Management of Abortion
Eva Lathrop
Carrie Cwiak
DEFINITIONS
Anembryonic pregnancy—A pregnancy in which trophoblast develops without development of embryonic tissue.
Dilation and evacuation—A surgical technique for pregnancies beyond 12 to 14 weeks gestation, utilizing advanced cervical dilation and evacuation of fetus and placenta via suction and forceps.
Early pregnancy loss—Loss of a pregnancy before 24 weeks gestation.
Electric vacuum aspiration—A surgical technique for pregnancies less than 12 to 14 weeks gestation, utilizing cervical dilation and aspiration of the fetus and placenta via suction.
Embryonic death—The finding of no cardiac activity in an embryo at least 5 mm and up to 15 mm (8 weeks) in length.
Fetal death—The finding of no cardiac activity in a fetus over 8 weeks (15 mm) gestation.
Incomplete abortion—Clinical and ultrasonic evidence of retained tissue in the uterus after an early pregnancy loss or induced abortion.
Induced abortion—Medical or surgical termination of an ongoing pregnancy.
Inevitable abortion—Dilation of the cervix without passage of pregnancy-related tissue.
Manual vacuum aspiration—Aspiration of the fetus and placenta via suction generated by a handheld syringe.
Missed abortion—Clinical or ultrasonic evidence of a nonviable pregnancy without cervical dilation or passage of pregnancy-related tissue.
The management of abortion remains a principal focus of gynecology. In the United States, each year, more than 1 million pregnancy losses occur and more than 1 million induced abortions are performed. With minimal modification, the surgical management of early pregnancy loss (EPL) is the same as for induced abortion, making uterine aspiration one of the most frequently performed operations in gynecology and one of the most thoroughly studied. In addition, the medical techniques effective for induced abortion are typically as effective for EPL. This chapter focuses on the surgical management of abortion but also summarizes other treatment options. It reviews the incidence, risk factors, preoperative assessment, and evidence-based treatment for spontaneous, illegal, and legal abortion. Readers should keep in mind that abortion technology is rapidly evolving, and new protocols may supplant those described here.
EARLY PREGNANCY LOSS
Incidence
Pregnancy loss is a common reproductive outcome. National Vital Statistics estimated that 1,118,000 total pregnancy losses occurred in 2008 in the United States (17% of all pregnancies). The incidence of EPL is dependent on the definitions utilized for EPL and for recognized pregnancy but is typically quoted as between 10% and 15% of all pregnancies. The contemporary definition for EPL is the loss of a pregnancy before 24 weeks estimated gestational age (EGA), recognizing the typical limits of fetal viability when resources are available. The greatest percentage—over 85%—of EPL occurs before 13 weeks gestation.
Fetal death is defined as no cardiac activity in a fetus over 8 weeks gestation and is uncommon after the first trimester. The U.S. National Vital Statistics System utilizes the World Health Organization (WHO) categories for fetal death: early (<20 weeks EGA), intermediate (20 to 28 weeks), and late (28 weeks or more), the latter corresponding to the international definition for stillbirth. The 2006 data from the U.S. National Center for Health Statistics report a fetal death rate of 6.05 per 1,000 live births. The incidence of fetal death decreases with increasing gestational age. Of the fetal deaths over 20 weeks in 2006, greater than 50% occurred between 20 and 27 weeks, with over one third occurring between 20 and 23 weeks. These categories overlap with the definition commonly used for EPL. In addition, individual states vary in the gestational ages at which they begin collecting data on pregnancy loss or fetal death. However, determining the upper limit by which to define EPL may be more an argument of necessity for statistical records than for clinical practice.
The true incidence of EPL is also uncertain because of the difficulty in recognizing early conceptions and losses. When Wilcox and associates monitored daily urinary β-human chorionic gonadotropin (β-hCG) in the 1980s, they found that 31% of pregnancies resulted in spontaneous abortion after implantation, but approximately 70% of these—22% of all losses—were not yet clinically identified. Wang and colleagues published data in 2003 in which 8% of all conceptions in their study were recognized pregnancies followed by spontaneous loss. Twenty-six percent of all conceptions in that study were losses before knowledge of the pregnancy. The ability to confirm pregnancy at an earlier EGA has significantly improved with the clinical use of highly sensitive urine pregnancy tests that can detect levels as low as 15 mIU/mL or 10 days after the last menstrual period. However, home pregnancy tests remain highly variable and can require levels as high as 100 mIU/mL before testing positive. Therefore, a significant amount of EPL may still be unreported.
Terminology
EPL has been previously referred to as early pregnancy failure and spontaneous abortion. In addition to sensitive urine pregnancy tests, the availability of transvaginal ultrasound has enabled the diagnosis of EPL at very early EGAs. Terminology
has thus evolved to reflect the pathophysiology of the loss. Anembryonic pregnancy occurs when the trophoblast develops in the uterus without subsequent development of embryonic tissue. The diagnosis is confirmed by the ultrasonic finding of no yolk sac or embryonic pole and intrauterine gestational sac with mean sac diameter (MSD) of 16 mm or more, though utilizing an MSD cutoff of 20 mm in clinical practice can increase the specificity of diagnosis. Embryonic death is diagnosed by the ultrasound finding of no cardiac activity in an embryo at least 5 mm and up to 15 mm (8 weeks) in length. Fetal death is diagnosed by the ultrasound finding of no cardiac activity in a fetus over 8 weeks (15 mm) gestation. The first trimester of pregnancy is generally defined as either the first 12 or 14 weeks of pregnancy.
has thus evolved to reflect the pathophysiology of the loss. Anembryonic pregnancy occurs when the trophoblast develops in the uterus without subsequent development of embryonic tissue. The diagnosis is confirmed by the ultrasonic finding of no yolk sac or embryonic pole and intrauterine gestational sac with mean sac diameter (MSD) of 16 mm or more, though utilizing an MSD cutoff of 20 mm in clinical practice can increase the specificity of diagnosis. Embryonic death is diagnosed by the ultrasound finding of no cardiac activity in an embryo at least 5 mm and up to 15 mm (8 weeks) in length. Fetal death is diagnosed by the ultrasound finding of no cardiac activity in a fetus over 8 weeks (15 mm) gestation. The first trimester of pregnancy is generally defined as either the first 12 or 14 weeks of pregnancy.
