FIGURE 15-1 A, B: Clinical photographs of a patient with Madelung deformity. Note the seemingly prominent ulnar head and apparent volar subluxation of the wrist on the forearm.
Madelung deformity is characterized by shortening and accentuated articular volar-ulnar tilt of the distal radius, due to abnormalities of the volar-ulnar distal radial physis. As the ulna is unaffected, it grows normally and adopts a seemingly elongated and dorsally prominent position (even though it is the radius that relatively shortens and grows abnormally volarly). In advanced or severe cases, the distal radioulnar joint (DRUJ) may be incongruent and widened, and the carpus will migrate proximally and volarly. Ultimately, this results in pain, decreased ROM (most notably supination and extension), and aesthetic differences of the wrist.
Patients will typically present between the ages of 8 and 14 years. While the typical complaint is of pain and difficulty with activities of daily living and/or sports, it is the visible aesthetic deformity that troubles many patients the most. Without a tinge of gender bias, this is what drives many adolescent females in to see us.
Physical examination will demonstrate the prominent distal ulna and relative volar subluxation of the carpus compared with the forearm. When observed closely, the hand sits out of plane of the forearm. Forearm supination and wrist extension may be limited according to the severity of the structural changes. The DRUJ may be lax or unstable. Distal hand function and elbow motion are preserved. In rare situations, patients may present with spontaneous ruptures of the extensor tendons, which may lead to the diagnosis.21,22
Radiographs will confirm the diagnosis (Figure 15-2). A number of radiographic measures have been proposed to quantify and categorize Madelung deformity.23,24 One of the challenges in radiographic evaluation is that traditional indentmeters or landmarks used in other traumatic or acquired wrist conditions cannot be utilized owing to the abnormal skeletal anatomy. McCarroll et al. have proposed radiographic measures based upon the ulnar axis, given that the ulna may be the only unaffected structure of the wrist. Ulnar tilt, lunate subsidence, lunate fossa angle, palmar tilt, and palmar carpal displacement have been described, but only ulnar tilt and lunate subsidence were found to be reliable and reproducible, with unknown correlation to wrist function or patient-rated outcomes.
Surgical Indications
Surgical treatment is recommended for persistent pain and functional limitations or progressive bony deformity in the skeletally immature patient. Patients without symptoms or with mild deformity may be observed. While aesthetics are not a primary indication for surgery, many adolescent female patients find the visible deformity troubling and may wish to proceed with surgical correction, though they do not yet have pain or functional issues. Many of these patients have sufficient enough deformity and joint incongruity that they are at risk for ulnocarpal impaction syndrome. A thorough preoperative discussion is needed regarding the relative risks and benefits of any surgical intervention, particularly if a strong motivation is the desire for a more normal-appearing wrist. If it is subtle and pain free, most will not trade the scar and surgical grief to be rid of a small bump. If it is severe, they may be better off having surgery before carpal cartilage or triangular fibrocartilage complex injuries occur.
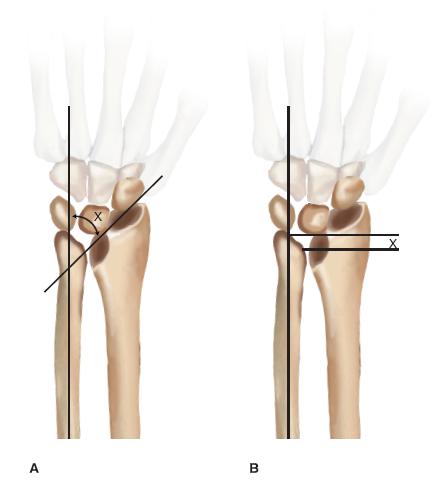
FIGURE 15-2 A, B: Schematic representations of measurements of ulnar tilt and lunate subsidence.
