Fig. 15.1
Metabolic control of calcium levels
Fig. 15.2
Vitamin D metabolism
In patients with osteoporosis, the bone is structurally normal but is reduced in overall amount. In children, osteoporosis may be idiopathic, as in juvenile osteoporosis, or may be due to disuse or chronic corticosteroid administration. The mechanism is uncertain, but numerous theories include increased bone resorption versus decreased bone formation, possibly due to deficient 1,25-dihydroxyvitamin D or calcitonin or due to a major interruption in transduction of mechanical forces that stimulate new bone formation [1, 3].
Hypophosphatasia results from a genetic error in the synthesis of alkaline phosphatase, the enzyme necessary for the maturation of the primary spongiosa in the physis. This condition leads to normal production of osteoid tissue but inadequate mineralization, with resultant skeletal deformities that resemble rickets [1, 3, 4].
Nutritional Rickets
General
The primary etiology of this condition is vitamin D deficiency in the diet. This deficiency leads to failure of calcification of cartilage and osteoid tissue. Vitamin D deficiency results in an inability to absorb calcium and phosphorus. Parathormone (PTH) is released in response to hypocalcemia. Subsequently, serum calcium levels become normal or slightly decreased, but phosphate and vitamin D levels remain low (Table 15.1). Thus, radiologically, the physes display an elongation and a hazy appearance related to alterations in the provisional zone of calcification [4, 5]. The widened growth plate differentiates rickets from more common physiologic angular deformities of the lower extremity [6]. With treatment, calcification occurs and radiographic appearance gradually normalizes.
Table 15.1
Biochemical abnormalities in rickets
Biochemical abnormality | ||||||
|---|---|---|---|---|---|---|
Type of metabolic bone disease | Calcium | Phosphate | ALP | PTH | 25 (OH) Vit D | 1,25 (OH)2 Vit D |
Nutritional | N | N/↓ | ↑ | ↑ | ↓↓ | ↓ |
Vitamin D resistant | N | ↓ | ↑ | N | N | N |
Vitamin D dependent I (inability to hydroxylate) | ↓ | ↓ | ↑ | ↑ | ↑↑ | ↓↓ |
Vitamin D dependent II (receptor insensitivity) | ↓ | ↓ | ↑ | ↑ | N/↑↑ | ↑↑↑↑ |
Renal osteodystrophy | N/↓ | ↑ | ↑ | ↑↑ | N | ↓↓ |
Treatment
The routine treatment for nutritional rickets include the supplemental administration of vitamin D. Radiographs typically show improved mineralization within 2–4 weeks of initiating medical treatment [4, 6]. If the child does not respond to vitamin D therapy, vitamin D-resistant rickets should be suspected. Because residual deformity is very rarely observed after adequate medical treatment of nutritional rickets, there is no specific orthopedic treatment besides follow-up to ensure acceptable lower limb alignment.
Rickets of Prematurity
Premature infants with comorbidities, followed up in intensive care units, sometimes present with pathologic fractures, probably caused by passive motion exercises. With treatment of the underlying rickets, the fractures consolidate with orthopedic immobilization techniques [4].
Drug-Induced Rickets
Certain antiepileptic medications, such as valproic acid and phenytoin, have been known to create rachitic changes in children [7] (Box 15.2). These drugs lower vitamin D levels through a P-450 microsomal enzyme system mechanism in the liver. Patients mostly present with pathologic fractures while on treatment for seizures. Medical therapy with vitamin D supplementation and consultation with the treating neurologist is helpful.
Box 15.2
Metabolic bone diseases can be caused by certain medications as well.
Remember that certain antiepileptics such as valproic acid and phenytoin may lower vitamin D levels in the body.
Vitamin D-Resistant Rickets (Familial Hypophosphatemic Rickets)
General
Vitamin D-resistant rickets involves a group of disorders in which normal dietary ingestion of vitamin D is insufficient to accomplish normal mineralization of bone [2, 6]. There are four major forms of vitamin D-resistant rickets, the most common of which is inherited as an X-linked dominant trait, followed in occurrence by an autosomal dominant type [2, 4, 6]. The inherent pathology is the renal tubule’s incapability to retain phosphate, which causes hypophosphatemia. The third group is characterized by failure of the kidney to accomplish the second hydroxylation of vitamin D. This condition can simply be treated medically, therefore orthopedic treatment is infrequently needed. In the fourth group, also known as renal tubular acidosis, the kidney excretes fixed base and wastes bicarbonate resulting in wasting of calcium and sodium [3, 6]. Laboratory findings are listed in Table 15.1.
Vitamin D-resistant rickets typically becomes evident between the ages 1 and 2 years, slightly older than nutritional rickets. The major complaints are delayed walking and angular deformities of the lower extremities (Figs. 15.3 and 15.4). Systemic manifestations are generally absent. The deformities are much more severe when compared to nutritional rickets. Once affected children begin to walk, genu varum develops, although genu valgum may occur in some children [4, 6]. Short stature is also a feature of hypophosphatemic rickets, with their standing height often being 2 standard deviations below the mean for their peers [8]. Radiologically, the physes are widened, there is genu varum and coxa valga, Furthermore, a varus deformity of the distal tibia often leads to varus malalignment of the ankle joint (Fig. 15.5). The upper extremities are involved, to a lesser degree, as well [4].
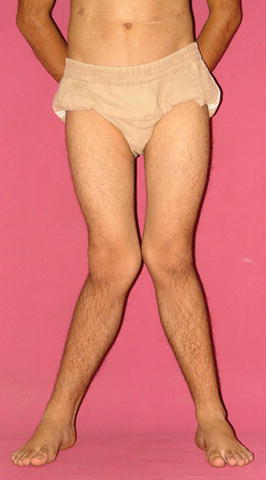


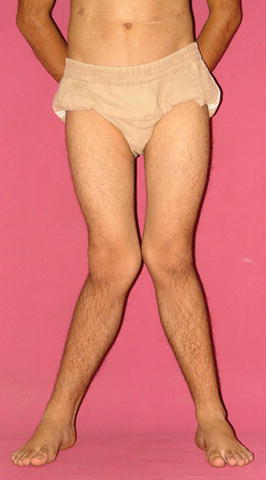
Fig. 15.3
Photograph of a patient with severe genu valgum deformity

Fig. 15.4
Photograph of a patient with severe genu varum deformity

Fig. 15.5
X-ray showing distal tibial varus deformity
Treatment
Medical Treatment
The standard treatment consists of oral supplementation of large doses of phosphorus along with administration of vitamin D. Studies have revealed that longitudinal growth is superior in children who receive vitamin D treatment [4]. Furthermore, treatment by growth hormone administration also increases height and has positive influence on bone density [9]. Recently, analogs of vitamin D3 (1,25-dihydroxy-vitamin D3) have been proved to be more effective than the previously used supplements [10].
Orthopedic Treatment
The orthotic management of skeletal deformities in patients with vitamin D-resistant rickets has not been successful. If patients complain of increasing pain and difficulty walking, angular deformities should be surgically corrected [4, 11]. The postoperative management should be done in close collaboration with the attending nephrologist or endocrinologist, since calcium levels tend to suddenly increase with postoperative immobilization period. The most common deformity seen in this patient group is a gradual anterolateral bowing of the femur accompanied by tibia vara (Figs. 15.6 and 15.7). In order to reach a physiologic lower extremity alignment, multilevel osteotomies are often necessary [4, 11, 12]. The mechanical axis can be slightly overcorrected during surgery. The suggested fixation modality varies among reports. While external fixation allows fine-tuning of the alignment postoperatively [13] (Fig. 15.8), intramedullary fixation and plate fixation have also been reported [12, 14–16] (Fig. 15.9; Table 15.2). Regardless of type of implants utilized, careful preoperative planning of the surgery for these multiplanar deformities is obligatory to successfully reestablish the alignment of the lower extremity.


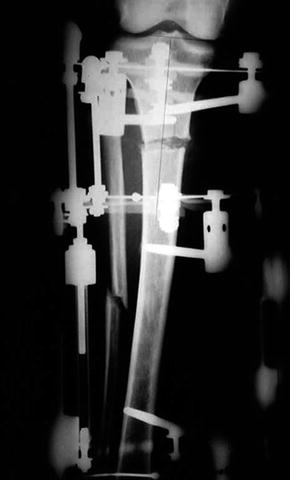


Fig. 15.6
X-ray of a patient with a anterior bowing of the femur

Fig. 15.7
Photograph of a patient with severe anterior bowing of the femur
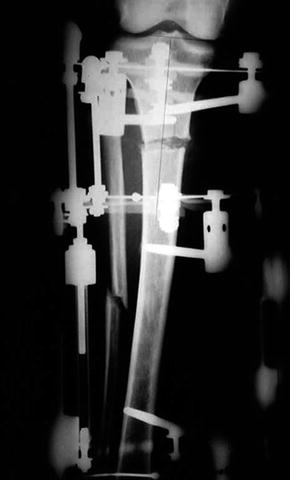
Fig. 15.8
X-ray of external fixation for the tibial deformity