Once the diagnosis of a nonviable pregnancy has been made by abnormal trend in β-hCG or ultrasound, then terminology is also used to describe the clinical presentation of EPL. Missed abortion refers to a nonviable pregnancy in which dilation of the cervix and passage of pregnancy-related tissue have not yet occurred. Although missed abortion was associated in the past with complications from delayed diagnosis and retained products of conception, currently, it is often made when a patient is asymptomatic. Inevitable abortion can be considered the next stage in a continual process, in which a woman has a dilated cervix but passage of tissue has not yet occurred. Incomplete abortion refers to EPL in which some, but not all, of the tissue has passed. As a clinical definition, incomplete abortion refers to a woman who is symptomatic with abnormal bleeding, pain, or signs of infection due to retained tissue in the uterus. However, after passage of the gestational sac, it can be difficult to determine if the remaining tissue in the uterus is clinically significant in the woman with mild to no symptoms.
Risk Factors
EPL has several important risk factors. Over two thirds of EPL prior to 12 weeks EGA are associated with chromosomal anomalies, the most frequent of which are autosomal trisomies, followed by polyploidies, and then monosomy X. The earlier the gestational age at loss, the higher the frequency of chromosomal anomaly. Almost all anomalies, including some that would not appear to handicap survival (such as cleft lip), increase the likelihood of EPL. These anomalies are typically the result of random mutations, though a predisposition due to a balanced translocation or family history of a genetic defect can increase maternal or paternal risk.
Demographic details point to some other nonmodifiable risk factors. In a large study published by Nybo Anderson and colleagues, the rates of EPL increased with maternal age. Women aged 20 to 30 years, 35 years, 40 years, and 45 years saw a 9% to 17%, 20%, 40%, and 80% EPL rate, respectively. Previous studies reported an increase from 12% at ages less than 20 to 26% at age 40. Likewise, the risk increases with advancing paternal age. Race also plays a role. At each stage of pregnancy, black and Hispanic women in the United States have higher rates of pregnancy loss overall and of fetal death than do white women.
Independent of the effect of age, the risk of EPL changes with previous pregnancy history. Increasing rates are seen with increasing gravidity or parity. Personal history of one or more spontaneous losses increases the risk of recurrence. This effect is seen at all gestational ages. The risk of EPL was reported to increase with each documented loss in one study, increasing from 20% after one loss to 43% after three or more. Alternatively, the risk of EPL is lower for a woman who has not had a previous pregnancy or whose last pregnancy was successful. The length of the interval between pregnancies appears to have little impact.
Modifiable risk factors for EPL have also been identified. Overall, poor diet and obesity have each been associated with increased risk of EPL. Smoking may increase the risk of EPL. Because smoking is not teratogenic, its effect on spontaneous abortion rates may be via abortion of normal conceptuses. In one study, the risk of loss doubled; in other studies, the increase in risk was slight. Recent studies have not confirmed this increased risk. Alcohol consumption is associated with EPL as well as teratogenicity. The effects of alcohol on EPL risk appear to be greatest for those whose alcohol consumption is greater. Additionally, the risk appears to be greater with increased intake in the earlier gestational ages. Alcohol consumption as a teratogen has a dose-dependent effect and can result in mental retardation, microcephaly, midface hypoplasia, and renal and cardiac defects. Caffeine intake has been evaluated in many studies regarding EPL. Several studies had suggested an increased risk for spontaneous abortion in women who drank greater than 500 mg—or the equivalence of 5 cups—of coffee per day. However, a systematic review by Signorello and McLaughlin indicates that there is insufficient evidence supporting a causal relationship.
Certain maternal comorbidities are associated with an increased risk of EPL. Women with poorly controlled diabetes have higher levels of pregnancy loss as well as congenital anomalies. Increased rates of EPL are seen in women with other endocrine imbalances such as thyroid disease and polycystic ovarian syndrome, autoimmune disease, hypercoagulable states such as antiphospholipid antibody syndrome and thrombophilias, and chronic infections.
Cervical incompetence can lead to EPL. Cervical incompetence is more accurately defined as premature cervical dilation in midtrimester of pregnancy without uterine contractions, but the diagnosis is often made retrospectively in the women with unexplained repetitive midtrimester EPL without labor. Incidence rates range from 0.05 to 1 per 100 pregnancies. Though cervical loop electrocautery excision procedure is associated with EPL, data are otherwise lacking to confirm or refute other potential causes, such as previous cervical laceration or excessive mechanical dilation; the occurrence of this condition in primigravidas suggests alternative causes. These may include associated uterine anomalies, prenatal exposure to diethylstilbestrol, or abnormal histology of the cervix. In addition, premature cervical dilation without labor may be inheritable.
The presence of uterine anomalies can lead to EPL as well. Uterine synechiae, or Asherman syndrome, may permit insufficient surface area to support a pregnancy and lead to spontaneous loss. Uterine septa and abnormalities of müllerian fusion can also result in pregnancy loss if the pregnancy implants on the septum and outgrows its blood supply. Although no effect is seen in the first trimester, the incidence of EPL due to uterine anomalies after 13 weeks gestation may be 20% to 25%. Leiomyomata, specifically submucosal or large myomata, can interfere with implantation and make sustained pregnancy difficult.
Prevention
It is largely unknown how to prevent EPL. A meta-analysis of four studies suggests that oral or vaginal progesterone can prevent fetal loss when given to women with threatened abortion (bleeding, but with a viable fetus). Because the studies were small and of poor quality, further study is warranted before this can be accepted as proven therapy. One study by Mills and colleagues indicated that women with diabetes with excellent glycemic control early in pregnancy had the same rate of spontaneous abortion as did controls. Optimization of maternal health and avoidance of substances may be advisable for all women to prevent EPL as well as encourage maternal
well-being. However, Cochrane reviews of randomized trials have found insufficient evidence for EPL prevention from vitamin supplementation, Chinese herbal medicine, bed rest, HCG, or beta-agonists.
well-being. However, Cochrane reviews of randomized trials have found insufficient evidence for EPL prevention from vitamin supplementation, Chinese herbal medicine, bed rest, HCG, or beta-agonists.
Surgery may benefit some women with cervical incompetence or uterine abnormalities. For cervical incompetence, vaginal or abdominal cerclage can be performed, and those techniques are described elsewhere in this text. A Cochrane review of randomized trials concluded that cerclage reduces preterm delivery, though not perinatal mortality, in women at high risk for recurrent preterm delivery. Benefits for lowrisk women are unproven. If uterine synechiae are diagnosed, hysteroscopic lysis of adhesions is recommended. Women with müllerian anomalies who experience EPL at 13 weeks gestation or later may be candidates for reconstructive operations, described elsewhere in this text. Removal of uterine fibroids, if performed only because of infertility, may help little; the effect of myomectomy on pregnancy loss rates is unknown.
