Management of Esophageal Foreign Bodies
Jeff E. Schunk
Nanette C. Dudley
Introduction
Young children often swallow foreign bodies because of their inquisitive nature and propensity for pica (1). Esophageal impaction of these objects occurs frequently, and removal is often necessary to avoid serious complications (2,3,4,5,6,7,8,9). Most esophageal foreign bodies are blunt or smooth, and coins are the most common (1,10,11). Other esophageal foreign bodies include bones, meat, toys, and, less commonly, sharp objects. Esophageal foreign bodies may occur at any age, although they are found more commonly in children aged 6 months to 6 years.
A variety of techniques and settings may be used for esophageal foreign body removal, depending on the type of physician specialist who performs the procedure. Local referral patterns, the nature of the foreign body, the duration and extent of symptoms, and the physician’s familiarity with various techniques will determine the method of choice. Removal methods include endoscopy (10,11,12) or the use of Magill forceps (13,14) in the operating room, flexible endoscopy in the outpatient setting (15), the Foley catheter technique (16,17,18), advancement with a Bougie dilator (19,20), and a newer method called the “penny pincher” (21).
Anatomy and Physiology
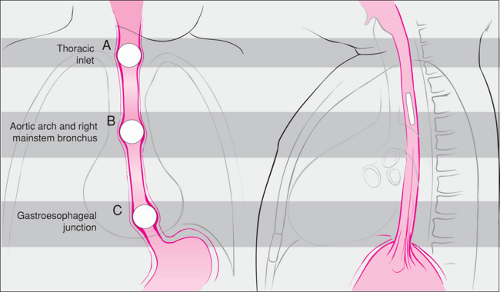
Esophageal foreign bodies occur at predictable sites of normal anatomic narrowing (10,11). These sites include the thoracic inlet (cricopharyngeus), the level of the right mainstem bronchus-aortic arch, and the gastroesophageal junction (lower esophageal sphincter) (Fig. 83.1): (10,11,22,23). Children with underlying esophageal pathology are predisposed to foreign body impaction at sites of pathologic narrowing that may not correspond to the typical sites.
It is generally recommended that all esophageal foreign bodies should be removed. Local reaction, both inflammatory and muscular, may adversely affect esophageal motility and can lead to adjacent airway narrowing. Although esophageal perforation is most likely to occur from an impacted sharp object (24), complications also have been reported from impacted blunt objects. These include esophageal perforation (4), tracheoesophageal fistula (5), esophageal-aortic fistula (8), vocal cord paralysis (9), brain abscess (7), and upper airway compromise from local reaction (25). With the exception of disc (“button”) batteries (26,27,28), no serious complications have been reported from blunt esophageal foreign bodies impacted for less than a few days. Removal of an esophageal foreign body
typically results in rapid return to normal esophageal function and relief of associated symptoms.
typically results in rapid return to normal esophageal function and relief of associated symptoms.
Indications
Patients with esophageal foreign bodies often present with a foreign body sensation, pain, or symptoms of impaired esophageal function such as vomiting, drooling, and dysphagia. Airway compromise with stridor or wheezing also may occur. However, many children with esophageal foreign bodies have no symptoms. In two emergency department (ED) studies, 30% (22) and 44% (29) of children with a coin in the esophagus were asymptomatic. Patients with asymptomatic esophageal coins of less than 24 hours duration can be observed for spontaneous passage, as this will occur about 25% of the time (30,31,32).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree