affected.
Palmoplantar crease pigmentation.
Hyperpigmentation is the most striking cutaneous sign in almost all cases of the chronic variety of adrenal hypofunction. Children present a generalized increased skin color accentuated in sun-exposed areas particularly in dark-skinned children (Fig. 13.4). Other areas with marked pigmentation are sites of trauma, around scars, and over areas of friction. Mucosal surfaces develop blue-brown macules (Fig. 13.5). Color changes on mucous membranes and palmoplantar creases are less marked in dark-skinned patients than in Caucasians. Darkened hair and pigmented bands in the nail plate are usually present [16–18].