Evaluation
A majority of the time, viability concerns in early pregnancy are preceded by vaginal bleeding. Bleeding in early pregnancy is common, reported in up to 25% of early pregnancies, and ensuring appropriate evaluation and management is essential for women’s health. In addition to the history and physical exam, ultrasonography and serial measurement of β-hCG are important diagnostic tools to differentiate threatened, incomplete, and complete abortion. These are also important in the diagnosis of ectopic pregnancy, as an intrauterine pregnancy identified on ultrasound virtually excludes the diagnosis of ectopic pregnancy.
The average rise of β-hCG is 100% over 48 hours, but the lower limit of β-hCG rise in normal pregnancies has been shown to be as low as 53% in 48 hours. Conversely, once trophoblastic development has stopped, β-hCG clears the serum at about the same rate of 100% in 2 days. β-hCG serum levels clear faster after EPL than after induced abortion, though levels can similarly be seen to plateau toward the end of clearance. Therefore, depending on the level of β-hCG at the time of EPL, β-hCG may remain positive for up to 8 weeks thereafter.
Although persistent β-hCG levels might alert the provider to abnormal trophoblastic tissue and an increasing trend to a continuing or new pregnancy, a single β-hCG level cannot assist in diagnosis of retained products of conception because if trophoblastic development has been interrupted, whether by EPL or induced abortion, then a positive β-hCG may be present, trending down, without retention of a clinically significant amount of tissue. Conversely, clinically significant but nonviable, retained tissue can be present with a negative β-hCG value since trophoblastic development is no longer occurring.
Increasing use of vaginal ultrasound has improved diagnostic validity, especially at early gestational ages. When an embryo is visible, management is straightforward. However, most abnormal pregnancies stop developing before an embryo is visible by sonography. The discriminatory zone is the β-hCG serum level at which an intrauterine gestational sac can be seen via ultrasound for a viable pregnancy. The discriminatory zone for vaginal ultrasound can range from 1,500 to 2,000 mIU/mL depending on laboratory and sonographic resources and has a specificity of 95% to 100%. Two additional sonographic findings have high specificity: a gestation sac at least 25 mm in mean diameter without an embryo and distorted sac shape. On the other hand, the sensitivity of these criteria appears to be low. Presence of fetal heart activity is more accurate in predicting EPL than are morphologic criteria. Several reports concur that once fetal cardiac activity is documented by ultrasonography in the first 12 weeks of pregnancy, the likelihood of subsequent fetal loss is low: about 2% to 4.5%. This does not hold true, however, for women older than age 35 or those with a history of recurrent pregnancy loss. Furthermore, studies have noted that fetal heart rates less than 100 beats per minute in the embryonic stage are associated with a significantly lower survival rate than those with normal fetal heart rates.
Given the lack of medical need for intervention in the majority of cases of EPL, clinicians need not act on a single abnormal clinical finding in a desired pregnancy, such as a falling β-hCG level or failure to observe fetal cardiac activity. Following the β-hCG trend can establish the diagnosis of normal versus abnormal (EPL or ectopic) pregnancy. Alternatively, repeating the ultrasound at an appropriate interval improves the diagnostic accuracy of this procedure.
The traditional approach to threatened abortion, characterized by uterine bleeding without cervical dilation or expulsion of tissue and demonstration of a potentially viable fetus, has been watchful waiting. The chance of EPL after threatened abortion can be as high as 50%. Reliably predicting fetal outcomes in such situations is not yet possible, and serial β-hCG levels or ultrasound examinations may be necessary to determine viability of a pregnancy that is not actively being passed.
In the case of missed abortion and in the absence of gestational trophoblastic disease, little to no trophoblastic tissue proliferation occurs after the pregnancy loss, and so, the current uterine size or ultrasound findings typically indicate the EGA at the time of loss. The discrepancy between current EGA and expected EGA based on last menstrual period or previous normal ultrasound suggests how long ago the loss actually occurred and, in extreme cases, may suggest whether infection, hemorrhage, and/or disseminated intravascular coagulation (DIC) is likely. Missed abortion in which the pregnancy is retained for 8 weeks or more has been associated with hemorrhage and DIC.
Diagnosis of incomplete abortion has come full circle from a basis of clinical symptoms, to detection of retained tissue in the uterus on ultrasound, back to clinical diagnosis. Harwood et al. noted that the endometrial thickness after EPL was as high as 29 mm in asymptomatic women. Similar studies have concluded that no cutoff value could predict which patients would require surgical management after medical or expectant management of EPL. Follow-up studies after early medical and surgical abortion have found similar results, leading to the conclusion that the thickness of the endometrium after completion of a pregnancy has a wide range of normal variability. Therefore, the diagnosis of incomplete abortion is typically made on clinical grounds and then confirmed by ultrasound findings. In other words, a thickened endometrium in an asymptomatic woman need not be acted upon.
Management
After confirmation of EPL, the first, and perhaps most important, step is to counsel the women and her partner. Helping the couple to grieve appropriately can minimize psychological sequelae from what can be a devastating loss. Subsequent clinical management is largely discretionary. Historically, surgical management was recommended for EPL due to a higher incidence of infectious and bleeding complications associated with delayed diagnosis, or the misclassification of illegal abortion as incomplete abortion. However, for women with missed, inevitable, or incomplete abortion, several options are available. Patient preference should generally determine the management as long as there is hemodynamic stability and absence of infection.
Many women faced with the disappointing diagnosis of EPL prefer prompt surgical evacuation. Surgical management of EPL is dependent upon EGA determined by current uterine examination and ultrasound and upon clinical diagnosis. EPL up to 12 to 14 weeks EGA should be performed by uterine aspiration, via either manual vacuum aspiration (MVA) or electric vacuum aspiration. As with induced abortion, sharp curettage is no longer standard of care for EPL as it is associated with more blood loss, postoperative hemorrhage, anemia, pain, and operative time compared to manual or electric aspiration. The safe limits of EGA for uterine aspiration are dependent on clinician experience and available equipment, but it can be safely performed up to 14 weeks EGA if the appropriate-sized cannula is available for use with either manual syringe or electric vacuum. As with induced abortion, cannula size in mm should typically correspond to uterine size in weeks gestation, plus or minus 1 mm in cannula size. Utilizing a cannula that is too small can result in increased operative time, bleeding, and risk of retained products, especially in the case of EPL that has occurred several weeks before. Although nonviable fetal tissue frequently softens over time, placental and trophoblastic tissue can become indurated and less likely to pass through a too-small cannula. For missed abortion, the guidelines for preoperative cervical preparation for induced abortion can be followed (see “Preoperative Cervical Preparation”). For inevitable and incomplete abortion, minimal to no cervical dilation may be necessary if the cervix is already dilated enough to admit the correct-sized cannula. The technique of uterine aspiration, via manual or electric vacuum, is identical to that for induced abortion (see “Manual Vacuum Aspiration” and “Electric Vacuum Aspiration”).
Site of uterine aspiration may depend on time of day, staff and equipment resources available, local protocols for sedation, and clinical presentation. The syringe used for MVA is portable, inexpensive, and convenient for outpatient use. The technique is described in detail later in this chapter. Blumenthal and Remsburg found that for surgical management of EPL, MVA in the clinic or emergency room was more cost-effective than was uterine aspiration in an operating room. Development of a protocol for MVA in an office or emergency room can decrease patient cost and increase patient satisfaction. Many women prefer in-office MVA for surgical management of EPL. As with other in-office procedures, patients must be clinically stable, without multiple comorbidities, and otherwise appropriate candidates for in-office sedation and surgical management. Clinicians who are contemplating provision of in-office MVA may be more comfortable initially offering it to patients with incomplete abortion or at an early EGA and then increasing the range as their comfort level allows.
Dependent on the skill of the physician, EPL past 12 to 14 weeks EGA can also be managed surgically, via dilation and evacuation (D&E). For women with a closed cervix, preoperative cervical preparation is essential. The guidelines for cervical preparation for induced abortion can be followed for fetal loss in the second trimester as well. For D&E, larger cannulas are available for use with electric vacuum aspiration. But for an EGA larger than the size of the suction cannula available, Bierer forceps should be utilized for safe evacuation of fetus and placenta. Even with retained placenta after second- or third-trimester loss or delivery, use of Bierer forceps for evacuation is safer and more efficient than the traditional horseshoe curette. The technique of D&E for fetal loss or retained placenta is identical to that for induced abortion (see “Dilation and Evacuation”).
Antibiotics should be administered as soon as possible for women with infectious complications of EPL, and timely uterine evacuation is recommended. However, perioperative antibiotic prophylaxis has not been found to decrease infection when used for incomplete abortion. It is unknown whether antibiotic prophylaxis is effective in other presentations of EPL like inevitable or missed abortion.
There are no studies that specifically address venous thromboembolism (VTE) associated with surgical management of EPL or induced abortion. The guidelines for VTE prophylaxis for gynecologic surgery may be followed in either situation (see “Venous Thromboembolism Prophylaxis”).
Analgesia should be used and can be provided via paracervical anesthesia, sedation, or combination of the two. Sedation is more likely to be associated with postoperative nausea and vomiting than paracervical block (PCB) alone. For sedation regimens, anxiolytic and narcotic medications are effective, whether via oral or intravenous administration. For the surgical management of EPL, randomized trials have concluded that adding an NSAID to a narcotic sedation regimen provides no additional benefit. And in comparison to sedation, general anesthesia provided no additional relief from postoperative pain but was associated with higher patient satisfaction. Whether this is due to the patient’s emotional state or her perception of increased pain relief with general anesthesia, preoperative patient counseling may increase satisfaction with sedation. Any benefit must be balanced against the potential complications of induction of anesthesia in addition to the fact that anesthesia is associated with more need for blood transfusion. The WHO Safe Abortion Guidelines recommend that general anesthesia not be routinely used first line for management of abortion, suggesting that the risks of general anesthesia outweigh the benefits in most cases.
Another option to expedite the expulsion of the pregnancy after EPL is medical management via the prostaglandin analogue, misoprostol. For missed abortion in the first or second trimester, randomized trials have shown that medical management is a safe and effective option for women desiring to avoid surgery. When compared to immediate surgical management, Graziosi et al. noted a cost savings to offering initial misoprostol management followed by surgery if the abortion was not complete by 24 hours. Though patient satisfaction was 58% in each arm of the trial, satisfaction was significantly decreased for women who started misoprostol treatment but eventually required surgical aspiration. When randomized versus placebo, misoprostol resulted in higher rates of complete abortion for fetal loss, at shorter time intervals, without an increase in side effects. Compared to smaller doses, 800 µg of misoprostol is most effective without additional side effects. At this dose, vaginal is similar to oral administration in overall success rates (70% to 90%) but superior in time to successful completion of abortion with less vomiting. Sublingual administration is also similar in efficacy to vaginal but with higher incidence of diarrhea. A randomized, controlled multicenter study by Zhang and colleagues comparing medical management with surgical evacuation found an 84% completion rate by day 8 when vaginal dosing of 800 µg of misoprostol was repeated at 48 hours if passage had not yet occurred, without increase in side effects. In that study, 83% of the woman stated they would recommend the medical treatment to others.
For EPL, only one of two trials has found the addition of mifepristone to the misoprostol regimen increases rates of complete abortion. Laminaria, methotrexate, and the practice of moistening misoprostol prior to vaginal insertion did not increase success. In comparison to other prostaglandins, misoprostol is superior to prostaglandin E but similar to gemeprost. Pain management should be provided and may include NSAIDs or narcotics, with more pain control required at higher EGAs.
For incomplete abortion in the first trimester, medical management with vaginal misoprostol had success rates of 80% to 91% in randomized trials compared to 89% to 100% success with surgical management. As expected, vaginal misoprostol was associated with less use of surgical aspiration overall but higher incidence of unplanned surgery for completion of abortion. Vaginal misoprostol was also associated with more days of bleeding, more need for pain relief, and slightly less patient satisfaction, but no difference in gastrointestinal symptoms, need for blood transfusion, anemia, infection, death, or serious complication. As for missed abortion, vaginal misoprostol provides the same efficacy as oral but with less gastrointestinal side effects. For incomplete abortion, repeated oral doses did not significantly increase the success of abortion completion but did increase side effects. There are no studies comparing medical management to surgical or expectant management for incomplete abortion in the second trimester.
A third option is to await spontaneous expulsion of the pregnancy. Expectant management has been found to have a wide range of success for missed abortion (56% to 98%) and incomplete abortion (52% to 85%) in the first trimester, as defined by no need for surgical intervention. When randomized to surgical management, expectant management was associated with a greater incidence of unplanned surgery for completion of abortion, bleeding, and blood transfusion. However, cost was decreased, and rates of infection, return to normal activity level, and psychological outcome were similar. Rates of success at 6 to 8 weeks were not significantly improved compared to 2 weeks, suggesting that 2 weeks is a reasonable time period to allow complete abortion to occur before intervening. When randomized to misoprostol management, expectant management has similar outcomes for incomplete abortion but inferior efficacy for missed abortion. When categorized by sonographic criteria, Luise et al. noted that 91% of incomplete abortions resolved spontaneously compared with 66% of anembryonic pregnancies. If choosing expectant management, a woman deserves counseling that several days or weeks may pass before resolution and that medical or surgical intervention may ultimately be necessary. Women with a diagnosis of anembryonic pregnancy may be counseled that their success rates may be lower with expectant management. Conversely, women at later gestational ages may not be good candidates for expectant management due to the longer time interval required for expulsion as well as the higher risk of bleeding and need for intervention.
