Injury Prevention
Karen S. Frush
Department of Pediatrics, Duke University Hospital and Health System, Durham, North Carolina 27710.
CASE SCENARIOS
Case 1
A 2-month-old infant, held in her mother’s lap, was in the front seat of an SUV stopped at an intersection. Paramedics in an ambulance at the same intersection report that a cement truck, traveling at a moderate rate of speed, struck the SUV on the front driver side. The infant was ejected approximately 50 feet from the car and was unresponsive when paramedics reached her. Resuscitation efforts were immediately initiated, and the infant was transported directly to a Level 1 Trauma Center, 5 miles away. She required intubation for depressed mental status and airway protection. Her evaluation revealed a severe closed head injury, a grade II liver laceration, and a femur fracture of the right leg. After stabilization in the emergency department (ED), she was admitted to the Pediatric Critical Care Unit for close observation and care. She was extubated 4 days later, but required subsequent placement of a gastrostomy tube and extensive follow-up and rehabilitation.
Case 2
A 2-month-old infant was restrained in an appropriate child restraint in the back seat of a Jeep SUV stopped at an intersection. An emergency medical technician near the scene reported that the SUV was struck on the driver’s side by a dump truck, traveling at a moderate rate of speed. The infant remained in the child restraint in the back seat, and was awake and crying when first responders arrived. He was transported to a Level 1 Trauma Center, 5 miles away, and was evaluated by the Pediatric Trauma Service. He was not found to have any significant injuries and was discharged home with his mother after a period of observation.
These two scenarios represent actual cases presenting to a Level I Trauma Center within 1 week. The cases involve infants of the same age, traveling in similar vehicles, involved in a similar type of crash. The same emergency medical services (EMS) agency responded immediately to both crash scenes. The infants were transported to a Level I Trauma Center where the same pediatric trauma team responded. Despite the similarities, the outcomes of the infants were very different. The key to this difference lies in the appropriate use of a child restraint at the time of the crash. These actual scenarios clearly demonstrate that the best treatment of trauma is to prevent it. Even with immediate care at the scene, advanced medical technology, and direct access to comprehensive trauma care, the effect of some injuries is so severe that it cannot be reversed once it occurs.
Over the past several decades, much progress has been made in the management and prevention of childhood disease. New immunizations have led to a decreased number of illnesses in young children; newer antibiotics have led to improved survival of children with immunodeficiency disorders and severe infection; and public health initiatives have led to increased screening efforts for common childhood problems, such as lead exposure, hemoglobinopathies, elevated cholesterol or lipid levels, and various metabolic disorders.
As the death rate due to childhood disease and infections has fallen, the problem of childhood injury has become more clear. Injuries are the leading cause of death and disability among children ages 1 to 19 years and cost society billions of dollars each year (1). Many injuries and injury-related deaths can be prevented.
As child advocates, physicians and other health care professionals can help reduce the number of childhood injuries through education, advocacy, policy, and research. This chapter describes the epidemiology of childhood injury and discusses successful approaches to injury prevention programs.
THE PROBLEM OF CHILDHOOD INJURY
Injury is the leading cause of death in children and young adults in the United States, regardless of gender, race, or economic status (2). In 1999, more than 1,500 children under the age of 14 years died from unintentional injuries, accounting for more deaths in this age group than all childhood diseases combined. In that same year, more than 13,500 adolescents and young adults in the 15- to 24-year-old age group died from unintentional injuries (2). For every injury death, an estimated 18 children require hospital admission, and 233 more visit an ED as a result of injuries (3).
Although the childhood injury death rate has been declining since the mid-1980s (Fig. 21-1), injuries continue to be a major public health problem and a great financial burden to society. The federal government pays approximately $12.6 billion each year in injury-related medical costs (i.e., ambulance, EMS, physicians, hospital, rehabilitation, and related treatment costs) and about $18.4 billion in death and disability payments (2). Even greater than these direct costs are the indirect costs of injury-related morbidity and mortality, described as “work loss cost” or “loss of productive years.” Work loss cost is the sum of the lifetime loss due to permanent disability, plus the cost due to temporary disability (4). This includes the victim’s lost wages and the value of lost household work, as well as the work loss of family and friends who care for the injured victim. The total financial cost of injuries in the United States is estimated to be more than $224 billion each year (2).
As researchers and health care providers have gained a better understanding of the magnitude of the problem of childhood injury, they have begun to stress the important difference between “injuries” and “accidents.” In the past, physicians commonly referred to injuries as “accidents” (i.e., a 2-month-old infant involved in a motor vehicle accident). Accidents are rare events that occur at random; these events are largely unforeseen, unpredictable, and unavoidable. An injury, in contrast, is “damage or harm to the body resulting in impairment or destruction of health” (5). Injuries are not random; they are predictable events that can be studied and analyzed. Specific factors can be identified that may increase the likelihood of injury (risk factors) or decrease the likelihood of injury (protective factors). Once these factors are identified, effective strategies can be developed to help avoid or prevent injuries.
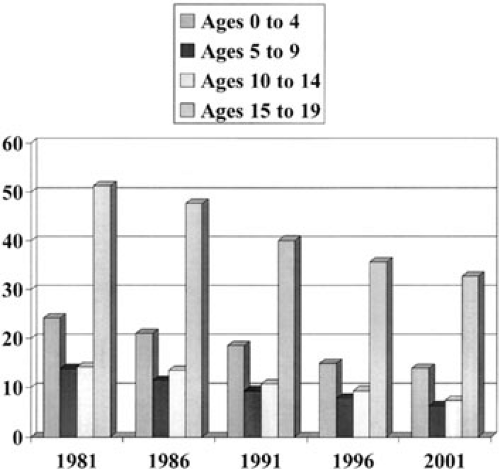 FIGURE 21-1. Trends in unintentional injury deaths by age group, 1981 to 2001. (From: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, U.S. Injury Mortality Statistics.) http://www.webappa.cdc.gov/cgibin/broker.exe |
The Haddon Matrix provides a conceptual model that can be used to analyze an injury event. Dr. William Haddon, a pediatrician who was appointed the first Director of the National Highway Safety Bureau in 1966, (6) identified three components of an injury event: the host, the agent, and the environment. The host is the person who is injured. The agent is the form of energy delivered to the host, such as kinetic, thermal, chemical, or electrical. The environment is the setting where the agent meets the host, and refers to both the physical and sociocultural setting. Environmental factors can cause the event or influence the event, such as an unfenced swimming pool or a toxin stored in an unmarked bottle or container.
In the Haddon Matrix, the three components of an injury event are considered at three different temporal phases: the preevent period, the event itself, and the postperiod event (7).
Opportunities to prevent morbidity and mortality due to an injury could be present before, during, and following the event. Table 21-1 illustrates the Haddon Matrix using pedestrian injuries as an example (6).
Epidemiology of Childhood Injury
Although injuries affect everyone, there is considerable variation in the rate of injuries among children, depending on their age group, racial or ethnic group, gender, socioeconomic group, and geographic area. Overall, rates are
highest among adolescents (ages 15 to 19), males, children from impoverished families, and minorities (6). Motor vehicle-related injuries are the leading cause of death across all age groups, including motor vehicle occupant and pedestrian events. Major causative factors in motor vehicle-related deaths and injuries include lack of street safety, lack of use of appropriate safety restraints, improper use of restraint devices, and use of alcohol. Other leading causes of injury-related death among children 1 to 19 years old include drowning and pedestrian injuries, followed by fires, bicycle crashes, falls, firearms, choking, and poisoning (6).
highest among adolescents (ages 15 to 19), males, children from impoverished families, and minorities (6). Motor vehicle-related injuries are the leading cause of death across all age groups, including motor vehicle occupant and pedestrian events. Major causative factors in motor vehicle-related deaths and injuries include lack of street safety, lack of use of appropriate safety restraints, improper use of restraint devices, and use of alcohol. Other leading causes of injury-related death among children 1 to 19 years old include drowning and pedestrian injuries, followed by fires, bicycle crashes, falls, firearms, choking, and poisoning (6).
TABLE 21-1 Haddon’s Matrix: Pedestrian Injury Example. | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||
Falls are the leading cause of nonfatal injuries in children. Falls, along with motor vehicle crashes and poisoning, are leading causes of hospitalization, whereas the most common causes of injury-related visits to the ED include falls, being struck against a person or object, motor vehicle crashes, and lacerations (6).
INFANTS AND YOUNG CHILDREN
Nearly one-half of the children ages 1 to 4 years who are killed in motor vehicle crashes each year are not restrained while riding in the car (8), despite the fact that all 50 states currently have laws mandating the use of child safety seats. Proper safety restraints are estimated to reduce the risk of death by approximately 70% in infants and 55% in toddlers (8) (Table 21-3). Recent studies suggest that use of safety restraints is as high as 85% in infants and 60% in young toddlers, (9) but many times restraints are used incorrectly (10). Information provided through the National SAFEKIDs Campaign and the National Highway Traffic Safety Administration suggests a misuse rate as high as 80% to 90% (11,12).
TABLE 21-2 Modifiable Factors in Different Phases of an Injury. | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