A number of surgical treatment strategies have been employed. In very young children with growth remaining, Vicker ligament release and physiolysis have been advocated to “untether” the distal radius and allow for spontaneous correction with growth.6 In older adolescents with established deformities and symptoms, corrective osteotomies are typically performed to (1) correct the alignment of the distal radial articular surface, (2) release any restrictive soft tissue structures, and (3) shorten the ulna to rebalance the wrist.25–33 We perform corrective dome osteotomies of the distal radius, as it is technically easy, allows for intraoperative adjustment of deformity correction, avoids the use of bulky implants, and leads to reliable bony healing. While gradual distraction lengthening of the radius or elaborate three-dimensional correction of the deformity using Ilizarov techniques have been advocated, these have not been shown to provide superior results, are more complex in their application and maintenance, and are not currently utilized at our institution.34,35 In some patients, dome osteotomy alone is not enough. Either an ulnar epiphysiodesis or ulnar shortening osteotomy is necessary depending on the age of the patient and degree of deformity.
SURGICAL PROCEDURES
Golf is deceptively simple and endlessly complicated.
—Arnold Palmer
 Physiolysis, Vicker Ligament Release
Physiolysis, Vicker Ligament Release
This is an isolated operation for the very young Madelung patient with the goal of realigning the carpus and restoring radial growth. A longitudinal incision is created overlying the flexor carpi radialis (FCR) tendon in the fashion of a classic Henry approach to the volar distal radius. The FCR tendon sheath is incised and the FCR tendon retracted ulnarly. The floor of the FCR is incised, and blunt dissection will allow for safe visualization of the pronator quadratus (PQ). The PQ is incised along its radial border, leaving a cuff of soft tissue for subsequent repair, and the pronator is swept ulnarly with careful subperiosteal elevation. Distal ulnar dissection along the volar aspect of the distal radius will allow for identification of any bipedicled PQ insertion and/or the stout Vicker ligament (in essence, usually a short radiolunate ligament), which can measure 5 to 7 mm in thickness (Figure 15-3).36 Vicker ligament is then transected, releasing the soft tissue tether. Any change in lunate position is noted on fluoroscopy. Following this, based on preoperative imaging and planning, intraoperative fluoroscopy, and direct visualization, the bony bridge in the volar-ulnar aspect of the distal radial physis is curetted, with care taken to avoid injury to the adjacent healthy physeal cartilage. Pronator muscle or fat interposition is then performed to lessen the risk of physeal bar recurrence. The pronator is repaired, and soft tissues are closed in layers. The wrist is immobilized in a short-arm cast for 2 weeks. The patient’s growth is followed closely every 6 months with radiographs. If ulnar overgrowth is recurring, early consideration for an ulnar epiphysiodesis versus later repeat radial reconstruction should occur.

FIGURE 15-3 Intraoperative photograph depicting Vicker ligament.
 Dome Osteotomy
Dome Osteotomy
In older patients with established deformity, limited remaining skeletal growth, and pain or functional limitations, a radial dome osteotomy is performed.28,29 Standard volar approach to the distal radius is performed with release of the Vicker ligament as described above. When an osteotomy is planned, circumferential periosteal elevation is required with judicious placement of small Homan or Bennett retractors. Following this, the level of the planned osteotomy is identified by direct visualization and fluoroscopic assistance, with great care being made to avoid violation of the DRUJ and radial physis, if still open (Figure 15-4). It is imperative that the dome be created concave distal; if the osteotomy is made convex distal, the prominent metaphyseal spike on the distal fragment will block radial deviation and extension of the osteotomy. (If you make the osteotomy look like a smile, not a frown, you will end up happy.) The path of the planned osteotomy is created using 0.045” K-wires to perforate the volar and/or dorsal cortex. Prior to completion of the osteotomy, a small stab incision is made overlying the radial styloid, and careful subcutaneous spreading is performed; the radial sensory nerve is almost ubiquitously beneath this incision and must be retracted and protected as do the extensor tendons and radial artery. Two indentllel or divergent smooth 0.0625″ K-wires are then placed into the radial styloid and driven to the level of the planned osteotomy. As the distal fragment will be rotated, these K-wires must be oriented in nearly a vertical or longitudinal fashion. If placed too transversely, they will miss the proximal fragment after the osteotomy is mobilized. Following this, curved osteotomes are used to connect the cortical perforations in the distal radius and complete the osteotomy. The curve of the osteotome blade is utilized to create an osteotomy plane that is curved concave distal in both the frontal and sagittal planes; this will facilitate correction of the flexion deformity as well. After the osteotomy is mobilized and the desired amount of correction is achieved, the previously placed K-wires are driven across the osteotomy, engaging the proximal ulnar cortex of the radius. Often a small spike of bone is removed to maximize correction and is used as local bone graft. Radiographs are obtained to confirm desired correction (Figure 15-5). Pins are bent and cut outside the skin. Volar skin flaps are raised, and, under direct visualization, a limited prophylactic volar forearm fasciotomy is performed. The PQ is reapproximated.