According to a recent meta-analysis, there is insufficient evidence to prescribe one of the above management plans in any given clinical situation. Surgical management is more likely to result in completion than medical management, and medical management is more likely to result in completion than expectant management, but the inverse is true of costs incurred. Patient safety and satisfaction are equivalent with any of these management plans, with the exception that expectant management for EPL in the second trimester has not been studied in randomized trials. Certainly in the face of severe anemia, hemodynamic instability, pain, or infection, surgical evacuation should be performed. Without these, patient preference should be strongly considered. There is no evidence to support the use of antibiotic prophylaxis with medical or expectant management of EPL.
Aftercare for EPL includes surveillance for signs of abnormal grieving reactions or depression, preconception or contraceptive care depending on future fertility desires, and return to regular preventive reproductive care. In the absence of complications, contraception can be initiated immediately, following the same guidelines as for induced abortion (see “Postoperative Care”). Routine follow-up visits are not necessary after uncomplicated management of EPL.
Complications
Early diagnosis of EPL has reduced the risk of complications. In the 1970s, the maternal case fatality rate was estimated to be 4.5 deaths per 100,000 fetal deaths. The most frequent causes of maternal death from fetal death were uterine perforation and coagulopathy. As with induced abortion, advances in care have made mortality from EPL a rare event. The Centers for Disease Control and Prevention (CDC) identified 62 maternal deaths from pregnancy loss in the United States between 1981 and 1991. This represented a case fatality rate of 0.7 deaths per 100,000 pregnancy loss. In 2002, there were two maternal deaths that were due to pregnancy loss. Infection, hemorrhage, and embolism were the leading causes of death. The mortality risk increased with gestational age; women who were older and of minority races also were at increased risk of death.
EPL is a potentially sensitizing event for Rh-negative women. Rates of use of Rh immunoglobulin (RhIG) after EPL are significantly lower than after induced abortion. RhIG candidates at 12 weeks gestation or earlier should receive a 50-µg dose; later abortions mandate a 300-µg dose.
The profound grief that frequently accompanies EPL often receives insufficient attention. Women and men experience the stages of grief. Guilt may be a difficult stage to resolve without help, and counseling plays an important role.
ILLEGAL ABORTION
Incidence
Despite the availability of legal abortions, small numbers of illegal procedures continue to occur in the United States. Estimates of the incidence of illegal abortion in the United States before 1970 or legalization ranged from 200,000 to 1.2 million per year; estimates for the late 1970s ranged from 5,000 to 23,000 per year. More recent estimates are not available; however, a national survey of US abortion patients demonstrated 1.2% of patients reported using misoprostol for self-induction of abortion and 1.4% reported self-inducing with other substances. Illegal abortions occur in large numbers in developing countries, where, according to WHO estimates, close to 50,000 women continue to die of illegal abortion complications each year, and deaths from unsafe abortion account for approximately 13% of all maternal deaths.
Risk Factors
Lack of access to safe, legal abortion is the most important risk factor for having an illegal procedure in the world today. Little is known about characteristics of women in the United States who may still obtain illegal abortions, although in a national survey assessing abortion patients’ reports of previous selfinduction, women who have self-induced live in geographically diverse areas in the United States, the majority are not foreign born, but the level of use overall appears to be higher among foreign-born women.
Techniques
Although a wide variety of illegal abortion methods are used around the world, two methods dominate in the United States: oral abortifacients and intrauterine instrumentation. Orally administered substances include self-obtained misoprostol, turpentine, laundry bleach, large doses of quinine, and various herbs. Intrauterine techniques were less common, more effective, and more dangerous; these ranged from intrauterine injection of soap or phenol disinfectants to insertion of
foreign objects. Self-induction of abortion, by any technique in the United States, while difficult to estimate, appears to be very rare.
foreign objects. Self-induction of abortion, by any technique in the United States, while difficult to estimate, appears to be very rare.
Complications
Transcervical administration of toxic substances carries a high risk of serious complications. The most frequently reported complication of illegal abortion is retained products of conception, although the incidence of such complications is unknown. In many countries in Latin America, Africa, and Asia where elective abortion is illegal or highly restricted, the black-market or private pharmacy availability of misoprostol has increased dramatically and led to important improvements in abortion safety, because misoprostol has reduced reliance on instrumentation of the cervix.
The number of illegal abortion deaths in the United States declined dramatically during the 1970s. During the 1975 to 1979 interval, women in both extremes of the reproductive age span had higher death rates from illegal abortion than did other women. The racial discrepancy in death rate was more striking: The mortality rate for black and Hispanic women was more than 10 times greater than for white women.
As with morbidity, the likelihood of mortality is strongly related to the abortion technique. Of the 17 illegal abortion deaths from 1975 to 1979, only one followed ingestion of an abortifacient (pennyroyal oil). The other deaths were related to intrauterine techniques, ranging from injection of cleaning solutions to insertion of foreign bodies (e.g., catheters, cotton swabs, thermometers, and coat hangers). Sepsis (10 cases) and air embolism (three cases) accounted for most of these deaths. The last reported death from illegal abortion in the United States was in 2004.
Management of Septic Abortion
Most women with septic abortion respond rapidly to uterine evacuation plus broad-spectrum antibiotics. Before beginning treatment, intrauterine and blood cultures should be obtained. An upright radiograph of the abdomen may identify a residual foreign body, gas bubbles in the uterus, or free air under the diaphragm; these findings direct management.
Antibiotic administration should begin immediately upon identification of septic abortion. Coverage should include gram-positive, gram-negative, and anaerobic bacteria. Ideally, in a case of septic abortion, the patient should go directly from the emergency department to the operating room. Peak serum levels of antibiotics will be present within an hour of their administration. Further delay of uterine evacuation is unwarranted and can compromise recovery. Prompt elimination of the necrotic infected tissue is critical. Tissue obtained during curettage should quickly go for microbiologic cultures. The yield of organisms, especially anaerobes, is often higher from a tissue specimen than from a swab inserted into the uterus.
