Intramuscular and Subcutaneous Injections
A. Felipe Blanco
James F. Wiley II
Introduction
Since its introduction in the second half of the 19th century, intramuscular injection has been a main route of drug delivery for the prophylaxis and treatment of disease (1). This mode of drug administration is most useful when the patient’s disease and/or the pharmacokinetic properties of the drug preclude oral dosing and an intravenous route is unavailable or unnecessary. The technique is straightforward and may be used for patients of all ages. New drugs and new applications for current drugs have increased the variety and frequency of agents delivered by this route.
Subcutaneous injection predates intramuscular injection in medical history. One of its first uses was for the prophylactic injection of cowpox to provide immunity against smallpox in the mid-18th century (1). Subcutaneous injection serves a more limited but still important role in drug delivery for pediatric care.
Anatomy and Physiology
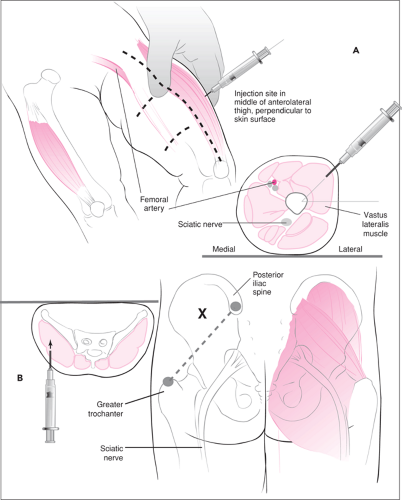
Site selection for intramuscular injection involves several considerations. The site should avoid major nerves and blood vessels. The muscle mass should be large enough to allow retention and absorption of the injected drug, and anatomic landmarks used for injection should remain consistent from patient to patient. In children, the four sites for intramuscular injection are the anterolateral thigh (vastus lateralis muscle), the ventrogluteal area (gluteus medius muscle), the upper arm (deltoid muscle), and the buttock (gluteus maximus muscle) (Fig. 120.1). Site preference depends on age and nutrition status of the child, as shown in Table 120.1 (2). Malnourished children may have decreased muscle mass at one or more injection sites and therefore require special consideration.
Intramuscular injection creates a depot for drug absorption from the muscle into the systemic circulation. However, this route does not always ensure rapid or complete bioavailability. Absorption depends on the lipophilic properties and concentration of the drug, on the total surface area available, and on blood flow at the injection site. Absorption varies by injection site: it is most rapid from the deltoid muscle, slowest from the gluteal muscles, and intermediate from the vastus lateralis muscle (3). Injected drug absorption increases with exercise and decreases or stops with circulatory disturbances such as shock, hypotension, congestive heart failure, and myxedema.
Intramuscular injection presents the delivered drug as a potential antigen to macrophages and T cells within the muscle. Furthermore, intramuscular injection causes tissue injury, which leads to a migration of many inflammatory cells of different types to the area. As a result, an amnestic response may occur within T lymphocytes, leading to a type IV immunologic response after re-exposure to the drug. Thus, intramuscular injection may predispose an individual to hypersensitivity and allergic reactions to the drugs received.
Intramuscular injection causes direct tissue injury and pain. Muscle enzymes (aspartate transaminase, creatine phosphokinase) are elevated by injection. This is especially true when large volumes are used, when the drug is intrinsically irritating, and when the pH of the injectant is far from physiologic range (3). Inadvertent injection into an artery or vein compounds the potential for tissue injury. Arterial injection may cause subsequent vasospasm and potential drug toxicity in the distal tissues. Arterial or venous injection also carries the risk of untoward systemic effects with certain agents, such as
lidocaine. Table 120.2 lists drugs commonly injected via the intramuscular route and their potential for tissue injury.
lidocaine. Table 120.2 lists drugs commonly injected via the intramuscular route and their potential for tissue injury.
TABLE 120.1 Preferred Injection Sites | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
The goal of subcutaneous injection is to deliver the drug into the adipose tissue, which lies below the dermis layer of the skin and above the muscle layer. The optimal sites for this
task are the upper lateral shoulder, the anterior thighs, and the abdomen, because they have a relative abundance of fat and few surface veins. The adipose layer has a smaller blood supply relative to the muscle layer; therefore, drug absorption after subcutaneous injection is less consistent and slower than after intramuscular injection. Drugs given subcutaneously, such as growth hormone and insulin, are best absorbed from the abdomen, followed by the arms, thighs, and buttocks (4,5). The potential for allergic reactions and tissue injury discussed above for intramuscular injections also exists, although to a lesser extent, in the case of subcutaneous injections. Table 120.2 also lists the agents commonly delivered by subcutaneous injection.
task are the upper lateral shoulder, the anterior thighs, and the abdomen, because they have a relative abundance of fat and few surface veins. The adipose layer has a smaller blood supply relative to the muscle layer; therefore, drug absorption after subcutaneous injection is less consistent and slower than after intramuscular injection. Drugs given subcutaneously, such as growth hormone and insulin, are best absorbed from the abdomen, followed by the arms, thighs, and buttocks (4,5). The potential for allergic reactions and tissue injury discussed above for intramuscular injections also exists, although to a lesser extent, in the case of subcutaneous injections. Table 120.2 also lists the agents commonly delivered by subcutaneous injection.
TABLE 120.2 Drugs Frequently Used for Intramuscular or Subcutaneous Injection | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Indications
Intramuscular Injection
Common reasons for using intramuscular injections in the ambulatory setting include immunization, infectious prophylaxis, treatment of existing infection, pain management, and sedation (Table 120.2). The need for intramuscular epinephrine to treat anaphylaxis and the need for intramuscular anticonvulsants for prolonged seizures in patients in whom intravenous access cannot be obtained are two emergency indications for intramuscular injection (6,7). This route of drug delivery ensures compliance and avoids first-pass metabolism. With some infectious diseases (e.g., streptococcal pharyngitis and certain gonococcal infections), a single intramuscular shot of antibiotic has proven as efficacious as a multiple-day, orally administered drug regimen (8,9). Potential advantages of intramuscular drug administration, however, should be weighed against the pain of the procedure and potential risks of local injury and allergic reaction when used in the outpatient setting. Intramuscular injections should be avoided in patients with bleeding dyscrasias and circulatory instability. Hematoma formation and hemorrhage can cause extensive local tissue damage in patients with hemophilia, thrombocytopenia, von Willebrand disease, disseminated intravascular coagulation, and other clotting disorders. In addition, patients in shock do not absorb drugs well from intramuscular injections and may suffer complications from erratic drug delivery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree