Management of Cerebral Edema and Elevated Intracranial Pressure
Steven G. Kernie
Most forms of acute head injury increase the volume of the intracranial contents. Cerebral edema, hemorrhage, acute hydrocephalus, or rapidly growing tumors all result in intracranial hypertension (see Chapter 104 and Table 104-5). The relationship between the volume increase and the rise in intracranial pressure is not linear. Small volumes can be accommodated either by stretch, if the cranial sutures are still open, or by displacement of cerebrospinal fluid (CSF) into the spinal canal (this is why in most forms of intracranial hypertension, with the notable exception of hydrocephalus, the ventricles appear small). To a lesser extent, the blood contained at any time in the cerebral vessels, especially the cerebral veins, diminishes. As the volume increase produced by the injury becomes larger, however, the pressure increases more rapidly, a circumstance that can be described as a volume-dependent decrease in the compliance of the cranium. Any additional volume causes a disproportionate elevation in intracranial pressure.
The most immediate and dangerous consequence of increased intracranial pressure is a reduction in cerebral blood flow. Cerebral herniation (see Chapter 104) tends to be a later development. In most organs, blood flow is directly proportional to the difference between arterial and venous pressure (the perfusion pressure) and is inversely proportional to the resistance of the organ’s vascular bed. Some organs, such as the heart and the brain, regulate their vascular tone (and thus their vascular resistance) to maintain constant blood flow over a wide range of perfusion pressures appropriate for age (autoregulation). Below or above this autoregulation range, blood flow changes in proportion to perfusion pressure. (Other organs, such as the intestine and the skin, have their flow regulated by neural and humoral inputs in response to a variety of physiological circumstances, sometimes without change in blood pressure.)
The cranial enclosure introduces a new variable for consideration. The outside surface of the cerebral blood vessels is exposed to intracranial pressure. If this pressure exceeds venous pressure, then the effective perfusion pressure is the difference between arterial and intracranial pressure, the venous pressure becoming irrelevant in defining blood flow (just as the height of a waterfall is irrelevant in determining the flow of the river). Intracranial hypertension can reduce cerebral perfusion pressure below the autoregulation range of the cerebral blood vessels, resulting in cerebral ischemia.
Cerebrospinal fluid production and subsequent absorption is, like cerebral blood flow, quite dynamic. The choroid plexus accounts for at least 70% of the brain’s production of cerebrospinal fluid, and the transependymal movement of fluid from the brain parenchyma to the ventricular system accounts for the rest. The average volume of cerebrospinal fluid in children ages 4 to 13 years is 90 mL, and the rate of formation is approximately 500 mL per day, resulting in an hourly turnover of about 14% of the total volume.
The rate of production remains fairly constant and declines only slightly with increased intracranial pressure, but the rate of absorption increases linearly as the pressure exceeds approximately 15 mm Hg to 40 mm Hg to where the rate of absorption is triple the rate of production.2
CEREBRAL EDEMA
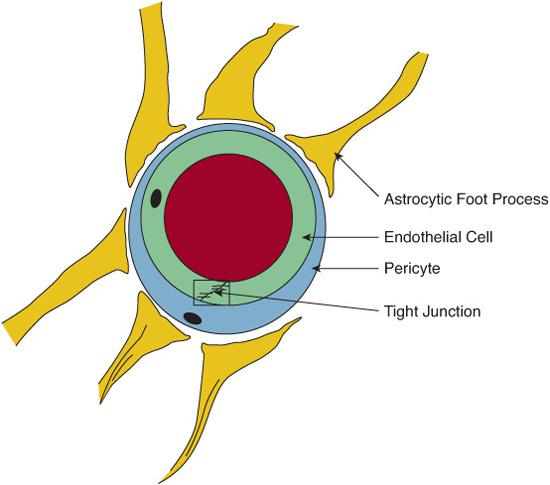
The brain has specialized systems to regulate traffic of water and solutes in and out of the blood vessels. Brain endothelial cells, for instance, differ from those in other organs by their lack of fenestrations and the presence of an extensive patchwork of tight junctions. In addition, the capillary basement membranes, the pericytes embedded within this membrane, and aquaporin-4 expressing astrocytic end-feet3 form a sheath around every blood vessel, creating a very selective membrane known as the blood-brain barrier (Fig. 111-1). This barrier provides an ideal system for selective transfer of nutrients and metabolic products while protecting the brain cells from exposure to potentially injurious circulating molecules and from excessive accumulation of water (cerebral edema).
Based on the operative mechanisms, cerebral edema is classified as vasogenic, cytotoxic, or interstitial. Vasogenic edema is caused by increased capillary permeability and disruption of the blood-brain barrier following injury. It is seen with brain tumors, abscesses, hemorrhage, and trauma. Cytotoxic edema results from alterations in the membrane functions of neurons, glia, and endothelial cells such as those that occur after hypoxic-ischemic insults, infection, and trauma. Interstitial edema occurs when the usual flow of transependymal fluid to the ventricular system is altered or impeded.2 This happens when cerebrospinal fluid absorption is blocked or when production is increased beyond the brain’s ability to reabsorb it. In most clinical situations, cerebral edema results from a combination of more than one of these mechanisms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