Subsequent management is governed by the response of the woman and by microbiologic findings. All women with septic abortions should be closely observed after surgery, with special attention to vital signs and urine output, to detect incipient shock. Prompt aggressive therapy is essential if septic shock develops.
Postabortal sepsis from Clostridium perfringens has become rare. When this infection occurs, however, it can be catastrophic. In the absence of hemolysis, C. perfringens bacteremia can be managed by uterine aspiration and antibiotics. In the presence of hemolysis, hysterectomy and more aggressive medical therapy may be indicated.
LEGAL ABORTION
Incidence
Legal abortion is one of the most frequently performed operations in the United States. In 2009, 784,507 induced abortions were reported. The national abortion ratio was 227 abortions per 1,000 live births in that year. The abortion rate was 15.1 abortions per 1,000 women aged 15 to 44. The total number of induced abortions and the rate of induced abortion both declined by 5% from 2008 to 2009, the most recent year for which data are available.
Demographic Characteristics
The majority of women having induced abortions in the United States tend to be young, white, single, and of low parity. Non-Hispanic white women had the lowest rate of induced abortion at 8.5/1,000 women aged 15 to 44, and non-Hispanic black women had the highest rate of induced abortion at 32.5/1,000 women aged 15 to 44. In 2009, most (64%) abortions took place at 8 weeks gestation or earlier; 92% occurred at 13 weeks gestation or earlier. Only 7% of procedures were done between 14 and 20 weeks gestation and 1.3% at more than 21 weeks. Before 1990, provision of very early (<6 weeks of gestational age) abortions was rare. Between 2000 and 2009, the percentage of abortions performed at 6 weeks or less increased by 47%. Most abortions take place safely in freestanding clinics (93%) and physician’s offices (2%). In-hospital procedures (5%) are necessary when women have a higher risk of medical or surgical complications.
Preoperative Counseling
In a recent large study, the reasons most often cited by US women for choosing abortion were that having a baby would interfere with her education, work, or ability to care for her other dependents. A majority (73%) could not afford a baby, and almost half were having relationship problems and did not want to be single mothers. Preoperative counseling should include a nonjudgmental discussion of all alternatives available, including continuing the pregnancy and adoption. Abortion procedures are reviewed and compared, including the risks, benefits, and expected experience with each method. Women choose surgical abortion to avoid the perceived involvement, awareness, pain, or emotional impact of medical abortion. Women choose early medical abortion in order to avoid surgery or anesthesia, to experience a simpler or more natural process, or in situations in which medical abortion was available sooner. Conversely, in comparison to surgical abortion, early medical abortion is associated with a longer duration of bleeding, and patients should be counseled accordingly. Contraceptive options, eligibility, and desires should also be reviewed during preoperative counseling.
Legal Considerations
It is important for clinicians to know the legal restrictions to abortion in their state. State regulations include, but are not limited to, waiting periods, counseling requirements, parental involvement for minors, ultrasound requirements, specific scripted consents, and insurance regulations.
Preoperative Medical Evaluation
The preoperative evaluation should include counseling, informed consent, a brief history, and a limited physical examination. The history taking should focus on relevant data, such as gynecologic problems (e.g., leiomyomata, uterine anomalies,
cervical stenosis) or medical problems (e.g., cardiac disease, asthma, morbid obesity) that might influence the course of the operation. Physical examination should include the heart and lungs (if anesthesia is to be used), abdomen, and pelvis. Although ultrasonography is not necessary on a routine basis, it is useful in several scenarios. Ultrasound is recommended if the size, shape, or position of the uterus is unclear as in the case of very early pregnancy, when uterine size is inconsistent with EGA per last menstrual period, and in preparation for most second-trimester cases. If ectopic pregnancy or a uterine anomaly is suspected, ultrasound should also be utilized. Ultrasound is a routine component of early medical abortions, which requires exclusion of ectopic pregnancy before use of most regimens. It is imperative to be aware of the legal requirements regarding ultrasound and abortion in a given state in order to be in compliance with these requirements when possible. Routine laboratory tests include the hematocrit (or hemoglobin) and Rh type. Additional laboratory tests may be indicated in patients with medical disorders that could influence surgical approach, anesthesia options, or the decision to perform a hospital-based procedure. Many clinicians perform a urine pregnancy test on all patients requesting abortion. Screening for chlamydia and gonorrhea need not be routine but should be targeted based on risk factors, symptoms, or examination. If bacterial vaginosis is detected preoperatively, it should be treated.
cervical stenosis) or medical problems (e.g., cardiac disease, asthma, morbid obesity) that might influence the course of the operation. Physical examination should include the heart and lungs (if anesthesia is to be used), abdomen, and pelvis. Although ultrasonography is not necessary on a routine basis, it is useful in several scenarios. Ultrasound is recommended if the size, shape, or position of the uterus is unclear as in the case of very early pregnancy, when uterine size is inconsistent with EGA per last menstrual period, and in preparation for most second-trimester cases. If ectopic pregnancy or a uterine anomaly is suspected, ultrasound should also be utilized. Ultrasound is a routine component of early medical abortions, which requires exclusion of ectopic pregnancy before use of most regimens. It is imperative to be aware of the legal requirements regarding ultrasound and abortion in a given state in order to be in compliance with these requirements when possible. Routine laboratory tests include the hematocrit (or hemoglobin) and Rh type. Additional laboratory tests may be indicated in patients with medical disorders that could influence surgical approach, anesthesia options, or the decision to perform a hospital-based procedure. Many clinicians perform a urine pregnancy test on all patients requesting abortion. Screening for chlamydia and gonorrhea need not be routine but should be targeted based on risk factors, symptoms, or examination. If bacterial vaginosis is detected preoperatively, it should be treated.
Preoperative Cervical Preparation
Osmotic dilators help to prepare the cervix for D&E abortions and can occasionally be used for earlier aspiration abortions in certain circumstances (Fig. 33.1). Osmotic dilators currently available in the United States include laminaria, Lamicel, and Dilapan. Laminaria are hygroscopic sticks of seaweed that dilate the cervix over several hours. The mode of action is not well understood, but the principal mechanism appears to be desiccation of the cervix. This drying can alter the ratio of collagen to ground substance, thus changing collagen crosslinkages. Alternatively, laminaria can alter the elaboration, release, or degradation of uterine prostaglandins. Laminaria cause the cervix to dilate the areas not in physical contact with the laminaria; whatever the mechanism, it is more complex than mere passive stretching, as previously thought. Maximum dilation is achieved at 12 and 24 hours after placement. Laminaria is made of natural resources, and there have been historical concerns of potential increased infection risk. There are no studies that show an increased risk of infection with laminaria and several studies that demonstrate the safety of and lack of increased infection with laminaria use.
