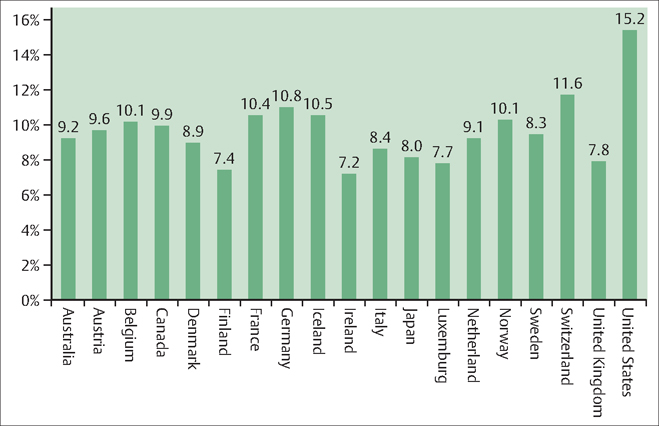
54 Medical Economics and Social Issues Robert L. Barbieri There is a strong relationship between population health and economic growth and stability. In general, countries with strong, growing, and stable economies have better overall population health than do poor countries. In general within a country, wealthy individuals and families have better health and more access to high quality health care than do poor individuals and families. The strong relationship between health and economic prosperity both at the global and individual levels is a major challenge to clinicians. As part of their professional commitment, clinicians need to be engaged in trying to provide equitable access to health care for all members of their community. Two key links between health and economic growth are longevity and small family size. As the health of a population improves longevity increases. As longevity increases the educational and skill level of members of the society increases, in turn increasing their economic productivity. OB/GYN practitioners help to ensure the birth of healthy children, thereby initiating the path to a long and healthy life. In general, as family size decreases, investment in each child increases, resulting in better educated and more economically productive adults. According to one report, as the growth rate of the population of a country increases by 1%, the rate of growth of domestic product decreases by 0.4% (Bloom DE, Williamson J. Demographic transitions and economic miracles in emerging Asia. World Bank Econ Rev 1998;12:419–455). OB/GYN practitioners play a key role in helping families achieve their optimal size. In many developed countries, controlling the rate of growth of health care costs and ensuring high quality are critical health economics issues. As a thought experiment, it is not sustainable for the health care costs to grow at a rate of 10% per year and gross domestic product (GDP) to grow at a rate of 4% per year. Eventually the entire GDP would be spent on health care. The amount of gross domestic product (GDP) spent on health care varies substantially among developed countries (Fig. 54.1). Most developed countries are taking multiple steps to attempt to control the rate of rise of health care costs including: Fig. 54.1 Total health care spending as a percentage of gross domestic product in 2003. Reducing health care waste can take many forms, including avoiding unnecessary tests and procedures. Toyota engineers developed the concept of “lean production systems,” which is the never-ending pursuit of perfection by eliminating unnecessary steps and waste in the production process. In health care, common causes of waste include: Using the lean production method, Toyota engineers have achieved high levels of reliability, quality, and cost-control. Health systems are in the process of systematically redesigning work using these proven methods. In the United States a 90-day supply of a generic osteoporosis medication, alendronate, costs $10. A 90-day supply of the same brand-name product costs in the range of $200. The widespread use of generic medications has the potential to reduce overall health care costs. A modest concern is that the use of generics will reduce the money available to pharmaceutical firms for research and development of new drugs. Many new drugs and technologies are expensive but offer only a modest improvement in health outcomes. Most health insurers have evidence-based processes for trying to limit the introduction of new technologies and procedures that are supported by limited evidence. For example, some insurers require the publication of three high-quality clinical trials that demonstrate the clinical utility of a new technology or procedure before they will reimburse for the innovative technology or new procedure. A modest disadvantage of this approach is that it can delay the access of patients to promising, but as yet unproven, treatments. An electronic health record opens opportunities for health savings through the use of decision-support software to encourage the use of generic medications, reduce the use of unnecessary imaging studies, avoid duplication of testing, and ensure timely provision of preventive care services such as vaccinations. Key concerns with an electronic health record include the protection of the patient’s privacy and provisions to “hide” especially sensitive medical information. It is estimated that 10% of patients create 70% of all health care costs. Many of these patients have chronic conditions such as diabetes, emphysema, and heart failure, which may be best managed in an outpatient setting by midlevel providers such as nurse practitioners and physician assistants. By proactively ensuring patients are incorporating healthy behaviors (such as taking their medicines) in their daily activities, expensive hospitalizations can be reduced. A substantial percentage of all health care expenditure occurs in the last year of life. Wide geographic variation exists in the total value of health care interventions provided in the last year of life. This suggests that regional culture and practice patterns influence the intensity of health care provided in this period. Reducing the variation in health care expenditures in the last year of life will likely reduce the rate of growth of health care costs. Most economists believe that when analyzed in a narrow context, the best approach to reducing administrative costs in the health care system is to move to a single-payor system such as the Medicare system for all citizens. A major concern with this cost-saving intervention is that it is likely that the range of choices for clinicians and patients will be reduced and innovation might be slowed. Government control of all health care choices is likely to result in some limitations of benefits, reduction in service quality for some citizens, and potential delays in care. Prevention activities such as vaccinations improve population health but may not dramatically reduce health care costs in most developed countries that are already reaping the benefits of prevention activities. Primary prevention activities that focus on healthy life styles, such as maintaining an optimal body mass index, have not received sufficient attention and are likely to reduce the costs of major diseases such as diabetes and heart disease. Many preventive services that have been documented to have a positive health and economic impact are not routinely provided by clinicians (Table 54.1).
Population Health Promotes Economic Growth and Stability
Health Economics Issues in Developed Countries
Reducing Waste: Lean Engineering
Generic Medications
Effectiveness Review of All New Drugs and Technology
Interoperable National Health Record
Long-Term Management of Chronic Health Conditions
Reducing the Use of Expensive Interventions in the Last Weeks of Life
Reducing Administrative Costs of Managing Health Insurance
Increasing Primary Prevention Activities