 Dome Osteotomy with Ulnar Epiphysiodesis
Dome Osteotomy with Ulnar Epiphysiodesis
If the patient is young enough to have recurrent deformity with continued ulnar growth, a distal ulnar epiphysiodesis is simultaneously performed. The physis is located by palpation and fluoroscopy. A longitudinal incision is made over the physis. Care is taken to identify and protect the ulnar sensory nerve. A 25-gauge needle is placed in the physis and the location confirmed by fluoroscopy. Either mini-incision drilling or open epiphysiodesis can be performed. It is easy to get off the mark and mainly drill or curette the metaphysis (the metaphysis actually offers less resistance than the physis). At times, the ulnar growth plate can be difficult to “kill,” and so we tend to be aggressive. Subperiosteal dissection is performed. Direct visualization of the physis while drilling and curetting is performed. A reversed block of cortical cancellous bone is inserted and confirmed by fluoroscopy. Soft tissues are then closed in the standard fashion. The limb is immobilized in a bulky, well-padded long-arm cast, which is bivalved to allow for postoperative swelling.
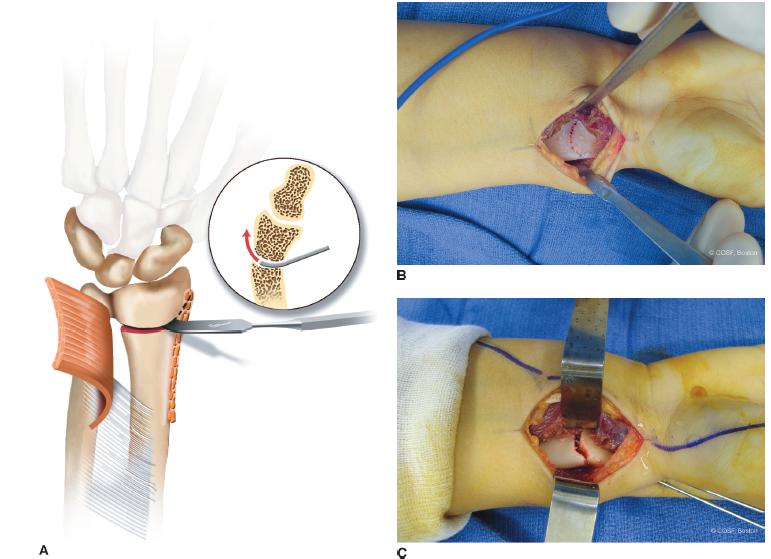
FIGURE 15-4 A: Schematic diagram of the dome osteotomy. B:After the pronator has been elevated and Vicker ligament released, the cortex is perforated with K-wires in preindenttion of a concave-distal osteotomy. C: Intraoperative appearance after completion of the osteotomy and pin fixation. Note that the distal articular fragment has been corrected in two planes, providing both radial inclination as well as extension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


