Intraosseous Infusion
Dee Hodge III
Introduction
After ensuring an adequate airway and providing adequate ventilation, assessing circulation and establishing vascular access are the next priorities in pediatric resuscitation. Traditional approaches to vascular access in children (peripheral catheters, central catheters, and cutdowns) may be difficult under any circumstances and may be almost impossible when vascular collapse is present. In one study of pediatric arrests, 24% of the patients required more than 10 minutes before vascular access was achieved (1). Intraosseous infusion is a rapid method of obtaining vascular access during critical situations. Intraosseous lines can be placed quickly and fluids and/or medications given rapidly via this route.
Intraosseous infusion is an old technique first developed during the 1930s as the preferred route of vascular access in children (2,3,4). With the advent of butterfly needles and plastic catheters during the 1950s and 1960s, the technique fell out of favor and was rarely if ever performed. The development of advanced pediatric life support interventions brought the need for a rapid, reliable method of vascular access. Intraosseous infusion has filled that need.
The technique is used in the prehospital, emergency department (ED), and hospital settings where critical intravenous access is necessary. The procedure is relatively straightforward and can be effectively performed by physicians, physician assistants, nurses, and paramedics (5,6,7). Intraosseous lines are most commonly placed in children under 3 years of age because this group usually represents the greatest challenge in obtaining vascular access; however, the technique may be used in any age group (8,9).
Anatomy and Physiology
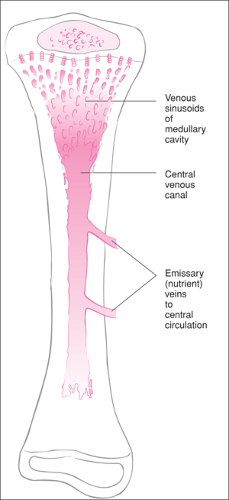
The marrow space of the long bones functions essentially as a noncollapsible vein (10). Blood flows from the venous sinusoids of the medullary cavity of the long bones to drain into a central venous canal. From the central canal, blood drains by nutrient or emissary veins into the central circulation (Fig. 21.1). Absorption from the medullary cavity of a long bone into the systemic circulation is rapid, although obviously slower than occurs with peripheral or central intravenous lines (3,11,12). Intraosseous flow rates are influenced by venous valves, venous tortuosity, venous pressure, and blood flow through the marrow cavity. The tibia and femur are the preferred sites, because the marrow cavity is well developed even in the neonatal period, and the limbs are readily accessible (13,14,15). Insertion at the proximal and distal tibia is generally easier than at the distal femur because there is less subcutaneous tissue overlying the bone (Fig. 21.2). To enter the distal femur, the needle must pass through the relatively bulky quadriceps femoris muscle. In addition, the bony cortex is thinner and more easily penetrated at the tibial sites.
Obtaining vascular access is generally more problematic for children than adults because of the small size of the vessels and the abundance of subcutaneous fat, both of which make identification of veins by palpation more difficult. With cardiopulmonary failure and other shock states, blood flow is shunted away from the periphery to supply vital organs. In the early stages of shock due to hypovolemia or pump failure, the blood pressure of a child is maintained by an increased heart rate and a marked increase in the peripheral vascular resistance (compensated shock). This is largely the result of sympathetic nervous system stimulation and circulating catecholamines. Preload is also enhanced by contraction of capacitance veins.
For the child in shock, this resulting vasoconstriction can sometimes make it impossible to obtain either peripheral or central vascular access within an acceptable time interval.
For the child in shock, this resulting vasoconstriction can sometimes make it impossible to obtain either peripheral or central vascular access within an acceptable time interval.
Indications
Intraosseous infusion is indicated for those situations in which immediate vascular access is required, most often cardiopulmonary arrest and shock (see also Chapters 19 and 73). Unlike the administration of medications, many of which can be given through the endotracheal tube or rectally, fluid volume can only be given via vascular access. Because the flow rates achieved are not sufficient to fully treat severe hypovolemic shock, this technique should not be considered to provide “definitive” access. Intraosseous access should therefore be attempted simultaneously with attempts at peripheral and central access. However, often after an initial bolus of fluid has been administered via an intraosseous line, the vessels are more prominent, and establishing peripheral or central access then becomes possible. The few absolute contraindications to this procedure include recent fractures in the bone to be used, osteogenesis imperfecta, and osteopetrosis. Cellulitis or an infected burn at the site of insertion are relative contraindications (11,13,16,17,18).
Equipment
The equipment necessary for performing intraosseous infusion is listed in Table 21.1. Intraosseous needles are manufactured by several companies, with multiple designs incorporating the main desired features. It is useful to have regular in-service training sessions or “mock codes” during which the intraosseous needle is used so that ED personnel can become familiar with these features. Needles used for the procedure should have a trocar or some method to prevent bone from occluding the needle, a short shaft to prevent bending or displacement, and a hub to fit in the palm of the operator’s hand during placement. A protective flange or a method to adjust the depth of penetration of the needle also affords some advantage (Jamshidi, Cook-Sussmane-Raszynski models). Some experts believe threaded needles (Cook-Sur-Fast model) that screw into the bone offer no significant advantage and have the potential drawback of not providing the “feel” of entering the marrow cavity (19). Newer pediatric devices include a “bone injection gun” (WaisMed, Caesarea, Israel), which employs a spring-loaded needle that is injected into the bone, as well as the EZ-IO (Vidacare, San Antonio, TX), a compact battery-powered drill with a threaded intraosseous needle. Povidone-iodine (Betadine) is needed for skin preparation, and gloves should be worn in observance of universal precautions (see Chapters 7 and 8). Lidocaine should be used for local anesthesia in awake patients.
Procedure
The most common sites used for insertion are the proximal tibia, the distal tibia, and the distal femur. The proximal tibia may be used in patients up to age 3 to 4 years. After this age, the patient’s proximal tibia is more difficult to penetrate, and therefore the distal tibia should generally be used. To locate the proximal tibia site, the operator first identifies the anterior medial surface of the tibia and palpates the tibial tuberosity. The entry site is halfway between the
anterior and posterior border of the tibia and 1 to 2 cm distal to the tibial tuberosity (20) (Fig. 21.3). At the distal tibia, the site of insertion is located just proximal to the medial malleolus halfway between the anterior and posterior borders of the bone (Fig. 21.4). The distal femur is used as a secondary site in infants or when the operator fails to enter the tibia. The location of insertion is approximately 1 cm proximal to the femoral plateau (Fig. 21.5).
anterior and posterior border of the tibia and 1 to 2 cm distal to the tibial tuberosity (20) (Fig. 21.3). At the distal tibia, the site of insertion is located just proximal to the medial malleolus halfway between the anterior and posterior borders of the bone (Fig. 21.4). The distal femur is used as a secondary site in infants or when the operator fails to enter the tibia. The location of insertion is approximately 1 cm proximal to the femoral plateau (Fig. 21.5).
 Figure 21.2 The proximal tibia is a preferred site for intraosseous needle insertion because there is little overlying soft tissue.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|