Fig. 15.9
Intramedullary fixation of a tibial deformity correction
Table 15.2
Review of literature
Authors | Journal (year) | Title | Number of patients | Results |
|---|---|---|---|---|
Fucentese et al. | J Child Orthop (2008) | Metabolic and orthopedic management of X-linked vitamin D-resistant hypophosphatemic rickets | 12 | Single bilateral surgical correction was performed in six patients; one patient each had three and five corrections. Bone lengthening was performed in three patients. At last follow-up, the height of seven operated patients was within normal range. In addition, leg axis was normalized in six patients with mild genua vara in two. Bone healing was excellent: surgical complications were rare. In case of bone deformity, surgery can safely be performed, independent of age or bone maturation |
Kocaoglu et al. | J Bone Joint Surg Br (2011) | Combined technique for the correction of lower-limb deformities resulting from metabolic bone disease | 17 (43 segments) | 43 segments in 17 patients with metabolic bone disease underwent surgical treatment by the fixator assisted nailing technique. The deformity correction was achieved with a low complication rate. The use of intramedullary nail prevented recurrence of deformity and refracture |
Kanel et al. | J Pediatr Orthop (1995) | Unilateral external fixation for corrective osteotomies in patients with hypophosphatemic rickets | (29 segments) | Corrective osteotomies were performed on 29 bones in nine children with hypophosphatemic rickets. Use of the Orthofix external fixator enabled precise correction of the deformities without interruption of medical management |
Rubinovitch et al. | Clin Orthop Relat Res (1988) | Principles and results of corrective lower limb osteotomies for patients with vitamin D-resistant hypophosphatemic rickets | 10 (44 osteotomies) | Osteotomies were combined with shortening and compression plating. Recurrence of deformity occurred in 27 % of the cases. While osteotomies were safe and provided dramatic improvement to limb deformity, postoperative control of vitamin D metabolism was the one constant factor for maintenance of correction |
Petje et al. | Clin Orthop Relat Res (2008) | Deformity correction in children with hereditary hypophosphatemic rickets | 10 (53 segments) | 37 corrective operations were performed on ten children. Depending on the patient’s age, external fixation was used in 53 segments: Kirschner wires in 18, DynaFix in three, the Taylor patial Frame device in 13, and the Ilizarov device in 19. Internal fixation with intramedullary nailing was performed in 12. Deviation of the mechanical axis and knee orientation lines was increased at the follow-ups conducted during a period of 5–12 months. Additional follow-ups revealed a recurrence rate of 90 % after the first corrective procedure and 60 % after a second procedure |
Song et al. | Acta Orthopedica (2006) | Deformity correction by external fixation and/or intramedullary nailing in hypophosphatemic rickets | 20 (55 segments) | 55 segmental deformities (20 femora, 35 tibiae) from 20 patients were examined retrospectively. Distraction osteogenesis was used in 28 segments and acute deformity correction in 27. External fixation was applied in 24 segments, intramedullary nailing in six, and external fixation and intramedullary nailing in 25. Recurrent deformity or refracture occurred in 10 of 21 segments with distraction osteogenesis by external fixation only, 4 of 6 with acute correction by intramedullary nailing, and 1 of 25 with distraction osteogenesis or acute correction by external fixation and intramedullary nailing. External fixation and intramedullary nailing can be recommended to prevent complications during or after deformity correction in hypophosphatemic rickets |
Eralp et al. | J Bone Joint Br (2004) | A correction of windswept deformity by fixator assisted nailing | 2 (7 segments) | Seven segments in two patients with vitamin D related metabolic bone disease were treated by fixator-assisted nailing technique. All deformities were accurately corrected and there was no consolidation problem at the osteotomy sites. The total treatment time was found less than with other techniques |
Stanitski | Clin Orthop Relat Res (1994) | Treatment of deformity secondary to metabolic bone disease with the Ilizarov technique | 8 (18 segments) | Complications were limited to several pin-tract infections and mild translational deformity in two patients. Healing index averaged approximately twice that seen in pediatric femoral lengthening and was 25 % greater than for patients undergoing tibial lengthening. The lack of implants requiring removal, modularity, and reasonable treatment time make this technique an attractive alternative to conventional osteotomy for management of limb-length deformity associated with metabolic bone disease |
Recurrent deformity is a common sequela of osteotomies in patients with hypophosphatemic rickets [4, 12, 14] (Fig. 15.10). As expected, younger patients have a higher risk of recurrence. Therefore, milder deformities should not be operated early in the infancy. At this stage guided growth by hemiepiphyseodesis is an advisable alternative [17]. Only when gait is compromised by a thrust, or symptoms such as pain start, a corrective osteotomy should be done.


Fig. 15.10
Note the recurrence of the deformities in a patient despite the intramedullary nails
Short stature is also noted amongst children with hypophosphatemic rickets. The common indication for long bone lengthening is a shortening of the entire or segment of limb in one or both legs [11]. The procedure can be performed by monolateral or circular external fixators or by lengthening over an intramedullary nail (LON) (Fig. 15.11) [12]. The application of flexible intramedullary nails in limb lengthening for children is also an alternative with multiple advantages [18]. This technique also respects the bone biology that is essential during the limb lengthening.


Fig. 15.11
Following deformity correction (fixator assisted nailing) lengthening over nail was performed at the femur
Author’s Preferred Method, Tips and Tricks
The pathological change caused by hypophosphatemic rickets occurs very close to the growth plate, often leading to juxta-articular multiplanar deformities and severe malalignment. Preoperative assessment usually reveals multiple centers of rotation of angulation (CORA) (Fig. 15.12); thus several osteotomies may be required to fully correct the multiapical deformities. Many methods of treatment have been described. The most common involve acute or gradual correction, using either circular or monolateral external fixators, which can secure accurate correction of the deformity and address the limb-length discrepancy. However, these methods are uncomfortable for the patient, especially when both legs are involved. There are further disadvantages, such as the need for daily adjustments, weekly follow-ups, a high rate of pin-track infection, and a long duration of external fixation.


Fig. 15.12




Long sagittal bowing deformity at the femur: note there are multiple centers of rotation in these type of deformities
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