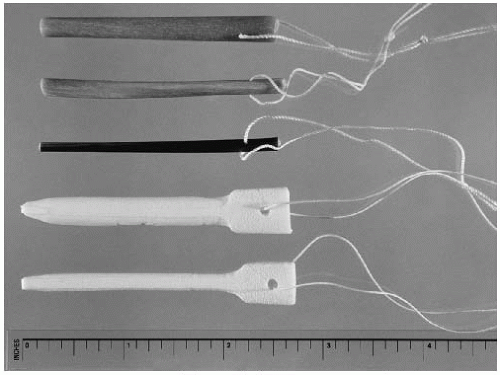 FIGURE 33.1 Osmotic dilators. Top: Laminaria of various sizes. Bottom: Lamicel in 5- and 3-mm sizes. |
Lamicel is a cylinder of polyvinyl alcohol sponge impregnated with magnesium sulfate. It works within several hours, achieving maximum dilation by 6 hours postplacement, and has the advantage of uniform size (either 5 or 3 mm diameter), assured sterility, and easy insertion and removal. Lamicel is effective as a cervical preparation agent a few hours before procedures up to 16 weeks and can be used overnight in preparation for procedures up to 17 to 18 weeks, but Lamicel is rarely used as a sole agent for cervical preparation for later procedures given the limits of its dilation capabilities. Dilapan-S is another available synthetic osmotic dilator, made of a polyacrylate-based proprietary hydrogel, and is available in 3 and 4 mm diameters and lengths of 55 and 65 mm. Dilapan-S swells rapidly demonstrating significant dilation by 2 hours. Most of the dilation is completed by 4 to 6 hours after placement, but it continues to expand up to 24 hours. Dilapan-S does have some potential problems; it shortens as it expands, prompting the recommendation to choose the longer length to ensure continuous dilation of the internal os, and it can be difficult to remove.
Osmotic dilators are convenient in an outpatient setting. Placement of any of the available brands for 3 to 4 hours before abortion frequently dilates the cervix sufficiently for abortion. Women can be sent home with laminaria in place overnight, allowing for maximal dilation. In-facility admission for observation is not necessary. Compared with use of metal dilators, use of laminaria dramatically reduces the risk of cervical injury and uterine perforation. This protection against trauma can be especially important for young teenagers with immature cervices who are at increased risk for cervical injury. Disadvantages include the cost, inconvenience, and occasional cramping involved. Instances of extramural delivery after placement of osmotic dilators are rare.
Alternatively, preoperative preparation of the cervix with misoprostol can facilitate abortion. Misoprostol, a prostaglandin E derivative, is safe, inexpensive, stable at room temperature, and effective in improving the Bishop score of the cervix. It is superior in cost efficacy and side effect profile in comparison to gemeprost. The drug can be given orally, vaginally, buccally, or sublingually. In general, misoprostol is better tolerated when given by the vaginal route versus the oral route; this probably relates to different pharmacokinetics when absorbed through the vagina versus through the gut. Both the sublingual and buccal routes demonstrate effectiveness similar to that of the vaginal route, while the side effect profile remains slightly higher than that of the vaginal route. Buccal use generally has fewer side effects than the sublingual route. Women often prefer an oral route to vaginal self-administration, but when placed in the vagina by the clinician at the end of the pelvic examination, most patients find this manner of administration acceptable. A randomized controlled trial (RCT) by Singh and colleagues suggests that misoprostol 400 µg per vagina 3 to 4 hours before the operation may be the optimal dose. Administration 1 hour before a procedure has been found not to be effective, and short intervals without proven efficacy should be discouraged. This has been reiterated by the Society of Family Planning (SFP) in the clinical guidelines for cervical preparation for procedures 14 weeks or below. In this guideline, cervical preparation with misoprostol can be considered for women who may be at increased risk of complications from cervical dilation: women in the late first trimester, adolescents, and women in whom cervical dilation is expected to be difficult due to either patient factors or provider experience. Recent data show an inferior
effect of same-day misoprostol for preoperative cervical priming in second-trimester procedures as compared with laminaria administered the day before the procedure. In the SFP guideline addressing cervical preparation for second-trimester abortions, misoprostol can be considered as an alternative to laminaria for early second-trimester cases (13 to 16 weeks) in women considered at low risk for cervical injury but should not routinely replace laminaria. After 16 weeks, misoprostol can be used in conjunction with laminaria in select cases but provides inadequate dilation alone at later gestations. Disadvantages of cervical preparation with misoprostol include the delay required, spotting and cramping, and occasional expulsion of the pregnancy in the waiting room.
effect of same-day misoprostol for preoperative cervical priming in second-trimester procedures as compared with laminaria administered the day before the procedure. In the SFP guideline addressing cervical preparation for second-trimester abortions, misoprostol can be considered as an alternative to laminaria for early second-trimester cases (13 to 16 weeks) in women considered at low risk for cervical injury but should not routinely replace laminaria. After 16 weeks, misoprostol can be used in conjunction with laminaria in select cases but provides inadequate dilation alone at later gestations. Disadvantages of cervical preparation with misoprostol include the delay required, spotting and cramping, and occasional expulsion of the pregnancy in the waiting room.
Prophylactic Antibiotics
Induced abortion patients should receive prophylactic antibiotics. A meta-analysis of the RCTs on this topic by Sawaya and colleagues showed decreased risk for postabortal endometritis for women deemed low and high risk for infection when prophylactic antibiotics were given as part of routine abortion care. The choice of antibiotic and duration of therapy are unclear. Both tetracyclines and nitroimidazoles have been shown to be effective. Doxycycline is the most commonly recommended prophylactic antibiotic in the setting of surgical abortion and has been shown to substantially reduce the risk of postabortal infection. The regimen of 100 mg of doxycycline preoperatively followed by 200 mg immediately postoperatively has been shown to decrease infection risk by 87%. Alternatives to this include azithromycin or metronidazole in prophylactic doses. However, if one administers antibiotics for more than 24 hours, prophylaxis ends and presumptive treatment of C. trachomatis begins. In high-risk populations, presumptive treatment of all patients for chlamydial infection (or bacterial vaginosis with metronidazole) may be a reasonable course of action.
Venous Thromboembolism Prophylaxis
As for EPL, there are no studies that specifically address VTE associated with surgical management of induced abortion. The Society of Gynecologic Surgeons’ systematic review concluded that, other than early ambulation, no prophylaxis is required for minor surgeries in patients without significant risk factors for VTE, as they are considered low risk for VTE. Patients having minor surgery who have two or more risk factors for thromboembolism (previous VTE, thrombophilia, malignancy, etc.) are at moderate risk, and prophylaxis can be provided via intermittent compression devices, with the addition of heparin if the risk is particularly high. Although based on limited numbers of trials of gynecologic surgery, these recommendations are feasible for the management of high-risk abortion patients who would typically be managed in an operating room.
Preoperative Preparation
If local anesthesia is to be used alone, no preoperative fasting is necessary, but if conscious sedation is a possibility, the patient should fast for at least 6 hours before the procedure. Similarly, if conscious sedation is used, the patient should be instructed to bring someone with her to escort her home. She should empty her bladder before being placed in the dorsal lithotomy position; catheterization is unnecessary. An antiseptic is applied to the cervix and vagina (e.g., povidone-iodine or chlorhexidine). Routine sterile precautions (e.g., drapes, caps, masks, and gowns) are unnecessary. The clinician should use a “no-touch” technique: He or she wears sterile gloves and does not touch those ends and portions of the sterile instruments inserted into the uterus. Use of local anesthesia predominates in the United States. Although local anesthesia does not completely relieve discomfort, it is less expensive and safer than general anesthesia. As with EPL, the benefits as well as the risks must be considered before using general anesthesia. It is a good general rule, when performing abortions under local anesthesia, to use slow, controlled movements. A support person who can talk to the patient also helps alleviate anxiety and discomfort.
Paracervical Anesthesia
To perform a PCB, the clinician should use the smallest volume of the lowest concentration of local anesthetic. Local anesthetics vary in their toxicity; for example, chloroprocaine is substantially less toxic than lidocaine. With lidocaine, a 0.5% concentration is safer than a 1% solution and is equally effective. The total dose of lidocaine should not exceed 5 mg/kg or 300 mg, whichever is less. Maximum is approximately 20 mL of 1% lidocaine or 0.25% bupivacaine for a 50-kg woman, with 10 mL being typically sufficient. Alternatively, use of local anesthesia with vasoconstrictor (e.g., epinephrine 1:200,000) slows systemic absorption of anesthetic and allows a larger total dose, although the epinephrine has additional risks and side effects. Some clinicians buffer the lidocaine solution with sodium bicarbonate to decrease burning. Vasovagal episodes occur rarely and can be treated with atropine.
Paracervical anesthesia is widely used prior to abortion procedures and has been shown to decrease pain from cervical dilation and uterine aspiration. Approaches include infiltration of the cervix at the 12-o’clock position (for application of the tenaculum) and then injection at four sites (at the 2-, 4-, 8-, and 10-o’clock positions) or two sites (at the 4- and 8-o’clock positions) at the junction of the cervix and vagina. Submucosal injection precludes inadvertent intravascular injection. Despite its widespread use, a systematic review of pain control for first-trimester abortions found insufficient evidence of a clear benefit to PCB and was not able to support its use without further well-designed RCTs. This systematic review did find evidence of decreased pain with first-trimester procedures in women who were given conscious sedation and general anesthesia or who listened to music during the procedure. In 2012, Renner et al. performed an RCT, single blinded with a sham arm to minimize confounders with adequate power to detect differences in perceived pain, and were able to demonstrate a clear decrease in pain in the PCB group and higher satisfaction overall with the abortion experience. Deep injection (3 cm) and a delay of a few minutes between injection and dilation may maximize the benefits of the PCB.
Hemorrhage Prophylaxis
Intraoperative blood loss is typically minimal with surgical management for induced abortion (as well as for EPL). Although many clinicians routinely provide misoprostol, methylergonovine maleate (methergine), or oxytocin with first- or second-trimester uterine evacuation, evidence for use of uterotonics to prevent significant blood loss is limited. For first-trimester procedures, one study has shown that intramuscular methergine significantly decreases uterine atony and need for reaspiration. However, oral methergine is unstable at room temperature and utilizing it for prophylaxis is not recommended. Prophylactic oxytocin does not significantly decrease blood loss in the first trimester. And there are no studies of misoprostol use in this setting.
In the second trimester, an RCT found that vasopressin administered with paracervical anesthesia significantly
decreases blood loss with D&E, most notably at later EGAs. As little as 4 U (0.2 mL) mixed in with the anesthetic lowers the blood loss significantly; overall, vasopressin lowers fourfold the risk of a hemorrhage of 500 mL or more. It is important to remember to administer vasopressin when opting to administer regional or general anesthesia, in which case the vasopressin can be mixed with saline and injected paracervically. The SFP guideline for postabortion hemorrhage recommends its routine use with D&E to decrease blood loss. 400 µg of misoprostol, when studied alone or with osmotic dilators for preoperative cervical preparation, was found to have little to no effect on blood loss. Larger misoprostol doses, as are typical for controlling postpartum hemorrhage, have not been studied for postabortion hemorrhage. Administration of oxytocin during D&E procedures after 20 weeks, when oxytocin receptors are present to some degree, may be helpful in preventing excess blood loss, and its use is determined by provider preference. Lack of evidence for prophylactic use does not preclude the use of uterotonics for treatment of hemorrhage (see “Immediate Complications”).
decreases blood loss with D&E, most notably at later EGAs. As little as 4 U (0.2 mL) mixed in with the anesthetic lowers the blood loss significantly; overall, vasopressin lowers fourfold the risk of a hemorrhage of 500 mL or more. It is important to remember to administer vasopressin when opting to administer regional or general anesthesia, in which case the vasopressin can be mixed with saline and injected paracervically. The SFP guideline for postabortion hemorrhage recommends its routine use with D&E to decrease blood loss. 400 µg of misoprostol, when studied alone or with osmotic dilators for preoperative cervical preparation, was found to have little to no effect on blood loss. Larger misoprostol doses, as are typical for controlling postpartum hemorrhage, have not been studied for postabortion hemorrhage. Administration of oxytocin during D&E procedures after 20 weeks, when oxytocin receptors are present to some degree, may be helpful in preventing excess blood loss, and its use is determined by provider preference. Lack of evidence for prophylactic use does not preclude the use of uterotonics for treatment of hemorrhage (see “Immediate Complications”).
Manual Vacuum Aspiration
As with EPL, sharp curettage is an obsolete method for induced abortion, supplanted by uterine aspiration, which usually involves dilation of the cervix, followed by manual or electric vacuum (suction) aspiration at 12 to 14 weeks gestation or earlier. Menstrual regulation, menstrual extraction, and minisuction




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


